Difference between revisions of "Primary biliary cholangitis"
(→Microscopic: a second PBC case, this one much more typically hard to diagnose!) |
(→Images: added a case without definite granulomas) |
||
| Line 85: | Line 85: | ||
www: | www: | ||
*[http://www.gidesigns.net/images/MC-copper-flower-garland-L.jpg Garland - wreath of flowers (gidesigns.net)]. | *[http://www.gidesigns.net/images/MC-copper-flower-garland-L.jpg Garland - wreath of flowers (gidesigns.net)]. | ||
{| | |||
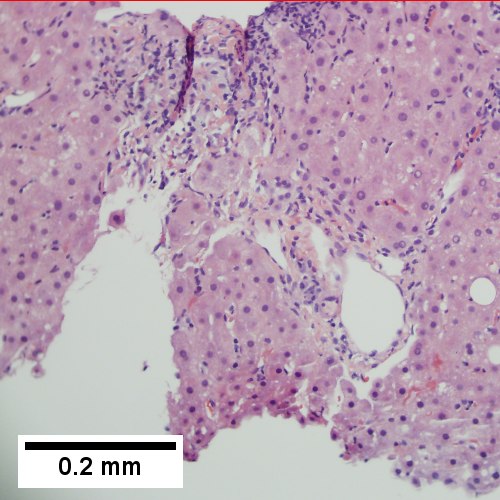
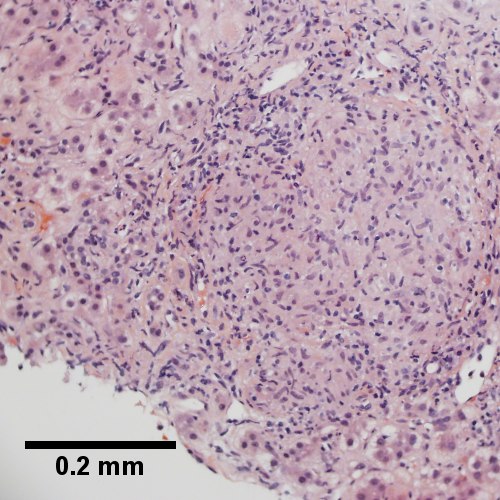
[[File:1 PBC 3 680x512px.tif| Ill defined triads, inflamed lobule (40X).]] | |||
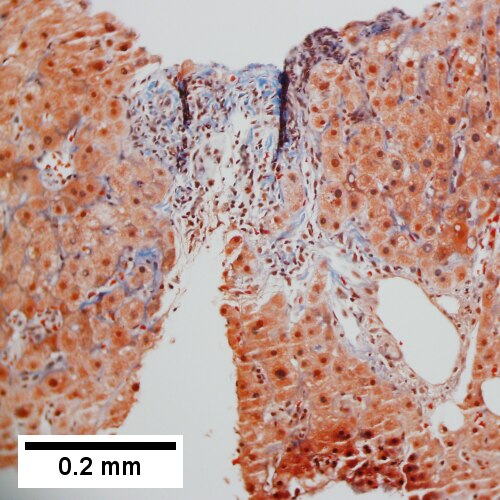
[[File:2 PBC 3 680x512px.tif| Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (400X).]] | |||
[[File:3 PBC 3 680x512px.tif| PAS without diastase shows triad lacking bile duct and piecemeal necrosis (200X).]] | |||
<br> | |||
[[File:4 PBC 3 680x512px.tif| PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (400X).]] | |||
[[File:5 PBC 3 680x512px.tif| Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (100X)..]] | |||
[[File:6 PBC 3 680x512px.tif| Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (200X)]] | |||
|} | |||
Primary biliary cirrhosis. AMA positive. Viral serology/ANA negative. No definite granulomas. Ill defined triads, inflamed lobule (TL 40X). Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (TM 400X). PAS without diastase shows triad lacking bile duct and piecemeal necrosis (TR 200X). PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (BL 400X). Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (BM 100X). Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (BR 200X). | |||
{| | {| | ||
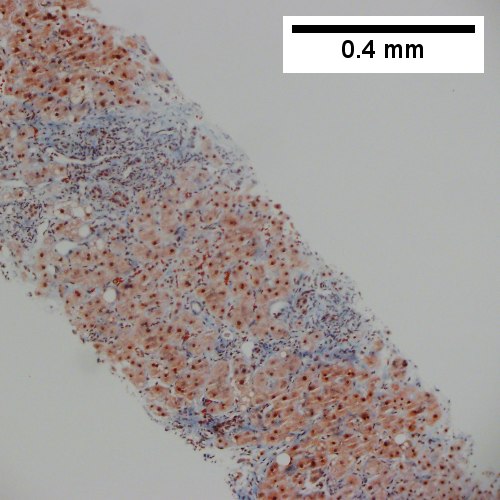
[[File:1 PBC 2 680x512px.tif|Two inflamed triads accompany acini with mild steatosis (20X).]] | [[File:1 PBC 2 680x512px.tif|Two inflamed triads accompany acini with mild steatosis (20X).]] | ||
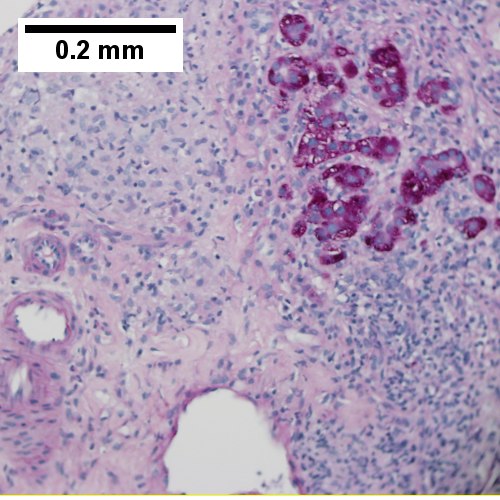
[[File:2 PBC 2 680x512px.tif|A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (200X).]] | [[File:2 PBC 2 680x512px.tif|A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (200X).]] | ||
<br> | |||
[[File:3 PBC 2 680x512px.tif|A triad lacks a bile duct (200X).]] | [[File:3 PBC 2 680x512px.tif|A triad lacks a bile duct (200X).]] | ||
[[File:4 PBC 2 680x512px.tif|Trichrome of the same triad shows portal fibrosis (200X).]] | [[File:4 PBC 2 680x512px.tif|Trichrome of the same triad shows portal fibrosis (200X).]] | ||
| Line 98: | Line 110: | ||
[[File:2 PBC - 1 - 200X 680x512px.tif|Loose granuloma in triad without duct]] | [[File:2 PBC - 1 - 200X 680x512px.tif|Loose granuloma in triad without duct]] | ||
[[File:3 PBC - 1 - 200X 680x512px.tif|Well-formed granuloma]] | [[File:3 PBC - 1 - 200X 680x512px.tif|Well-formed granuloma]] | ||
<br> | |||
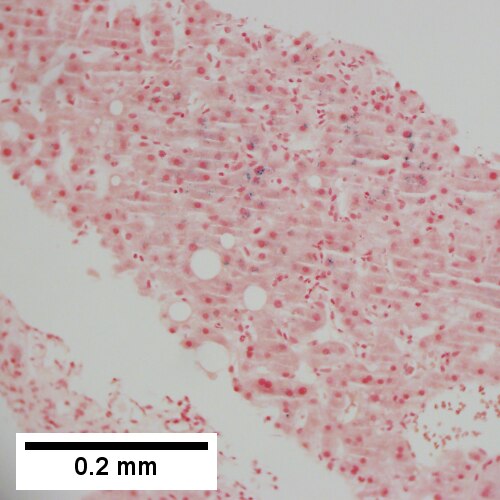
[[File:4 PBC - 1 -200X 680x512px.tif|Piecemeal necrosis, PAS without diastase]] | [[File:4 PBC - 1 -200X 680x512px.tif|Piecemeal necrosis, PAS without diastase]] | ||
[[File:5 PBC - 1 -400X 680x512px.tif|Damaged bile duct, PAS with diastase]] | [[File:5 PBC - 1 -400X 680x512px.tif|Damaged bile duct, PAS with diastase]] | ||
[[File:6 PBC - 1 -200X 680x512px.tif|Bridging fibrosis, trichrome]] | [[File:6 PBC - 1 -200X 680x512px.tif|Bridging fibrosis, trichrome]] | ||
|} | |} | ||
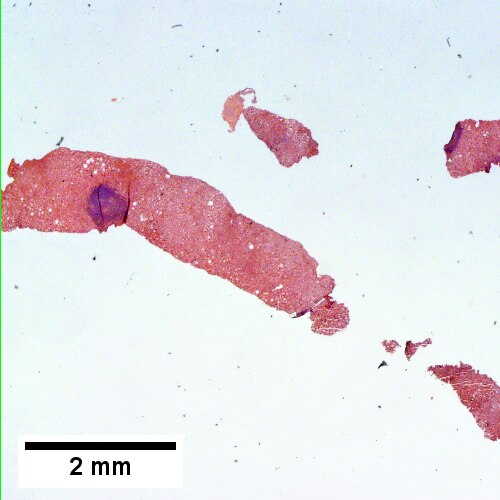
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (TL,40X) Loose granuloma in triad without duct (TM,200X) Well-formed granuloma (TR,200X) Piecemeal necrosis, PAS without diastase (BL,200X) Damaged bile duct, PAS with diastase (BM,400X) Bridging fibrosis, trichrome (BR,200X) | |||
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (TL,40X) Loose granuloma in triad without duct ( | |||
===Staging PBC=== | ===Staging PBC=== | ||
Revision as of 17:01, 29 July 2016
| Primary biliary cholangitis | |
|---|---|
| Diagnosis in short | |
 Primary biliary cirrhosis. H&E stain. | |
|
| |
| LM | "florid duct lesion": intraepithelial lymphocytes - in bile duct, bile duct epithelial cells with eosinophilic cytoplasm; plasma cells; +/-granulomas (close to bile duct); +/-"garland" cirrhosis -- has irregular border |
| LM DDx | sarcoidosis, primary sclerosing cholangitis, viral hepatitis, autoimmune hepatitis, drug-induced liver disease, Hodgkin's lymphoma |
| Site | liver - see medical liver diseases |
|
| |
| Associated Dx | other autoimmune conditions, e.g. celiac disease, Sjögren syndrome |
| Clinical history | woman, middle age |
| Symptoms | pruritis |
| Blood work | AMA +ve |
Primary biliary cirrhosis, abbreviated PBC, is a rare medical liver disease.
General
Epidemiology:
- Female>male (~9:1).[1]
- Usually middle age.
- Associated with other autoimmune conditions (Sjögren syndrome, progressive systemic sclerosis, celiac disease).
Etiology:
- Autoimmune.
Serology:
- AMA +ve.[2]
Classic presentation:
- Pruritis.
Pathophysiology:
- Septal bile duct attacked.
Treatment:
- Ursodeoxycholic acid.
- May be indication for transplant.
Microscopic
Features:
- "Florid duct lesion":[3]
- Intraepithelial lymphocytes - in bile duct - key feature.
- Bile duct epithelial cells with eosinophilic cytoplasm.[4]
- Plasma cells.
- Granulomas - close to bile duct.
- Seen in classic presentation -- often not present or poorly formed.
- Focal damage (may be missed on biopsy -- due to sampling).
- "Garland" cirrhosis -- has irregular border (unlike in EtOH).
- Garland originally "wreath of flowers" (in French).[5]
Notes:
- PAS stain useful for examining basement membrane... which is lost in PBC.
- Lobular inflammation should be minimal.
- May cause cholestatic picture.[6]
DDx:[7]
- Sarcoidosis (if granulomas present).
- Primary sclerosing cholangitis.
- Viral hepatitis.
- Autoimmune hepatitis.
- Drug-induced liver disease.
- Hodgkin's lymphoma.[8]
Images
www:
![Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (400X).](/w/images/thumb/1/17/2_PBC_3_680x512px.tif/lossy-page1-500px-2_PBC_3_680x512px.tif.jpg)
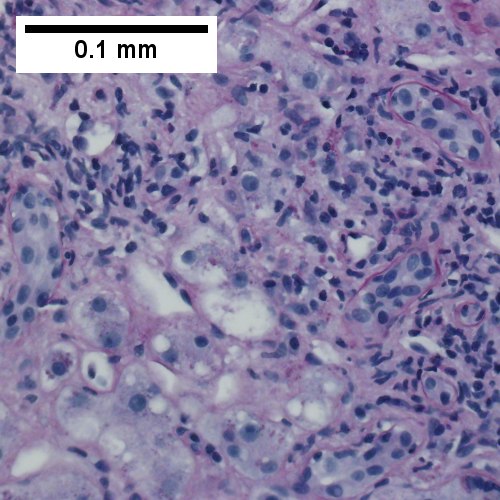
Primary biliary cirrhosis. AMA positive. Viral serology/ANA negative. No definite granulomas. Ill defined triads, inflamed lobule (TL 40X). Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (TM 400X). PAS without diastase shows triad lacking bile duct and piecemeal necrosis (TR 200X). PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (BL 400X). Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (BM 100X). Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (BR 200X).
![A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (200X).](/w/images/thumb/6/65/2_PBC_2_680x512px.tif/lossy-page1-500px-2_PBC_2_680x512px.tif.jpg)
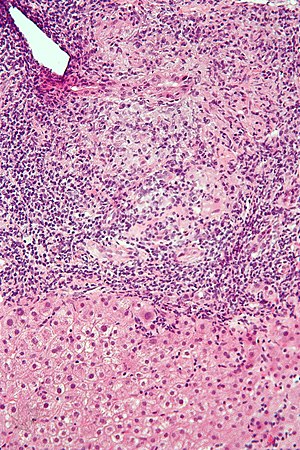
Primary biliary cirrhosis. Two inflamed triads accompany acini with mild steatosis (UL 20X). A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (UR 200X). A triad lacks a bile duct (LL 200X). Trichrome of the same triad shows portal fibrosis (LR 200X).
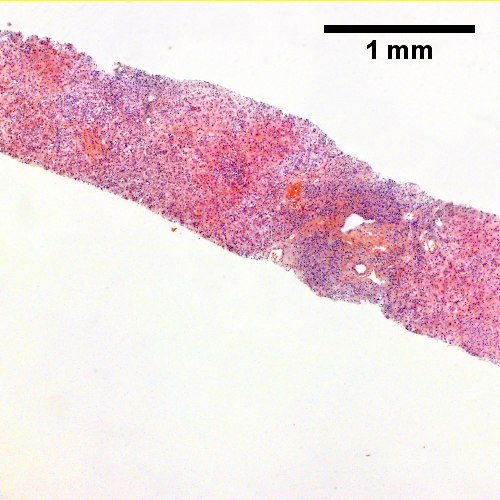
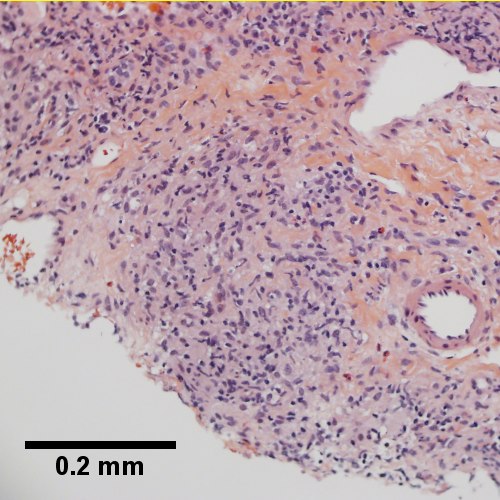
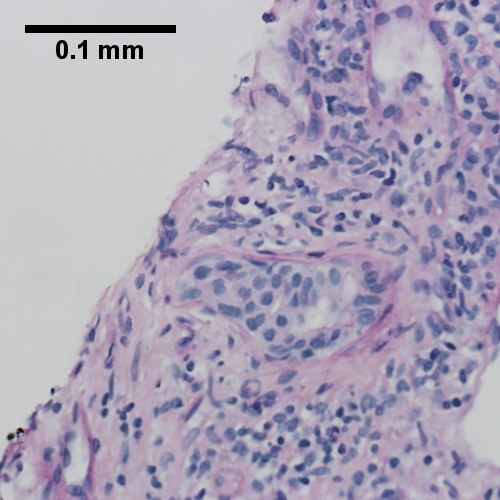
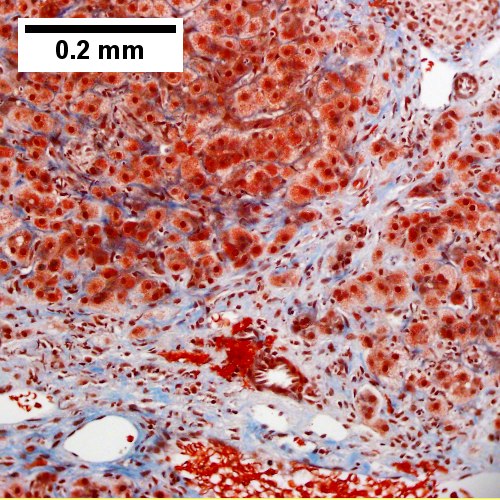
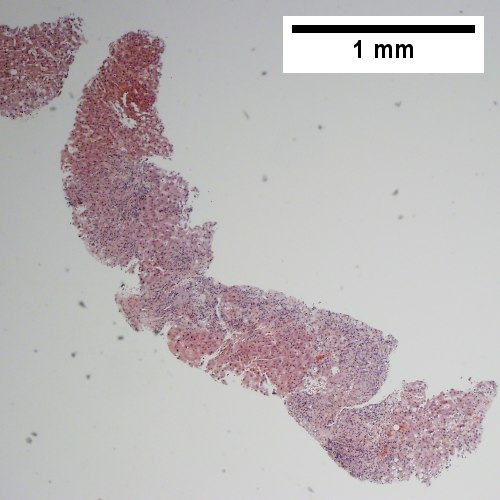
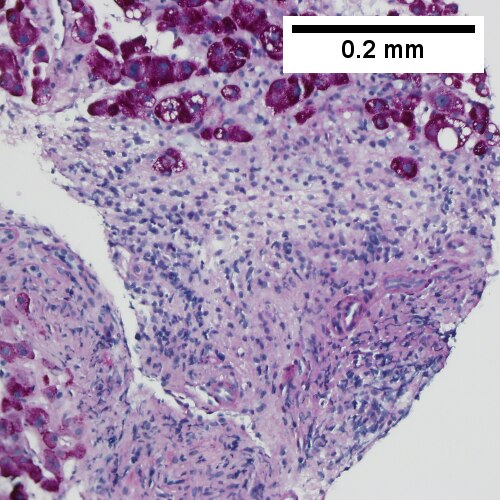
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (TL,40X) Loose granuloma in triad without duct (TM,200X) Well-formed granuloma (TR,200X) Piecemeal necrosis, PAS without diastase (BL,200X) Damaged bile duct, PAS with diastase (BM,400X) Bridging fibrosis, trichrome (BR,200X)
Staging PBC
PBC is staged according to Ludwig:[9]
- Stage 1: Portal - inflammation or bile duct abnormalities.
- Stage 2: Periportal - periportal fibrosis (enlargement of portal tracts) +/- inflammation.
- Stage 3: Septal - septal fibrosis +/-inflammation in septa.
- Stage 4: Cirrhosis - nodules of hepatocytes +/- inflammation.
Notes:
- There can be significant variation in staging on biopsy - due to variability of fibrosis in a PBC liver.[10]
- "Worst area" in biopsy specimen is used to determine stage.
See also
References
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 162. ISBN 978-0470519035.
- ↑ Nguyen, DL.; Juran, BD.; Lazaridis, KN. (Oct 2010). "Primary biliary cirrhosis.". Best Pract Res Clin Gastroenterol 24 (5): 647-54. doi:10.1016/j.bpg.2010.07.006. PMID 20955967.
- ↑ Nakanuma, Y.; Harada, K. (Sep 1993). "Florid duct lesion in primary biliary cirrhosis shows highly proliferative activities.". J Hepatol 19 (2): 216-21. PMID 7905494.
- ↑ OA. 11 September 2009.
- ↑ http://dictionary.reference.com/browse/garland
- ↑ Grimm, D.; Thimme, R. (Apr 2011). "[Cholestatic liver diseases].". Ther Umsch 68 (4): 195-9. doi:10.1024/0040-5930/a000150. PMID 21452140.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 163. ISBN 978-0470519035.
- ↑ Vanishing bile duct syndrome and Hodgkin disease: a case series and review of the literature. Pass AK, McLin VA, Rushton JR, Kearney DL, Hastings CA, Margolin JF. J Pediatr Hematol Oncol. 2008 Dec;30(12):976-80. PMID 19131796.
- ↑ PBC. eMedicine.com. URL: http://emedicine.medscape.com/article/171117-diagnosis. Accessed on: 22 September 2009.
- ↑ J Clin Pathol. 1996 July; 49(7): 556-559. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=500569. Accessed on: September 22, 2009.