Difference between revisions of "Muscularis propria invasion in the urinary bladder"
Jump to navigation
Jump to search
(tweak) |
|||
| Line 1: | Line 1: | ||
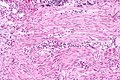
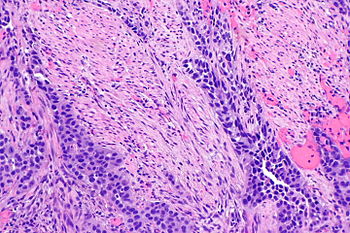
[[Image: Muscle invasive urothelial carcinoma -- intermed mag.jpg |thumb|350px|right | Muscle invasive urothelial carcinoma. [[H&E stain]].]] | |||
The presence or absence of '''muscularis propria invasion in the urinary bladder''' is a ''very important'' determination, as the clinical management changes between T1 and T2: | The presence or absence of '''muscularis propria invasion in the urinary bladder''' is a ''very important'' determination, as the clinical management changes between T1 and T2: | ||
*T1: usually conservative treatment (local excision). | *T1: usually conservative treatment (local excision). | ||
| Line 61: | Line 62: | ||
Image: Muscle invasive urothelial carcinoma -- very low mag.jpg | MIUC - very low mag. | Image: Muscle invasive urothelial carcinoma -- very low mag.jpg | MIUC - very low mag. | ||
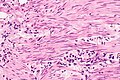
Image: Muscle invasive urothelial carcinoma -- low mag.jpg | MIUC - low mag. | Image: Muscle invasive urothelial carcinoma -- low mag.jpg | MIUC - low mag. | ||
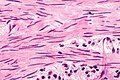
Image: Muscle invasive urothelial carcinoma - alt -- intermed mag.jpg | MIUC - intermed. mag. | Image: Muscle invasive urothelial carcinoma - alt -- intermed mag.jpg | MIUC - intermed. mag. | ||
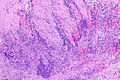
Image: Muscle invasive urothelial carcinoma -- high mag.jpg | MIUC - high mag. | Image: Muscle invasive urothelial carcinoma -- high mag.jpg | MIUC - high mag. | ||
Revision as of 02:26, 28 January 2016
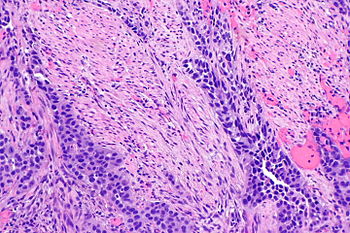
Muscle invasive urothelial carcinoma. H&E stain.
The presence or absence of muscularis propria invasion in the urinary bladder is a very important determination, as the clinical management changes between T1 and T2:
- T1: usually conservative treatment (local excision).
- T2: radical treatment (cystectomy or cystoprostatectomy).
A thin layer of discontinous muscularis mucuosae (MM) is present and, especially if hypertrophic, may be confused with muscuaris propria (MP).
General
Comparing muscularis propria and muscularis mucosae
A comparison between muscularis propria and muscularis mucosae - adapted from Paner et al.:[1]
| Feature | Muscularis mucosae | Muscularis propria |
|---|---|---|
| Outline/border | typically irregular (frayed edges) | usually regular (circumscribed) |
| Size of bundles ‡ | classically "small", often "large" (hypertrophic) | usually "large" |
| Isolated fibres | yes | no |
| Location in bladder | less common in trigone, dome very common | everywhere |
| Depth † | superficial, occ. deep | deep |
Notes:
- † The lamina propria thickness varies with location. It is thinnest in the trigone (0.5-1.6 mm) and thickest in the dome (1.0-3.1 mm).
- ‡ Small is defined as <4 muscle fibres; large >= 4 muscle fibres.
- The presence of hyperplastic bundles ranges from ~20% in the trigone to ~70% in the dome.
Images
Microscopic
Rational assessment of muscularis propria invasion
To call muscularis propria invasion:
- Definite tumour must be between muscle.
- Muscle bundles must be thick.
- Multiple bundles must be adjacent to one another.
- Should not be superficial - surface epithelium if present should be distant.
DDx:
- Invasion of hypertrophic muscularis mucosae.
Images
Sign out
Cannot exclude MP invasion
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE UROTHELIAL CARCINOMA. -- Extensive invasion into at least the lamina propria. - Negative for definite muscularis propria, see comment. Comment: The tumour is seen around bundles of smooth muscle that are favoured to represent muscularis mucosa; however, obliterated muscularis propria cannot be excluded. Correlation with the clinical findings is required. Additional transurethral sampling and/or imaging to assess the muscularis propria is suggested.
See also
References
- ↑ Paner, GP.; Ro, JY.; Wojcik, EM.; Venkataraman, G.; Datta, MW.; Amin, MB. (Sep 2007). "Further characterization of the muscle layers and lamina propria of the urinary bladder by systematic histologic mapping: implications for pathologic staging of invasive urothelial carcinoma.". Am J Surg Pathol 31 (9): 1420-9. doi:10.1097/PAS.0b013e3180588283. PMID 17721199.