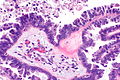
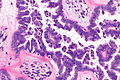
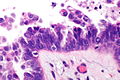
Serous borderline tumour
| Serous borderline tumour | |
|---|---|
| Diagnosis in short | |
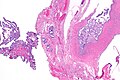
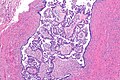
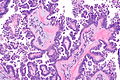
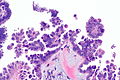
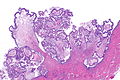
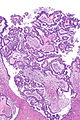
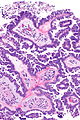
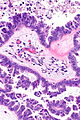
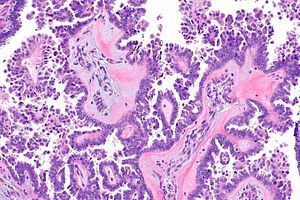 Serous borderline tumour with a micropapillary pattern. H&E stain. | |
|
| |
| LM | cuboidal to columnar epithelium with mild to moderate atypia, no invasion (see below), "sparse" mitoses ,+/-psammoma bodies, +/-micropapillary architecture (often described as a medusa head pattern) |
| Subtypes | serous borderline tumour (SBT) with micropapillary pattern, typical SBT or SBT not otherwise specified |
| LM DDx | serous cystadenoma, serous carcinoma of the ovary, clear cell carcinoma of the ovary |
| Site | ovary, uterine tube - see ovarian tumours |
|
| |
| Prevalence | uncommon |
| Prognosis | usually benign, need follow-up |
| Clin. DDx | other ovarian tumours (benign and malignant) |
| Treatment | excision, follow-up |
Serous borderline tumour is a Muellerian epithelial ovarian tumour with a behaviour that borders on malignant.
It is also known as serous tumour of low malignant potential, abbreviated SLMP.[1][2]
Serous ovarian tumour of low malignant potential redirects here.[2]
General
- Usually benign.
- Require long term follow-up.
Microscopic
Features:[3]
- Cuboidal to columnar epithelium with mild to moderate atypia.
- Non-invasive.
- "Sparse" mitoses.
- +/-Psammoma bodies.
- +/-Micropapillary architecture - often described as a medusa head pattern.
DDx:
- Serous carcinoma of the ovary - focus a with stromal invasion >5mm (linear measurement) or > 10 mm2 (area).[3]
- Invasive cells are "pink", i.e. have abundant eosinophilic cytoplasm,[3]; also, cells usu. large (~2-3x size of non-invasive component), and typically have an enlarged nucleus (~2x non-invasive component).
- Clear cell carcinoma of the ovary - classically associated with endometriosis, have simpler, smaller papillae without branching.
- Serous cystadenoma of the ovary.
Images
www
Subclassification
Typical subdivided into:[5]
- Micropapillary serous borderline tumour.
- Typical serous borderline tumour (SBOT).
Sign out
Cyst and Right Fallopian Tube, Excision: - SEROUS BORDERLINE TUMOUR with micropapillary architecture, see comment. - Fallopian tube within normal limits. - NEGATIVE for evidence of invasion. Comment: The lesion appears to be confined to a cystic structure.
See also
References
- ↑ Seidman, JD.; Kurman, RJ. (May 2000). "Ovarian serous borderline tumors: a critical review of the literature with emphasis on prognostic indicators.". Hum Pathol 31 (5): 539-57. PMID 10836293.
- ↑ 2.0 2.1 Dietel, M.; Hauptmann, S. (May 2000). "Serous tumors of low malignant potential of the ovary. 1. Diagnostic pathology.". Virchows Arch 436 (5): 403-12. PMID 10881733.
- ↑ 3.0 3.1 3.2 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 399. ISBN 978-0443069208.
- ↑ Burkholz, KJ.; Wood, BP.; Zuppan, C.. "Best cases from the AFIP: Borderline papillary serous tumor of the right ovary.". Radiographics 25 (6): 1689-92. doi:10.1148/rg.256055015. PMID 16284143.
- ↑ Park, JY.; Kim, DY.; Kim, JH.; Kim, YM.; Kim, KR.; Kim, YT.; Nam, JH. (Dec 2011). "Micropapillary pattern in serous borderline ovarian tumors: does it matter?". Gynecol Oncol 123 (3): 511-6. doi:10.1016/j.ygyno.2011.08.008. PMID 21917305.