Difference between revisions of "Small cell lymphomas"
Jump to navigation
Jump to search
m (photomicrograph) |
|||
| Line 124: | Line 124: | ||
==Hairy cell leukemia== | ==Hairy cell leukemia== | ||
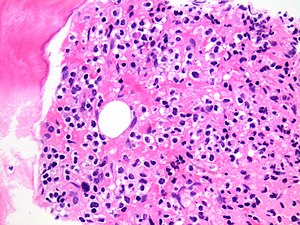
[[File:Bone marrow infiltration by hairy cell leukaemia.jpg|thumb|High power magnification of a bone marrow trephine showing infiltration by hairy cell leukaemia.]] | |||
*Abbreviated ''HCL''. | *Abbreviated ''HCL''. | ||
===General=== | ===General=== | ||
Revision as of 09:16, 2 June 2018
The small cell lymphomas are a collection of commonly seen lymphomas that have a near-identical histomorphologic appearance.
The group includes:
- Small lymphocytic lymphoma/chronic lymphocytic leukemia.
- Follicular lymphoma.
- Mantle cell lymphoma.
- Marginal zone lymphoma (includes MALT lymphoma).
- Hairy cell leukemia.
- Immunoproliferative small intestinal disease (IPSID).[1]
Table of B-cell lymphoma
Small cell lymphomas:
| Name | Location | Size of cells | IHC | Translocations | Clinical | Other |
|---|---|---|---|---|---|---|
| Follicular lymphoma | Follicle | Small, centrocytes, centroblasts | CD10+, BCL6+[2] | t(14;18)(q32;q21) IGH/BCL2[3] | may transform into DLBCL | very common |
| Mantle cell lymphoma | mantle zone | small | CD5+, CD23-, CD43+, cyclin D1+[2] | t(11;14)(q13;q32) BCL1/IGH[4] (also IGH/BCL1[5]) | aggressive, poor prognosis[6] | DDx: Castleman disease |
| Marginal zone lymphoma (includes MALT) | marginal zone, spleen, GI tract | small | CD21+, CD11c+, CD5-, CD23-[2] | t(11;18)(q21;q21) / API2‐MALT1, t(14;18)(q32;q21) / IGH‐MALT1, t(1;14)(p22;q32) / IGH‐BCL10[7] | classical GI lymphoma | subtypes: extranodal marginal zone lymphoma (AKA MALT lymphoma), SMZL, nodal marginal zone lymphoma |
| Precursor B cell lymphoblastic lymphoma/leukemia | location ? | small | CD10+, CD5-, TdT+, CD99+[2] | t(9;22), others | good prognosis (?) | other ? |
| B cell small lymphocytic lymphoma / chronic lymphocytic leukemia |
location ? | small | CD5+, CD23+, CD43+, cyclin D1- | trisomy 12; deletions of 11q, 13q, 17p[8] | good prognosis / indolent course | other ? |
Common medium and large cell lymphomas:
| Name | Location | Size of cells | IHC | Translocations | Clinical | Other |
|---|---|---|---|---|---|---|
| Burkitt's lymphoma | follicle | large cells | CD10, BCL6 | t(8;14) (q24;q32) | rapid growth | "starry sky" |
| Diffuse large B cell lymphoma | follicle (?) | large 4-5X of lymphocyte | MIB1 >40% | none/like follicular l. | poor prognosis | common among lymphomas |
Follicular lymphoma
- Abbreviated FL.
Main article: Follicular lymphoma
Mantle cell lymphoma
- Abbreviated MCL.
Main article: Mantle cell lymphoma
Marginal zone lymphoma
Main article: Marginal zone lymphoma
Classification:
- Extranodal marginal zone lymphoma.
- If in mucosa-associated lymphoid tissue known as a MALT lymphoma, AKA MALToma.
- Splenic marginal zone lymphoma (SMZL).
- Nodal marginal zone lymphoma (NMZL).
Hairy cell leukemia
- Abbreviated HCL.
General
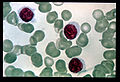
- Name comes from appearance on blood smear - cell hairy.
- Do to the biology, dry taps are common.[9]
Clinical:[10]
- Pancytopenia.
- Splenic enlargement.
- No lymphadenopathy.
- Good prognosis (with treatment), though (likely) not curable.
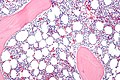
Gross
Features:[11]
- Huge beefy red spleen.
- Red as white pulp obliterated.
Microscopic
Features:[12]
- Small cells (10-20 micrometers) with "Fried egg"-like appearance:
- Well-demarcated fuzzy cell borders,
- Clear/whispy cytoplasm and,
- Central round nucleus.
- Peri-nuclear clearing ("water-clear rim"[13]) -- key feature.
DDx:
Images
www:
- HCL - bone marrow (nlm.nih.gov) from Holland-Frei Cancer Medicine (nlm.nih.gov).
- HCL - several images (upmc.edu).
- HCL - another case with several images (upmc.edu).
- HCL in the spleen (webpathology.com).
IHC
Features:[14]
- CD20 +ve, CD25 +ve, CD103 +ve.
- CD5 -ve.
Flow cytometry:
- CD19 +ve, CD11c +ve, FMC7 +ve.
B cell small lymphocytic lymphoma/chronic lymphocytic leukemia
Precursor B-cell lymphoblastic lymphoma/leukemia
General
- Good prognosis.
- Paediatric - usu. <6 years old.
Microscopic
Features:[15]
- High mitotic rate.
- "Starry sky" pattern.
- Small nucleoli.
IHC
Features:[2]
- CD10 +ve, TdT +ve, CD99 +ve.
- CD5 -ve.
Molecular
Subclassification based on molecular abnormalities (translocations, rearrangements):[16]
- t(9;22) / BCR-ABL.
- t(1;19) / E2A-PBX1.
- t(12;21) / ETV-CBFalpha.
- MLL rearrangement.
Precursor T-cell lymphoblastic lymphoma/leukemia
General
- Prognosis poor. (???)
Microscopic
Features:
- Small lymphoid cells. (???)
IHC
Features:[17]
- TdT +ve, CD34 +ve, CD99 +ve, CD1a +ve/-ve.
- TIA1 -ve.
See also
References
- ↑ Al-Saleem T, Al-Mondhiry H (March 2005). "Immunoproliferative small intestinal disease (IPSID): a model for mature B-cell neoplasms". Blood 105 (6): 2274–80. doi:10.1182/blood-2004-07-2755. PMID 15542584. http://bloodjournal.hematologylibrary.org/cgi/content/long/105/6/2274.>
- ↑ 2.0 2.1 2.2 2.3 2.4 Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 95. ISBN 978-0443066450.
- ↑ Yanai, S.; Nakamura, S.; Takeshita, M.; Fujita, K.; Hirahashi, M.; Kawasaki, K.; Kurahara, K.; Sakai, Y. et al. (Dec 2010). "Translocation t(14;18)/IGH-BCL2 in gastrointestinal follicular lymphoma: correlation with clinicopathologic features in 48 patients.". Cancer. doi:10.1002/cncr.25811. PMID 21192062.
- ↑ URL: http://atlasgeneticsoncology.org/Anomalies/t1114ID2021.html. Accessed on: 10 August 2010.
- ↑ URL: http://www.wipo.int/patentscope/search/en/WO2010059499. Accessed on: 26 May 2011.
- ↑ Hankin, RC.; Hunter, SV. (Dec 1999). "Mantle cell lymphoma.". Arch Pathol Lab Med 123 (12): 1182-8. doi:10.1043/0003-9985(1999)1231182:MCL2.0.CO;2. PMID 10583923.
- ↑ Bacon CM, Du MQ, Dogan A (April 2007). "Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists". J. Clin. Pathol. 60 (4): 361–72. doi:10.1136/jcp.2005.031146. PMC 2001121. PMID 16950858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001121/.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 318. ISBN 978-1416054542.
- ↑ Galani, KS.; Subramanian, PG.; Gadage, VS.; Rahman, K.; Ashok Kumar, MS.; Shinde, S.; Mahadik, S.; Ansari, R. et al. "Clinico-pathological profile of Hairy cell leukemia: critical insights gained at a tertiary care cancer hospital.". Indian J Pathol Microbiol 55 (1): 61-5. doi:10.4103/0377-4929.94858. PMID 22499303.
- ↑ URL: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cmed&part=A34022. Accessed on: 20 August 2010.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 326. ISBN 978-1416054542.
- ↑ URL: http://emedicine.medscape.com/article/200580-diagnosis. Accessed on: 18 August 2010.
- ↑ URL: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cmed&part=A34022. Accessed on: 20 August 2010.
- ↑ URL: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cmed&part=A34022&rendertype=table&id=A34029. Accessed on: 20 August 2010.
- ↑ DG. 17 August 2010.
- ↑ Randolph TR (2004). "Advances in acute lymphoblastic leukemia". Clin Lab Sci 17 (4): 235–45. PMID 15559730. http://findarticles.com/p/articles/mi_qa3890/is_200410/ai_n9429273/pg_2.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 97. ISBN 978-0443066450.