Pleomorphic adenoma
| Pleomorphic adenoma | |
|---|---|
| Diagnosis in short | |
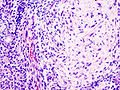
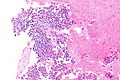
 Pleomorphic adenoma. H&E stain. (WC/KGH) | |
|
| |
| LM | proliferation of myoepithelium in a mesenchymal stroma +/- epithelium; cells in ducts = epithelial, cells not in ducts = myoepithelial, mesenchymal stroma = chondroid stroma (specific), others (require epithelium) mucochondroid, hyalinized, osseous, fatty, myxoid |
| LM DDx | myoepithelioma, carcinoma ex pleomorphic adenoma, epithelial-myoepithelial carcinoma, polymorphous low-grade adenocarcinoma, adenoid cystic carcinoma |
| IHC | S-100 +ve, SMA +ve, GFAP +ve |
| Site | salivary gland - usu. parotid gland, oral cavity, other sites |
|
| |
| Signs | mass lesion |
| Prevalence | common |
| Prognosis | benign |
| Clin. DDx | other salivary gland tumours |
Pleomorphic adenoma, abbreviated PA, is a very common benign salivary gland tumour.
General
Features:
- Very common - approx. 60% of parotid gland tumours.[1]
- May transform into a malignant tumour.
- Other benign salivary gland tumours do not do this.
- Only benign childhood salivary gland tumour of significance.
Weinreb's dictums
- Most common salivary tumour in all age groups.
- Seen in all sites (unlike other benign tumours).
- Recurrence and malignancy risk (unlike other benign salivary gland tumours).
- Any part of a tumour that looks like PA makes it a PA.
Gross
- May have cartilaginous appearance.
- Typically well-circumscribed.
Image:
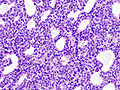
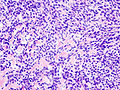
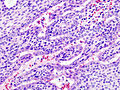
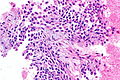
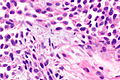
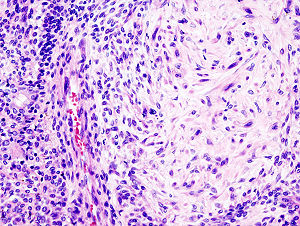
Microscopic
Features:[1]
- Proliferation of myoepithelium and epithelium (ductal cells) in mesenchymal stroma.
- Cells in ducts = epithelial.
- Cells not in ducts = myoepithelial.[2]
- Mesenchymal stroma - important feature.
Notes:
- Mesenchymal stroma not required for diagnosis -- if >5% ducts.[2]
- No chondroid stroma and <5% ductal cells = myoepithelioma.
- Look for, i.e. rule-out, poorly differentiated carcinoma: carcinoma ex pleomorphic adenoma.
Memory device: MEC = myoepithelium, epithelium, chondromyxoid stroma.
DDx:
- Myoepithelioma.
- Carcinoma ex pleomorphic adenoma.
- Epithelial-myoepithelial carcinoma.
- Polymorphous low-grade adenocarcinoma.
- Adenoid cystic carcinoma.
- Mucoepidermoid carcinoma - occasionally.[3]
Images
Case 1
Case 2
www
IHC
- S-100 +ve.
- SMA +ve.
- GFAP +ve.
Sign out
Left Partial Parotid, Partial Parotidectomy: - Pleomorphic adenoma. - Three benign lymph nodes. - NEGATIVE for malignancy.
Block letters
PAROTID GLAND MASS, RIGHT, EXCISION: - PLEOMORPHIC ADENOMA. - FOUR BENIGN LYMPH NODES. - NEGATIVE FOR MALIGNANCY.
Note:
- Complete excision is often elusive; stating "completely excised" on a surgical pathology report is unwise.[2]
Micro
The sections show a lesion with spindled (myoepithelial) cells and an epithelial component, on a background of a chondromyxoid stroma. The lesion is encapsulated by a thin layer of fibrous tissue. No nuclear atypia is apparent. Mitotic activity is not identified.
Unremarkable parotid gland and lymph nodes are present.
Alternate
The sections show a lesion with spindled (myoepithelial) cells and an epithelial component, on a background of a myxoid stroma. The lesion is mostly encapsulated by a thin layer of fibrous tissue. A small focus of macrophages is present. Significant nuclear atypia is not identified. Mitotic activity is not apparent. Unremarkable parotid gland and a morphologically benign lymph node are present. Ink is seen on the tumour.
See also
References
- ↑ 1.0 1.1 Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 295. ISBN 978-0443069604.
- ↑ 2.0 2.1 2.2 Weinreb I. 10 January 2011.
- ↑ Siddiqui, NH.; Wu, SJ. (Apr 2005). "Fine-needle aspiration biopsy of cystic pleomorphic adenoma with adnexa-like differentiation mimicking mucoepidermoid carcinoma: a case report.". Diagn Cytopathol 32 (4): 229-32. doi:10.1002/dc.20215. PMID 15754364.