Difference between revisions of "Lichen sclerosus"
Alessandro (talk | contribs) m (typos) |
|||
| Line 20: | Line 20: | ||
| Clinicalhx = | | Clinicalhx = | ||
| Signs = | | Signs = | ||
| Symptoms = | | Symptoms = pruritus | ||
| Prevalence = | | Prevalence = | ||
| Bloodwork = | | Bloodwork = | ||
| Line 45: | Line 45: | ||
Clinical: | Clinical: | ||
* | *Pruritus -> leads to scratching. | ||
*Chronic condition. | *Chronic condition. | ||
*Usu. post-menopausal women. | *Usu. post-menopausal women. | ||
| Line 103: | Line 103: | ||
===Micro=== | ===Micro=== | ||
==== | ====Inflammatory phase of lichen sclerosus==== | ||
The sections show skin with a lymphoplasmacytic predominant interface dermatitis with hyperkeratosis. Spongiosis is present. Scattered inflammatory cell are found with the basal aspect of the epidermis; however, they do not form clusters. No mitotic activity is appreciated. | The sections show skin with a lymphoplasmacytic predominant interface dermatitis with hyperkeratosis. Spongiosis is present. Scattered inflammatory cell are found with the basal aspect of the epidermis; however, they do not form clusters. No mitotic activity is appreciated. | ||
Revision as of 14:55, 4 March 2019
| Lichen sclerosus | |
|---|---|
| Diagnosis in short | |
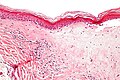
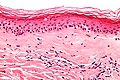
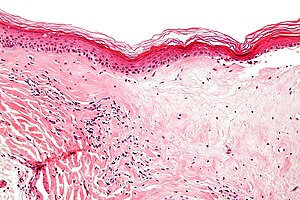 Lichen sclerosus. H&E stain. | |
|
| |
| Synonyms | balanitis xerotica obliterans (old term for lesion on glans penis) |
|
| |
| LM | fibrosis of dermis with loss of adnexal structures - key feature, loss of the rete ridges, (severe) hyperkeratosis, inflammation - often with eosinophils |
| LM DDx | morphea profunda, differentiated vulvar intraepithelial neoplasia, lichen planus, cutaneous amyloidosis, malignant melanoma with regression |
| Site | vulva, penis, urethra |
|
| |
| Associated Dx | differentiated vulvar intraepithelial neoplasia, vulvar squamous cell carcinoma |
| Symptoms | pruritus |
| Prognosis | chronic, benign |
| Lichen sclerosus | |
|---|---|
| External resources | |
| EHVSC | 9993 |
Lichen sclerosus is a relatively common chronic condition classically associated with the vulva. On the vulva is also known as chronic atrophic vulvitis.
On the glans penis it was referred to as balanitis xerotica obliterans, abbreviated BXO.[1][2]
General
- Associated with differentiated vulvar intraepithelial neoplasia - important.
- Approximately 50% of vulvar cancer associated with lichen sclerosus.
Clinical:
- Pruritus -> leads to scratching.
- Chronic condition.
- Usu. post-menopausal women.
- May lead to labial fusion.
Treatment:
- Steroids - high dose initially, then a maintenance therapy to prevent relapse.
Notes:
- Mixed vulvar dystrophy = lichen sclerosus + squamous cell hyperplasia.[3]
Microscopic
Features:[4]
- Loss of rete ridges.
- Severe hyperkeratosis.
- Hyperkeratosis = stratum corneum thickened.
- Fibrosis of the superficial dermis with loss of adnexal structures - key feature.
- Superficial dermis appears pale and homogeneous (distinct collagen bundles are lost).[5]
- Lichenoid inflammatory infiltrate - often with eosinophils; may destroy the dermal-epidermal junction leading to blister formation.
- May be prominent - in the inflammatory phase of the disease.[6]
Notes:
- May have angiokeratoma-like changes.[7]
DDx:
- Morphea profunda - deep fibrosis.
- Differentiated vulvar intraepithelial neoplasia - commonly co-exists with lichen sclerosus.
- Lichen planus (LP) - esp. for the inflammatory phase of lichen sclerosus.
- LP has wedge shaped hypergranulosis, lacks basilar exocytosis, no epidermal atrophy.[6]
- Cutaneous amyloidosis - classically has "cracked" appearance.
- Malignant melanoma with regression - esp. for the inflammatory phase of lichen sclerosus.
- Mycosis fungoides - the inflammatory infiltrate of lichen sclerosis can closely mimic mycosis fungoides (which almost never presents in a genital area).[8]
Images
www:
Sign out
VULVA, BIOPSY: - LICHEN SCLEROSUS.
FORESKIN, CIRCUMCISION: - LICHEN SCLEROSUS.
Note:
- BXO afflicts the glans penis.
Micro
Inflammatory phase of lichen sclerosus
The sections show skin with a lymphoplasmacytic predominant interface dermatitis with hyperkeratosis. Spongiosis is present. Scattered inflammatory cell are found with the basal aspect of the epidermis; however, they do not form clusters. No mitotic activity is appreciated.
Focal hypergranulosis and focal parakeratosis is present. Numerous Civatte bodies are identified.
The focal hypergranulosis is not wedge-shaped. There are no pointed rete ridges. There is no basal squamatization.
Sclerotic phase of lichen sclerosus
The sections show skin with loss of the rete ridges, hyperkeratosis and marked fibrosis of the superficial dermis. Few, scattered lymphocytes are seen in the dermis.
A granular layer is present. There is no basal nuclear atypia. There is no acanthosis.
Sclerotic phase of lichen sclerosus with active inflammation
The sections show skin with loss of the rete ridges, a thin epidermis, hyperkeratosis and marked fibrosis of the superficial dermis. Numerous lymphocytes are seen scattered between the collagen fibres in the deeper aspect of the dermis.
A granular layer is present. There is no basal nuclear atypia.
See also
References
- ↑ Finkbeiner AE (January 2003). "Balanitis xerotica obliterans: a form of lichen sclerosus". South. Med. J. 96 (1): 7–8. PMID 12602704.
- ↑ Stewart, L.; McCammon, K.; Metro, M.; Virasoro, R. (Mar 2014). "SIU/ICUD Consultation on Urethral Strictures: Anterior urethra-lichen sclerosus.". Urology 83 (3 Suppl): S27-30. doi:10.1016/j.urology.2013.09.013. PMID 24268357.
- ↑ Kini, U. (Jun 1997). "Squamous cell carcinoma of the vulva in association with mixed vulvar dystrophy. A brief report with review of literature.". Indian J Cancer 34 (2): 92-5. PMID 9491669.
- ↑ URL: http://www.pathologyoutlines.com/vulva.html#lichensclerosis. Accessed on: 19 April 2011.
- ↑ URL: http://www.webpathology.com/image.asp?n=2&Case=538. Accessed on: 25 August 2011.
- ↑ 6.0 6.1 Fung, MA.; LeBoit, PE. (Apr 1998). "Light microscopic criteria for the diagnosis of early vulvar lichen sclerosus: a comparison with lichen planus.". Am J Surg Pathol 22 (4): 473-8. PMID 9537476.
- ↑ Luzar, B.; Neil, SM.; Calonje, E. (May 2009). "Angiokeratoma-like changes in extragenital and genital lichen sclerosus.". J Cutan Pathol 36 (5): 540-2. doi:10.1111/j.1600-0560.2008.01091.x. PMID 19187108.
- ↑ Citarella, L.; Massone, C.; Kerl, H.; Cerroni, L. (Dec 2003). "Lichen sclerosus with histopathologic features simulating early mycosis fungoides.". Am J Dermatopathol 25 (6): 463-5. PMID 14631186.