Steatohepatitis
| Steatohepatitis | |
|---|---|
| Diagnosis in short | |
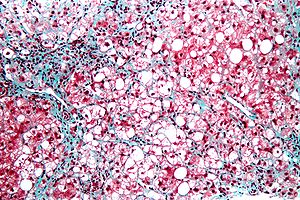 Steatohepatitis. Trichrome stain. | |
|
| |
| LM | steatosis (usually macrovesicular); hepatocyte injury -- ballooning degeneration (key feature), Mallory bodies; portal bridging (late stage) |
| Subtypes | by etiology (classically): ASH, NASH -- all almost histologically identical |
| LM DDx | steatosis, Wilson disease, hepatitis C, drug-induced liver disease |
| Gross | pale/yellowish, often enlarged |
| Site | liver - see medical liver disease |
|
| |
| Associated Dx | obesity, alcohol abuse |
| Prevalence | common |
| Prognosis | dependent on underlying cause |
| Treatment | dependent on underlying cause |
Steatohepatitis is a fatty change of the liver (steaosis) with (histologic) evidence of liver injury. It can be due to a number of different causes.
General
- Steatohepatitis is a label for a set of histopathologic findings.
- Fat accumulation (in hepatocytes) alone is liver steatosis.
- It may be a pattern seen in drug toxicity, e.g. methotrexate toxicity.[1]
Etiology:
- Alcohol = alcoholic steatohepatitis (ASH).
- Not alcohol = non-alcoholic steatohepatitis (NASH).
- Drug/toxin.[2]
Notes:
- Pathologists can comment on the etiology; however, the histomorphology is not distinctive. In other words, ASH and NASH are clinical diagnoses.
- Steatohepatitis is a misnomer. It is not an -itis; inflammation is not the (predominant) pathologic process.
Microscopic
Features:
- Steatosis (usually macrovesicular) - key feature.
- If less than 10% ... consider alt. diagnosis/disease process.
- Hepatocyte injury:
- Ballooning degeneration - key feature.[3]
- Mallory bodies.
- Mallory body wannabes: "occasional cytoplasmic clumping".
- +/-Chicken-wire perisinusoidal fibrosis +/- zone III (centrilobular) fibrosis (early).
- Late-stage disease - portal bridging.[4]
DDx:
- Steatosis - lacks ballooning degeneration.
- Wilson disease.
- Hepatitis C.
- Drug-induced liver disease.
Grading steatohepatitis
Grading inflammation:[5]
- Grade 1 - steatosis, occasional ballooning degeneration, PMNs.
- Grade 2 - obvious ballooning, obvious PMNs, chronic inflammation.
- Grade 3 - panacinar steatosis.
Five cases are provisioned with photogrphs, described.
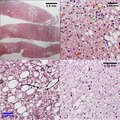
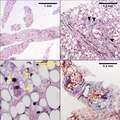
Necroinflammatory grades Brunt 1, NAH 3. Fibrosis stage 0. About 25% of the liver shows steatosis (UL), not pan-acinar. Only rarely identified were either ballooned hepatocytes or inflammatory aggregates. UR shows more macrovesicular (blue arrowhead) than microvesicular (yellow arrowhead) steatosis, with occasional neutrophils in acini ( tip of green arrowhead, benath inflammatory aggregate, with tuft of material in ballooned hepatocyte at base of green arrow), and many glycogenated nuclei (magenta arrowhead). Additional evidence of hepatocellular damage is seen on the reticulin with focal zone III collapse (LL, blue arrowhead) and on the PAS with diastase stain with PAS-D Kupffer cells (LR black arrowheads) Original oculars. UL 4X. UR 40X, LL 40X, LR 40X
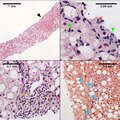
Necroinflammatory grades Brunt 2, NAH 6. Fibrosis stage 1. About half the hepatocytes show macrovesicular steatosis (UL), with sparing of part of the acinus (UL, Black arrowhead), Lipogranulomas, acomar inflammatory collections, mostly macrophages, about steatosis/ballooning degeneration afflicted hepatocytes or adjacent to them (UR, green arrowheads) are present.Tufts/flocks of ballooning degeneration are readily found (LL, magenta arrowheads). Mild to moderate mononuclear inflammation of portal triads does not exclude steatohepatitis (LL, yellow arrowheads). Trichrome displays the blue thin lines that separate hepatocytes in stage 1 fibrosis (LR blue arrowheads). Original oculars UL 4X, UR 40X (higher pixel photograph), LL 40X , LR 10X
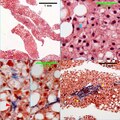
Necroinflammatory grades Brunt 1, NAH 3. Fibrosis stage 2. Overall, about a third of the biopsy shows mostly macrovesicular steatosis (UL). Rare inflammatory aggregates and ballooned hepatocytes were seen, but occasional linear/ropy Mallory hyalin was seen (UR blue arrowhead). Although trichrome can highlight Mallory hyalin (LL red arrowhead), the remainder of the image shows other cytoplasmic collections will also stain blue/blue-grey. The trichrome stain also showed peri-portal fibrosis (LR, yellow arrowheads). Original oculars UL 4X, UR 40X (higher pixel photograph), LL 40X (higher pixel photograph), LR 20X
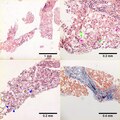
Necroinflammatory grades Brunt 2, NAH 7. Fibrosis stage 3. About 70% of hepatocytes are afflicted by steatosis (UL). Many ballooned cells are present, with their residual tufts/flocks (UR green arrowheads) demarcating multiple cells having formed apparent fat cysts. Two-three acinar inflammatory foci (UL magenta arrowheads) can be seen in a 20X field. The disorder is emphasized by a reticulin stain which shows the thin black lines (LL blue arrowheads) forming acinar circles, heading in irregular directions, and coming closer and separating from adjacent lines with great variability. The trichrome stain (RL) shows a bridge. Original oculars UL 4X, UR 20X, LL 20X, LR 10X
Necroinflammatory grades Brunt 3, NAH 8. Fibrosis stage 4. Steatosis is pan-acinar (UL). Acinar inflammatory aggregates More than 4 inflammatory aggregates are seen in a 20X field (UR black arrowheads). Many cells show ballooning degeneration, with tufts/flocks of material cytoplasm (LL yellow arrowheads) Trichrome limns regenerative nodules (LR magenta arrowheads). Original oculars UL 4X, UR 20X, LL 40X (higher pixel photograph), LR 10X
Image
See also
References
- ↑ MG. 22 September 2009.
- ↑ Farrell, GC. (2002). "Drugs and steatohepatitis.". Semin Liver Dis 22 (2): 185-94. doi:10.1055/s-2002-30106. PMID 12016549.
- ↑ Brunt, EM. (2001). "Nonalcoholic steatohepatitis: definition and pathology.". Semin Liver Dis 21 (1): 3-16. PMID 11296695.
- ↑ Gramlich, T.; Kleiner, DE.; McCullough, AJ.; Matteoni, CA.; Boparai, N.; Younossi, ZM. (Feb 2004). "Pathologic features associated with fibrosis in nonalcoholic fatty liver disease.". Hum Pathol 35 (2): 196-9. PMID 14991537.
- ↑ Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Am J Gastroenterol. 1999 Sep;94(9):2467-74. PMID 10484010.