Difference between revisions of "Chromophobe renal cell carcinoma"
Jump to navigation
Jump to search
| Line 33: | Line 33: | ||
==General== | ==General== | ||
*Least common of the common types of RCC ([[clear cell RCC]], [[papillary RCC]], [[chromophobe RCC]]). | *Least common of the common types of RCC ([[clear cell RCC]], [[papillary RCC]], [[chromophobe RCC]]). | ||
*[[ISUP nucleolar grading]] ( | *[[ISUP nucleolar grade|ISUP nucleolar grading]] (replaces ''Fuhrman grading'') not done for this entity, as it does not appear to have any predictive value.<ref name=pmid17527087>{{Cite journal | last1 = Delahunt | first1 = B. | last2 = Sika-Paotonu | first2 = D. | last3 = Bethwaite | first3 = PB. | last4 = McCredie | first4 = MR. | last5 = Martignoni | first5 = G. | last6 = Eble | first6 = JN. | last7 = Jordan | first7 = TW. | title = Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. | journal = Am J Surg Pathol | volume = 31 | issue = 6 | pages = 957-60 | month = Jun | year = 2007 | doi = 10.1097/01.pas.0000249446.28713.53 | PMID = 17527087 }}</ref> | ||
*May be associated with [[Birt–Hogg–Dubé syndrome]].<ref name=Ref_WMSP290>{{Ref WMSP|290}}</ref> | *May be associated with [[Birt–Hogg–Dubé syndrome]].<ref name=Ref_WMSP290>{{Ref WMSP|290}}</ref> | ||
Revision as of 18:05, 5 March 2015
| Chromophobe renal cell carcinoma | |
|---|---|
| Diagnosis in short | |
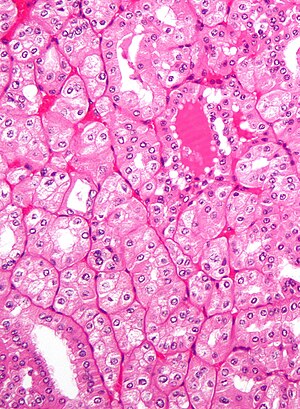 Eosinophilic variant of chromophobe renal cell carcinoma. H&E stain. | |
|
| |
| LM | pale cytoplasm, with wisps of eosinophilic material, perinuclear clearing (a pale halo surrounds the nucleus), periphery of cell distinct (cell membrane is easy to discern -- plant cell-like) |
| Subtypes | classic, eosinophilic variant |
| LM DDx | clear cell renal cell carcinoma (classic), renal oncocytoma, clear cell renal cell carcinoma eosinophilic variant |
| Stains | Hale's colloidal iron (Mueller-Mowry stain) +ve |
| IHC | CK7 +ve cell membrane, CD117 +ve, vimentin -ve |
| Gross | brown/tan, lacks central scar |
| Grossing notes | total nephrectomy for tumour grossing, partial nephrectomy grossing |
| Site | kidney - see renal tumours |
|
| |
| Syndromes | Birt–Hogg–Dubé syndrome |
|
| |
| Prevalence | relatively common |
| Clin. DDx | other renal tumours |
| Treatment | surgical resection |
Chromophobe renal cell carcinoma, abbreviated ChRCC, is a relatively common form of renal cell carcinoma.
General
- Least common of the common types of RCC (clear cell RCC, papillary RCC, chromophobe RCC).
- ISUP nucleolar grading (replaces Fuhrman grading) not done for this entity, as it does not appear to have any predictive value.[1]
- May be associated with Birt–Hogg–Dubé syndrome.[2]
Subtypes
There are two subtypes:[3]
- Classic.
- Eosinophilic variant.
Gross
- Tan, light-brown.
- Solitary, usually.
- Well-circumscribed.
Image:
Microscopic
Classic
Features - classic type (3 P's mnemonic):[4][3]
- Pale cytoplasm, with wisps of eosinophilic material; the cells are not completely clear, they have "cobwebs".
- Perinuclear clearing, i.e. a pale halo surrounds the nucleus - key feature.
- Periphery of cell distinct, i.e. cell membrane is easy to discern.
Notes:
- May have psammoma bodies.
- May be described as "plant-like"; plant cells have (thick) cell walls.
- The perinuclear clearing is often somewhat patchy, i.e. it is usually not present in very tumour cell.
DDx:
- Clear cell RCC (classic).
- Perinuclear clearing is not seen in clear cell RCC.
- ChRCC has wisps in the cytoplasm.
Eosinophilic variant
Features - eosinophilic variant:[3]
- Eosinophilic (finely granular) cytoplasm.
- Perinuclear clearing - key feature.
- Periphery of cell distinct.
- Smaller cells than classic subtype.
Notes:
- May have psammoma bodies.
DDx:
- Oncocytoma - particularly the eosinophilic variant.
- IHC may be useful to differentiate (CK7: oncocytoma = cytoplasm +ve, chromophobe = cell membrane +ve).
- A comparison based on histomorphology: Tabular comparison between ChRCC & oncocytoma.
- Oncocytoma typically has: no perinuclear clearing, no raisinoid nuclei, no binucleation.
- Clear cell RCC, eosinophilic variant.
- Perinuclear clearing is not seen in clear cell RCC.
- ChRCC has wisps in the cytoplasm.
Image
www:
Stains
- Hale's colloidal iron +ve (blue granular cytoplasmic).
- Oncocytoma -ve.
Note:
- This seems to be a difficult stain to get working.
Images
- ChRCC Hale's colloidal iron - several images (nature.com).
- ChRCC Hale's colloidal iron (ultrapath.org).[5]
- ChRCC Hale's colloidal iron (diagnosticpathology.org).
IHC
- CK7 +ve cell membrane.[3]
- Useful for differentiating from oncocytoma.
- CD117 +ve.
- Vimentin -ve.[6][7]
Uncommon stains for ChRCC versus oncocytoma:
ChRCC versus clear cell RCC
- CD117 +ve.
- -ve in CCRCC.
- CAIX (carbonic anhydrase CA IX) -ve.
- +ve (strong membranous) in CCRCC.[11]
- CK7 +ve.
- -ve in CCRCC.
Molecular
- Extensive aneusomy (monosomy?):[12]
- Loss of chromosomes: 1, 2, 6, 10, 13, 17, 21.
Sign out
KIDNEY, RIGHT UPPER POLE, PARTIAL NEPHRECTOMY: - CHROMOPHOBE RENAL CELL CARCINOMA. COMMENT: The sections show a mix of clear cells with wispy cytoplasm, and cells with eosinophilic cytoplasm and perinuclear halos. There are no true papillae. Stains and immunostains: Positive: CK7, CAM5.2, EMA, pankeratin, CD117, colloidal iron. Negative: AMACR, CD10, CD68, RCC, vimentin.
See also
References
- ↑ Delahunt, B.; Sika-Paotonu, D.; Bethwaite, PB.; McCredie, MR.; Martignoni, G.; Eble, JN.; Jordan, TW. (Jun 2007). "Fuhrman grading is not appropriate for chromophobe renal cell carcinoma.". Am J Surg Pathol 31 (6): 957-60. doi:10.1097/01.pas.0000249446.28713.53. PMID 17527087.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 290. ISBN 978-0781765275.
- ↑ 3.0 3.1 3.2 3.3 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 293. ISBN 978-0443066771.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1016-7. ISBN 0-7216-0187-1.
- ↑ URL: http://www.ultrapath.org/oldsite/cases99/sep99/cotm9-2.html. Accessed on: 9 October 2011.
- ↑ Zhang, W.; Yu, WJ.; Jiang, YX.; Li, YJ.; Han, F.; Liu, Y.; Han, ZL. (Feb 2012). "[Chromophobe renal cell carcinoma: a clinicopathologic study and immunophenotypes of 42 cases].". Zhonghua Bing Li Xue Za Zhi 41 (2): 76-80. PMID 22455881.
- ↑ Din, NU.; Fatima, S.; Ahmad, Z. (Dec 2013). "Chromophobe renal cell carcinoma: a morphologic and immunohistochemical study of 45 cases.". Ann Diagn Pathol 17 (6): 508-13. doi:10.1016/j.anndiagpath.2013.06.005. PMID 24095630.
- ↑ Memeo L, Jhang J, Assaad AM, et al. (February 2007). "Immunohistochemical analysis for cytokeratin 7, KIT, and PAX2: value in the differential diagnosis of chromophobe cell carcinoma". Am. J. Clin. Pathol. 127 (2): 225–9. doi:10.1309/9KWEA4W9Y94D1AEE. PMID 17210525. http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17210525.
- ↑ Jain, S.; Roy, S.; Amin, M.; Acquafondata, M.; Yin, M.; Laframboise, W.; Bastacky, S.; Pantanowitz, L. et al. (Dec 2013). "Amylase α-1A (AMY1A): A Novel Immunohistochemical Marker to Differentiate Chromophobe Renal Cell Carcinoma From Benign Oncocytoma.". Am J Surg Pathol 37 (12): 1824-30. doi:10.1097/PAS.0000000000000108. PMID 24225843.
- ↑ Amin MB, Epstein JI, Ulbright TM, et al. (August 2014). "Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): 1017–22. doi:10.1097/PAS.0000000000000254. PMID 25025364.
- ↑ Al-Ahmadie HA, Alden D, Fine SW, et al. (July 2011). "Role of immunohistochemistry in the evaluation of needle core biopsies in adult renal cortical tumors: an ex vivo study". Am. J. Surg. Pathol. 35 (7): 949–61. doi:10.1097/PAS.0b013e31821e25cd. PMID 21677535.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 292. ISBN 978-0781765275.
