Difference between revisions of "Gallbladder"
(→Xanthogranulomatous cholecystitis: *added pancreatic heterotopia) |
|||
| Line 190: | Line 190: | ||
Notes: | Notes: | ||
* | *Low grade dysplasia should prompt targeted sampling and review.<ref name=uscap2017_akki/> | ||
*Gallbladders with high grade dysplasia should be [[submitted in total]] to exclude [[gallbladder adenocarcinoma]].<ref name=uscap2017_akki>Akki ''et al.'' (2017) "Detecting Incidental Gallbladder Adenocarcinoma: When to Submit the Entire Gallbladder". Available at: [http://www.abstracts2view.com/uscap17/view.php?nu=USCAP17L_2016 http://www.abstracts2view.com/uscap17/view.php?nu=USCAP17L_2016]. United States and Canadian Academy of Pathology Annual Meeting. Accessed on: April 9, 2017.</ref> | |||
DDx: | DDx: | ||
Revision as of 14:04, 30 October 2017
The gallbladder, in pathology (and general surgery), is a growth industry... due to the worsening obesity epidemic.
Normal
Anatomy
- Body.
- Fundus.
- Neck.
Variations:
- Hartmann's pouch - invagination of the gallbladder wall at the origin of the cystic duct.
Image:
Histology
- No muscularis mucosae.
- Small amount of lymphocytes in the lamina propria.
Note:
- As there is no muscularis mucosae, the cancer staging is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion.
Image
Overview
Most common:
- Cholelithiasis with cholecystitis.
Common:
- Antral-type metaplasia.
Uncommon:
- Intestinal metaplasia.
- Gallbladder dysplasia.
- Gallbladder carcinoma.
Common
Chronic cholecystitis
Acute cholecystitis
Gallbladder cholesterolosis
Cholelithiasis
- AKA gallstones.
Less common pathologic diagnoses
Adenomyoma of the gallbladder
General
- Glands in muscle.
- Analogous to what happens in the uterus.
- Significance - may mimic malignant tumours of the gallbladder.[2][3]
- Uncommon.
Gross
- Cystic spaces (Rokitansky-Aschoff sinuses) - may be seen on imaging.[4][5]
- Gallbladder wall thickening.
Microscopic
Features:[6]
- Glands in muscularis propria of the gallbladder wall - key feature.
- Significant muscular hypertrophy - key feature.
- No nuclear atypia.
DDx:
- Gallbladder carcinoma.
- Chronic cholecystitis - has less muscular hypertrophy; overlaps with this diagnosis.[6]
- Phrygian cap.[7]
Image
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH MILD CHOLESTEROLOSIS AND ADENOMYOSIS (FUNDUS). - CHOLELITHIASIS.
Gallbladder polyps
General
- Polyps are significant as they may be adenomatous, i.e. pre-cancerous.
- These are similar to polyps found elsewhere GI tract.
Microscopic
- See intestinal polyps.
Flat dysplasia:[8]
- Nuclear changes.
- Increased NC ratio.
- Hyperchromasia (essential).
- +/-Intestinal metaplasia --> goblet cells.
Gallbladder diverticulosis
General
- Uncommon.
- Thought to arise in the context of an outflow obstruction.[9]
Microscopic
Features:
- Mucosal pouch penetrating the muscularis propria of the gallbladder wall - key feature.
DDx:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH DIVERTICULOSIS. - CHOLELITHIASIS.
Xanthogranulomatous cholecystitis
- Abbreviated XGC.
Pancreatic heterotopia
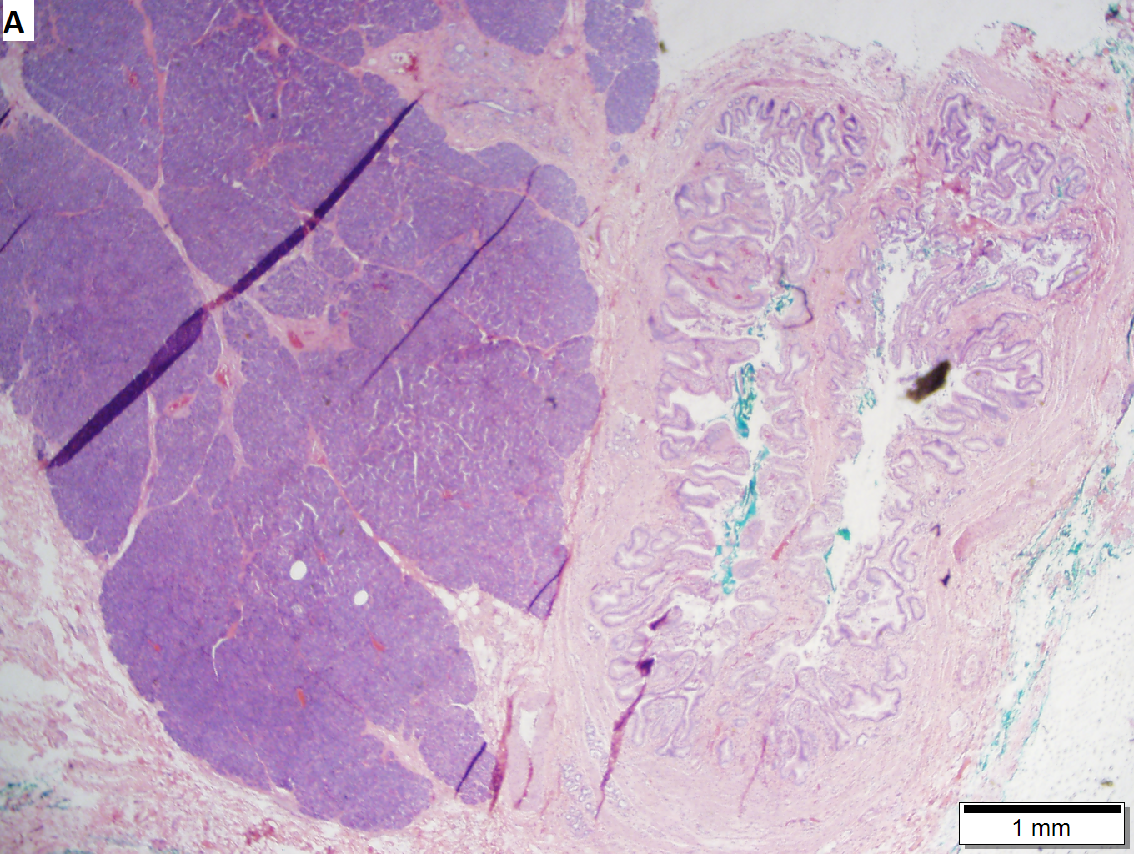
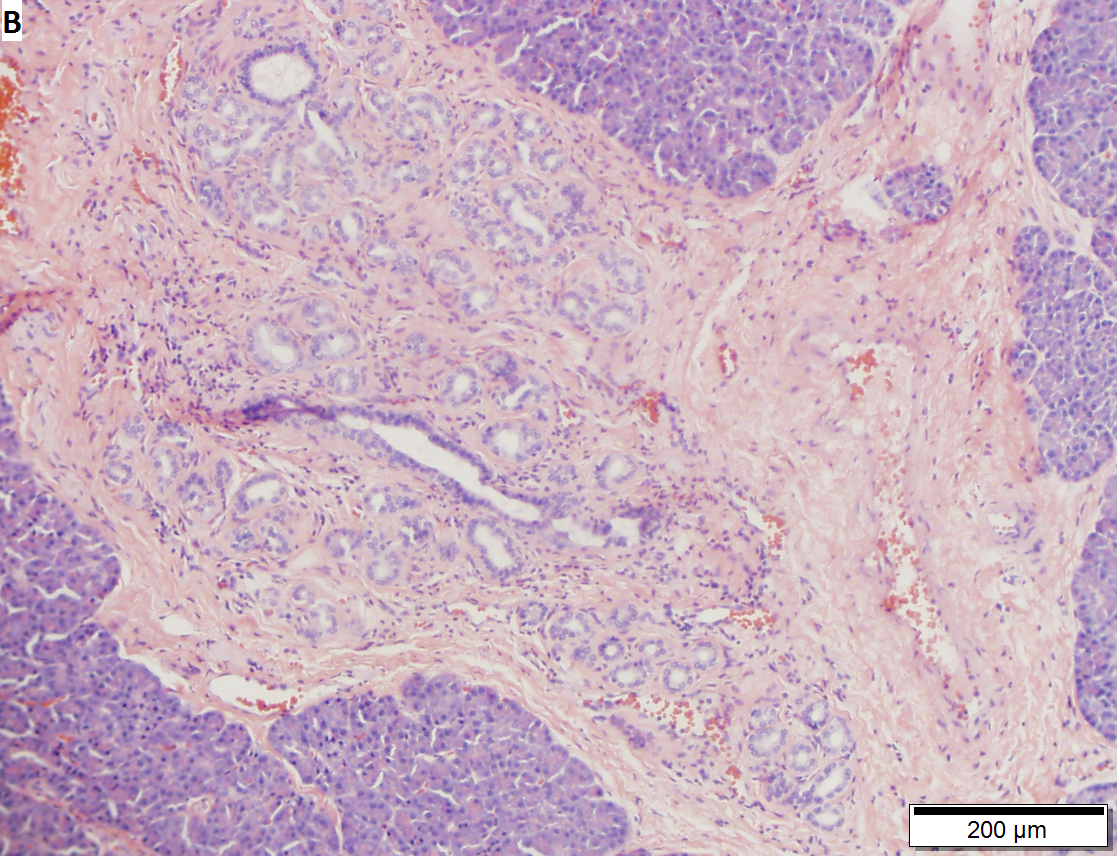


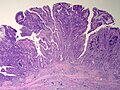
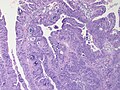
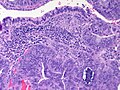
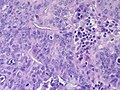
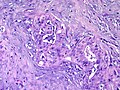
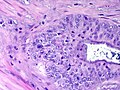
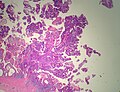
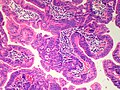
Pancreatic heterotopia near cystic duct in 35 year old women. A. The cystic duct margin is at right; the heterotopia, at left. This cannot be a portion of the pancreas because the cystic duct margin lies proximal to the common bile duct. B. Pancreatic ducts with lobular proliferation, but without the inflammation that would usually be present were this obstruction by a gallstone. C. Nuclei of the duct and the proliferated bile ductules are bland. D. Acini are unremarkable; no pancreatic islets were seen in this case.
Premalignant lesions
General
- Metaplasia associated with carcinoma.[10]
Hypothesis:[11]
- Antral type metaplasia --> intestinal metaplasia --> dysplasia --> carcinoma.
Intestinal metaplasia of the gallbladder
- AKA gallbladder intestinal metaplasia.
Antral type metaplasia
General
Microscopic
Features:[12]
- Columnar cells with:
- Abundant, pale, apical mucin.
- Small basal nucleus.
- Cells often in nests -- below luminal surface.
- Cells vaguely resemble foveollar epithelium of the stomach.
Notes:
- May look similar to cells of the gallbladder neck[12] and common bile duct.[13]
- These glandular cells are not as columnar and have less well-defined cell borders.
- Cells with antral type metaplasia >2:1 (height:width), benign mucosal glands <2:1.
- These glandular cells are not as columnar and have less well-defined cell borders.
Images:
Sign out
Gallbladder, Cholecystectomy: - Chronic cholecystitis with antral-type metaplasia, NEGATIVE for dysplasia. - Cholelithiasis.
Gallbladder adenoma
- Gallbladder dysplasia redirects here.
General
- Premalignant lesion.
- May be associated with familial adenomatous polyposis or Peutz-Jeghers syndrome.[14]
Microscopic
Features:
- Gallbladder epithelium with:
- Nuclear atypia - key feature.
- Nuclear hyperchromasia.
- Nuclear crowding (pseudostratification) or round enlarged nuclei.
- +/-Goblet cells.
- Nuclear atypia - key feature.
Architectural subclassification:[15]
- Papillary ~ 45%.
- Tubulopapillary ~ 30%.
- Tubular ~ 25%.
Notes:
- Low grade dysplasia should prompt targeted sampling and review.[16]
- Gallbladders with high grade dysplasia should be submitted in total to exclude gallbladder adenocarcinoma.[16]
DDx:
- Gallbladder adenocarcinoma.
- Reactive changes.
Images
- Tubular adenoma, biliary type (rsna.org).[14]
- Gallbladder with high-grade dysplasia (flickr.com/lunar caustic).
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - BILIARY TYPE TUBULAR ADENOMA WITH HIGH GRADE DYSPLASIA. - MARGINS CLEAR OF ADENOMA (NEAREST MARGIN 1.0 CM).
Intracholecystic Papillary Neoplasm[17]
General
- Probably some overlap with 'adenoma' above
- Lesion defined as being >1cm.
- Low-grade lesions previously designated “papillary adenoma”
- High-grade lesions previously designated “noninvasive papillary carcinoma.”
- Oten arise in a background of pyloric-gland metaplasia.
- May be associated with invasive adenocarcinoma, which should be reported as intracystic papillary neoplasm with an associated invasive carcinoma and staged.
- Population
- Female (F/M=2:1)
- Mean age 61
- Presentations
- Pain
- Incidental
- No particular association with gallstones.
Microscopic
- Cell types
- Pancreatobiliary type
- Intestinal types with goblet, Paneth, and/or serotonin-containing cells.
- Architecture
- Papillary
- Tubulopapillary
- Tubular
- Dysplasia - high or low grade
Notes: All of the gallbladder should be submitted prior to sign out to exclude invasive adenocarcinoma.
Malignant
Gallbladder carcinoma
See also
References
- ↑ URL: http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder.htm. Accessed on: 13 December 2012.
- ↑ Saul, WM.; Herrmann, PK. (1988). "[Adenomyoma of the gallbladder].". Dtsch Z Verdau Stoffwechselkr 48 (2): 112-6. PMID 3168899.
- ↑ Sasatomi, E.; Miyazaki, K.; Mori, M.; Satoh, T.; Nakano, S.; Tokunaga, O. (Oct 1997). "Polypoid adenomyoma of the gallbladder.". J Gastroenterol 32 (5): 704-7. PMID 9350002.
- ↑ Ching, BH.; Yeh, BM.; Westphalen, AC.; Joe, BN.; Qayyum, A.; Coakley, FV. (Jul 2007). "CT differentiation of adenomyomatosis and gallbladder cancer.". AJR Am J Roentgenol 189 (1): 62-6. doi:10.2214/AJR.06.0866. PMID 17579153.
- ↑ 5.0 5.1 Boscak, AR.; Al-Hawary, M.; Ramsburgh, SR.. "Best cases from the AFIP: Adenomyomatosis of the gallbladder.". Radiographics 26 (3): 941-6. doi:10.1148/rg.263055180. PMID 16702464.
- ↑ 6.0 6.1 Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 439. ISBN 978-0443066573.
- ↑ URL: http://radiopaedia.org/articles/phrygian_cap. Accessed on: 16 May 2014.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 172. ISBN 978-0470519035.
- ↑ Beilby, JO. (Aug 1967). "Diverticulosis of the gall bladder. The fundal adenoma.". Br J Exp Pathol 48 (4): 455-61. PMC 2093791. PMID 4963758. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2093791/.
- ↑ Duarte I, Llanos O, Domke H, Harz C, Valdivieso V (September 1993). "Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples". Cancer 72 (6): 1878–84. PMID 8364865.
- ↑ 11.0 11.1 Mukhopadhyay S, Landas SK (March 2005). "Putative precursors of gallbladder dysplasia: a review of 400 routinely resected specimens". Arch. Pathol. Lab. Med. 129 (3): 386–90. PMID 15737036. http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2.
- ↑ 12.0 12.1 12.2 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 1789. ISBN 978-0781740517.
- ↑ Cutz, E. 3 March 2011.
- ↑ 14.0 14.1 Levy, AD.; Murakata, LA.; Abbott, RM.; Rohrmann, CA.. "From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology.". Radiographics 22 (2): 387-413. PMID 11896229. http://radiographics.rsna.org/content/22/2/387.full.
- ↑ Adsay, V.; Jang, KT.; Roa, JC.; Dursun, N.; Ohike, N.; Bagci, P.; Basturk, O.; Bandyopadhyay, S. et al. (Sep 2012). "Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases.". Am J Surg Pathol 36 (9): 1279-301. doi:10.1097/PAS.0b013e318262787c. PMID 22895264.
- ↑ 16.0 16.1 Akki et al. (2017) "Detecting Incidental Gallbladder Adenocarcinoma: When to Submit the Entire Gallbladder". Available at: http://www.abstracts2view.com/uscap17/view.php?nu=USCAP17L_2016. United States and Canadian Academy of Pathology Annual Meeting. Accessed on: April 9, 2017.
- ↑ Adsay, V.; Jang, KT.; Roa, JC.; Dursun, N.; Ohike, N.; Bagci, P.; Basturk, O.; Bandyopadhyay, S. et al. (Sep 2012). "Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases.". Am J Surg Pathol 36 (9): 1279-301. doi:10.1097/PAS.0b013e318262787c. PMID 22895264.