Difference between revisions of "Adult granulosa cell tumour"
Jump to navigation
Jump to search
(fix typo) |
(touch) |
||
| Line 1: | Line 1: | ||
'''Adult granulosa cell tumour''' is an [[ovarian tumour]]. It is also known as '''granulosa cell tumour'''. It should '''not''' be confused with the ''[[granular cell tumour]]''. | '''Adult granulosa cell tumour''' is an [[ovarian tumour]]. It is also known as '''granulosa cell tumour'''. It should '''not''' be confused with the ''[[granular cell tumour]]''. | ||
Ideally, it should be called ''adult granulosa cell tumour'' to avoid confusion with ''[[juvenile granulosa cell tumour]]''. | Ideally, it should be called ''adult granulosa cell tumour'' to avoid confusion with ''[[juvenile granulosa cell tumour]]''. | ||
Revision as of 15:24, 2 February 2016
Adult granulosa cell tumour is an ovarian tumour. It is also known as granulosa cell tumour. It should not be confused with the granular cell tumour.
Ideally, it should be called adult granulosa cell tumour to avoid confusion with juvenile granulosa cell tumour.
General
- May secrete estrogen.
- May present with endometrial pathology, e.g. endometrial hyperplasia or endometrioid endometrial carcinoma.
- Occasionally secrete antrogens lead to virilization.[1]
Note:
- Normal granulosa cells convert androgen from the theca cells to estrogen and/or progesterone.[2]
Gross
- Classically solid.
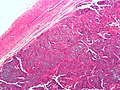
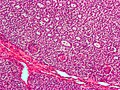
Microscopic
Features:
- Classic appearance includes gland-like structures filled with acidophilic material (Call-Exner bodies).
- Small cuboidal to polygonal cell in sheets or strands or cords.
- Nuclear grooves.
Note:
- There is a "10% rule" -- if less than 10% of a SCST is granulosa cells... it isn't granulosa cell tumour.
- Juvenile variant of GCT has more nuclear pleomorphism.
DDx:[3]
- Urothelial cell carcinoma (UCC).
- UCC usually has extensive necrosis.
- Brenner tumour.
- Sertoli cell tumour.
- Sertoli-Leydig cell tumour.
- Endometrial stromal sarcoma.
Images
IHC
- Inhibin positive.[4]
- Inhibin negative in Brenner tumour.
- Calretinin +ve.
Molecular
- Currently not used for diagnosis.
See also
References
- ↑ Patel, SS.; Carrick, KS.; Carr, BR. (Mar 2009). "Virilization persists in a woman with an androgen-secreting granulosa cell tumor.". Fertil Steril 91 (3): 933.e13-5. doi:10.1016/j.fertnstert.2008.10.038. PMID 19062005.
- ↑ Havelock, JC.; Rainey, WE.; Carr, BR. (Dec 2004). "Ovarian granulosa cell lines.". Mol Cell Endocrinol 228 (1-2): 67-78. doi:10.1016/j.mce.2004.04.018. PMID 15541573.
- ↑ Kommoss, S.; Anglesio, MS.; Mackenzie, R.; Yang, W.; Senz, J.; Ho, J.; Bell, L.; Lee, S. et al. (Jun 2013). "FOXL2 molecular testing in ovarian neoplasms: diagnostic approach and procedural guidelines.". Mod Pathol 26 (6): 860-7. doi:10.1038/modpathol.2012.226. PMID 23348906.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1102. ISBN 0-7216-0187-1.
- ↑ Jamieson, S.; Fuller, PJ. (Feb 2012). "Molecular pathogenesis of granulosa cell tumors of the ovary.". Endocr Rev 33 (1): 109-44. doi:10.1210/er.2011-0014. PMID 22240241.
- ↑ Shah, SP.; Köbel, M.; Senz, J.; Morin, RD.; Clarke, BA.; Wiegand, KC.; Leung, G.; Zayed, A. et al. (Jun 2009). "Mutation of FOXL2 in granulosa-cell tumors of the ovary.". N Engl J Med 360 (26): 2719-29. doi:10.1056/NEJMoa0902542. PMID 19516027.