Difference between revisions of "Thrombotic microangiopathy"
Jump to navigation
Jump to search
| Line 5: | Line 5: | ||
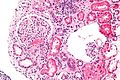
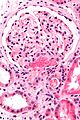
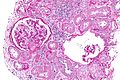
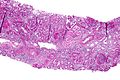
| Caption = Acute thrombotic microangiopathy. [[H&E stain]]. | | Caption = Acute thrombotic microangiopathy. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = microvascular occlusion with "loose" intimal thickening - fluffy appearing intima, +/-onion skin-like appearance | | Micro = microvascular occlusion with "loose" intimal thickening - fluffy appearing intima, fibrin entrapped RBCs, +/-onion skin-like appearance (chronic change) | ||
| Subtypes = | | Subtypes = acute, chronic | ||
| LMDDx = [[vasculitis]] | | LMDDx = [[vasculitis]] | ||
| Stains = | | Stains = | ||
Revision as of 20:11, 25 December 2013
| Thrombotic microangiopathy | |
|---|---|
| Diagnosis in short | |
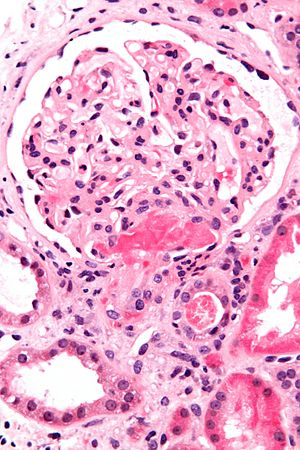 Acute thrombotic microangiopathy. H&E stain. | |
|
| |
| LM | microvascular occlusion with "loose" intimal thickening - fluffy appearing intima, fibrin entrapped RBCs, +/-onion skin-like appearance (chronic change) |
| Subtypes | acute, chronic |
| LM DDx | vasculitis |
| Site | blood vessels - esp. kidney |
|
| |
| Treatment | dependent on underlying cause |
Thrombotic microangiopathy, abbreviated TMA, is a group of disorders affecting small blood vessels. Microangiopathic is a disease affecting small blood vessels.[1]
Differential diagnosis
Clinical
Others:[4]
- Malignant hypertension.[5]
- DIC.
- APLA[6] in SLE.
- Scleroderma renal crisis.
- HIV associated TTP.
- Chemotherapy.
- Calcineurin inhibitor toxicity.
Notes:
- The above cannot be differentiated on a histomorphologic basis.
Histologic
The histomorphologic differential diagnosis is:
- Vasculitis.
- Inflammatory cells within the vessel wall.
- Vessel wall injury, i.e. necrosis.
General
- Underlying pathology: endothelial cell damage.
Microscopic
Features:[7]
- Microvascular occlusion.[8]
- "Loose" intimal thickening; fluffy appearing intima.
- May be have an onion skin-like appearance.
- Fibrin entrapped RBCs.
Notes:
- The last two (#2 and #3) are useful for discrimination from endarteritis.[7]
- Early finding: endothelial cell swelling.
Images
www:
Acute changes:
Chronic changes:
See also
References
- ↑ URL: http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/one/000005089.htm. Accessed on: 9 September 2010.
- ↑ URL: http://emedicine.medscape.com/article/779218-overview. Accessed on: 8 November 2010.
- ↑ Mayer SA, Aledort LM (May 2005). "Thrombotic microangiopathy: differential diagnosis, pathophysiology and therapeutic strategies". Mt. Sinai J. Med. 72 (3): 166–75. PMID 15915311.
- ↑ Benz, K.; Amann, K. (May 2010). "Thrombotic microangiopathy: new insights.". Curr Opin Nephrol Hypertens 19 (3): 242-7. doi:10.1097/MNH.0b013e3283378f25. PMID 20186056.
- ↑ Zhang, B.; Xing, C.; Yu, X.; Sun, B.; Zhao, X.; Qian, J. (Mar 2008). "Renal thrombotic microangiopathies induced by severe hypertension.". Hypertens Res 31 (3): 479-83. doi:10.1291/hypres.31.479. PMID 18497467.
- ↑ Asherson, RA. (1998). "The catastrophic antiphospholipid syndrome, 1998. A review of the clinical features, possible pathogenesis and treatment.". Lupus 7 Suppl 2: S55-62. PMID 9814675.
- ↑ 7.0 7.1 Fogo, Agnes; Bruijn, Jan A.; Cohen, Arthur H.; Colvin, Robert B.;Jennette, J. Charles (2006). Fundamentals of Renal Pathology (1st ed.). Springer. pp. 204. ISBN 978-0387311265.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 670. ISBN 978-1416031215.
- ↑ Ruggenenti, P.; Noris, M.; Remuzzi, G. (Sep 2001). "Thrombotic microangiopathy, hemolytic uremic syndrome, and thrombotic thrombocytopenic purpura.". Kidney Int 60 (3): 831-46. doi:10.1046/j.1523-1755.2001.060003831.x. PMID 11532079.