Small intestine
The small intestine, also small bowel, is a relatively well-behaved piece of machinery from the perspective of pathology. It is uncommonly affected by malignancies, relative to its length when compared to the colon and rectum.
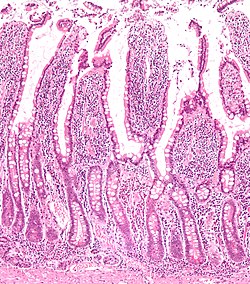
Normal small bowel
- AKA normal small intestine.
Anatomy
Consists of three segments:
- Duodenum - can be divided into four parts.
- Jejunum.
- Ileum.
The later two parts keep general surgeons awake at night (quite literally) 'cause they get obstructed and need urgent operations.
Length
- Normal length of small bowel = 3-8 metres.[1]
"Short":
- Less than 200 cm = short bowel syndrome.[2][3]
- Less than 100 cm usu. requires parenteral nutrition.[4]
Histology
The Gastrointestinal pathology article covers basic histology of the GI tract.
Immunohistochemistry
- Normal small intestine is CK20 +ve... while adenocarcinoma of the small bowel may be CK20 -ve.[5]
Sign out
SMALL BOWEL, BIOPSY: - SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH MORPHOLOGICAL BENIGN LYMPHOID AGGREGATES, NO SIGNIFICANT PATHOLOGY.
The segments
Duodenum
The duodenum is often biopsied by gastroenterologists.
Common reasons for biopsy:
- Suspected giardia.
- Suspected celiac sprue.
- Is this cancer?
- Looks normal... want to dot the i's and cross the t's.
Jejunum
- Uncommonly seen by pathologists.
- May be seen in the context of a resection done for a bowel obstruction.
Ileum
- This is seen occasionally -- often in the context of IBD and more specifically Crohn's disease.
- Crohn's disease andulcerative colitis are discussed in their respective articles.
Specific conditions
Small bowel obstruction
- Abbreviated SBO.
- This section gives an overview of SBOs. Its primary focus is benign causes of SBO that have nonspecific pathologic findings. Specific causes definitively identified by pathology, e.g. adenocarcinoma, are dealt with separately.
General
- Radiologic/clinical diagnosis.
The usual causes of bowel obstruction (large & small) are (mnemonic) SHAVING:
- Adhesions > hernias > neoplasms.
In the context of bowel obstructions and IBD, pathologists often see resected stomas (that were put in place emergently). These specimens are usually fairly straight forward.
Radiology
- Air-fluid levels.
Gross
- +/-Adhesions.
- +/-Bowel contorted.
- +/-Luminal narrowing +/-proximal dilation.
- +/-Serosal exudate.
- Suggestive of perforation.
Microscopic
Features:
- +/-Adhesions (serosal).
- Dense fibrous tissue replaces the adipose tissue.
- +/-Increased vascularity.
- +/-Submucosal fibrosis.
- +/-Serositis - seen in small bowel perforation.
- +/-Foreign body-type granuloma - due to previous surgical intervention.
DDx:
- Small bowel adenocarcinoma - most important differential diagnosis.
- Metastatic adenocarcinoma - classically on the serosal aspect.
- Signet ring cell carcinoma.
Sign out
SMALL BOWEL, RESECTION: - SMALL BOWEL WITH FIBROUS ADHESIONS (EXTENSIVE) ASSOCIATED WITH FOCAL LUMINAL NARROWING. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
SMALL BOWEL, RESECTION: - SMALL BOWEL WITH FIBROUS ADHESIONS (EXTENSIVE), FOCAL LUMINAL NARROWING AND A FOREIGN BODY-TYPE GRANULOMA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ischemic changes
SMALL BOWEL, RESECTION: - SMALL BOWEL WITH ISCHEMIC CHANGES, FIBROUS ADHESIONS, FOCAL SEROSITIS AND MURAL MICROABSCESS FORMATION. - NO SIGNIFICANT VASCULAR PATHOLOGY APPARENT. - NEGATIVE FOR MALIGNANCY.
Small bowel neoplasms
- Adenocarcinoma - like colonic.
- Adenosquamous carcinoma.
- Neuroendocrine tumour.
- GIST.
- Schwannoma.
- Classically have a peripheral lymphoid cuff.[8]
Mechanical small bowel perforation
Ileal nodular lymphoid hyperplasia
- AKA nodular lymphoid hyperplasia of the terminal ileum.
General
- An uncommon diagnosis.
- May be associated with hypogammaglobulinemia.[9]
Gross
- Mucosal nodularity.
Microscopic
Features:
- Lymphoid nodules +/- germinal centre formation.
Note:
- Tingible body macrophages suggest an aggregate is benign.
DDx:
- MALT lymphoma.
- Mantle cell lymphoma.
- Other lymphomas.
IHC
- CD20 and CD3 - mixed population of lymphocytes.
- CD23 - follicular dendritic cells.
- Cyclin D1 -ve.
Note:
- IHC should be used if there is:
- Clinical suspicion.
- Histologic suspicion - either:
- Sheets of lymphocytes without apparent germinal centre formation in a larger area (~ 2 mm).
- Lymphoepithelial lesions.
Sign out
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH LYMPHOID NODULES WITH GERMINAL CENTRE FORMATION -- NO SIGNIFICANT PATHOLOGY. - NEGATIVE FOR ILEITIS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH LYMPHOID HYPERPLASIA -- NO SIGNIFICANT PATHOLOGY.
Micro
The sections show small bowel mucosa with lymphoid hyperplasia.
Immunostains for CD3 and CD20 show a mixed population of lymphocytes. A CD23 immunostain shows follicular dendritic cell networks. A cyclin D1 immunostain is negative.
Alternate
Immunostains for CD3 and CD20 show a mixed population of lymphocytes, with CD20 cells predominating. A cyclin D1 immunostain is negative. A CD23 immunostain shows follicular dendritic cell networks.
Multiple lymphomatous polyposis
- Abbreviated MLP.
- AKA lymphomatous polyposis.
General
- MLP is classically due to mantle cell lymphoma.[10]
- May be due to other lymphomas, e.g. follicular lymphoma.[11]
Microscopic
Features:
- Lymphoid nodules consisting of (small) atypical lymphocytes with an abnormal architecture.
IHC
See small cell lymphomas.
Small bowel diaphragm disease
- AKA diaphragm disease.
General
Microscopic
Features:[12]
- Focal submucosal fibrosis.
- +/-Distortion of adjacent muscularis propria.
- +/-Adjacent mucosal erosions/granulation tissue.
DDx:
Meckel diverticulum
General
- Most common congenital anomaly of the gastrointestinal tract.[13]
- Remnant of the omphalomesenteric duct - a connection of the yolk sac and midgut.
The rule of 2s:
- 2 feet from the terminal ileum
- 2% of the population
- 2% symptomatic.
- 2 inches long.
- 2 year old.
- 2 types of epithelium - gastric and pancreatic.
Main clinical DDx of a symptomatic Meckel diverticulum:
Gross
- Antimesenteric attachement, i.e. a Meckel's diverticulum hangs off the side opposite of the mesentery.
Image:
Microscopic
Features:[13]
- Small bowel mucosa.
- +/-Gastric mucosa:
- Foveolar epithelium: champagne flute-like columnar epithelium.
- Oxyntic mucosa: parietal cells (pink) and chief cells (purple).
- +/-Pancreatic epithelium:
- Pancreatic acini.
Images:
- Gastric foveolar epithelium in a MD (radiographics.rsna.org).
- Gastric glands in a MD (radiographics.rsna.org).
- Pancreatic glands in a MD (radiographics.rsna.org).
Ischemic enteritis
General
- Typically elderly and due to atherosclerosis.
- Rare.
- High mortality.[14]
- May occur together with ischemia of the colon, i.e. ischemic colitis, in which case it is known as ischemic enterocolitis.
Etiologies:
- Atherosclerosis.
- Vasculitis.
- Embolism.
- Thrombosis.
Microscopic
Features:
- See ischemic colitis.
DDx:
- Infection.
- Crohn's disease.
- Radiation changes.
- Drugs/toxins.
Weird stuff
Autoimmune enteropathy
- Abbreviated as AIE.
General
- Considered a pediatric disease.
- Super rare in adults - there are only ~11 reported cases in the literature.[15]
- May be a component of the IPEX syndrome.[16]
Diagnosis is clinico-pathologic:[15]
- Intact immune system.
- Autoantibodies.
- Anti-enterocyte antibody.
- Anti-goblet antibody.
- Lack of response to gluten-free diet.
Microscopic
Features:[15]
- +/-Loss of goblet cells.
- +/-Loss of paneth cells.
- Villous blunting.
DDx:
See also
References
- ↑ Nightingale, JM.. "Management of patients with a short bowel.". Nutrition 15 (7-8): 633-7. PMID 10422101.
- ↑ Donohoe, CL.; Reynolds, JV. (Oct 2010). "Short bowel syndrome.". Surgeon 8 (5): 270-9. doi:10.1016/j.surge.2010.06.004. PMID 20709285.
- ↑ Matarese, LE.; O'Keefe, SJ.; Kandil, HM.; Bond, G.; Costa, G.; Abu-Elmagd, K. (Oct 2005). "Short bowel syndrome: clinical guidelines for nutrition management.". Nutr Clin Pract 20 (5): 493-502. PMID 16207689.
- ↑ Sundaram, A.; Koutkia, P.; Apovian, CM. (Mar 2002). "Nutritional management of short bowel syndrome in adults.". J Clin Gastroenterol 34 (3): 207-20. PMID 11873098.
- ↑ Chen ZM, Wang HL (October 2004). "Alteration of cytokeratin 7 and cytokeratin 20 expression profile is uniquely associated with tumorigenesis of primary adenocarcinoma of the small intestine". Am. J. Surg. Pathol. 28 (10): 1352–9. PMID 15371952.
- ↑ URL: http://www.emedicine.com/EMERG/topic66.htm. Accessed on: 19 April 2011.
- ↑ Greenwald, J.; Heng, M. (2007). Toronto Notes for Medical Students 2007 (2007 ed.). The Toronto Notes Inc. for Medical Students Inc.. pp. GS21. ISBN 978-0968592878.
- ↑ Levy AD, Quiles AM, Miettinen M, Sobin LH (March 2005). "Gastrointestinal schwannomas: CT features with clinicopathologic correlation". AJR Am J Roentgenol 184 (3): 797–802. PMID 15728600. http://www.ajronline.org/cgi/content/full/184/3/797.
- ↑ Yamaue H, Tanimura H, Ishimoto K, Morikawa Y, Kakudo K (1996). "Nodular lymphoid hyperplasia of the terminal ileum: report of a case and the findings of an immunological analysis". Surg. Today 26 (6): 431-4. PMID 8782302.
- ↑ Ruskoné-Fourmestraux, A.; Audouin, J. (Feb 2010). "Primary gastrointestinal tract mantle cell lymphoma as multiple lymphomatous polyposis.". Best Pract Res Clin Gastroenterol 24 (1): 35-42. doi:10.1016/j.bpg.2009.12.001. PMID 20206107.
- ↑ URL: http://www.pathmax.com/gilymph.html. Accessed on: 1 April 2012.
- ↑ 12.0 12.1 McCune KH, Allen D, Cranley B (October 1992). "Small bowel diaphragm disease--strictures associated with non-steroidal anti-inflammatory drugs". Ulster Med J 61 (2): 182–4. PMC 2448949. PMID 1481311. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2448949/.
- ↑ 13.0 13.1 Levy, AD.; Hobbs, CM.. "From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic Correlation.". Radiographics 24 (2): 565-87. doi:10.1148/rg.242035187. PMID 15026601.
- ↑ Nakase, H. (Jul 2008). "[Ischemic enteritis].". Nihon Rinsho 66 (7): 1330-4. PMID 18616124.
- ↑ 15.0 15.1 15.2 Akram, S.; Murray, JA.; Pardi, DS.; Alexander, GL.; Schaffner, JA.; Russo, PA.; Abraham, SC. (Nov 2007). "Adult autoimmune enteropathy: Mayo Clinic Rochester experience.". Clin Gastroenterol Hepatol 5 (11): 1282-90; quiz 1245. doi:10.1016/j.cgh.2007.05.013. PMC 2128725. PMID 17683994. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2128725/.
- ↑ Gentile, NM.; Murray, JA.; Pardi, DS. (Oct 2012). "Autoimmune enteropathy: a review and update of clinical management.". Curr Gastroenterol Rep 14 (5): 380-5. doi:10.1007/s11894-012-0276-2. PMID 22810979.