Difference between revisions of "Low-grade squamous intraepithelial lesion"
Jump to navigation
Jump to search
| Line 50: | Line 50: | ||
*[[High-grade squamous intraepithelial lesion]]. | *[[High-grade squamous intraepithelial lesion]]. | ||
*[[Uterine cervix with reactive changes]]. | *[[Uterine cervix with reactive changes]]. | ||
===Koilocytes versus benign squamous=== | |||
Koilocytes: | |||
*Perinuclear clearing. | |||
*Nuclear changes. | |||
**Size similar (or larger) to those in the basal layer of the epithelium. | |||
**Nuclear enlargement should be evident on low power, i.e. 25x. <ref>V. Dube 2008.</ref> | |||
**Central location - nucleus should be smack in the middle of the cell. | |||
Notes: | |||
# Both perinuclear clearing and nuclear changes are essential. | |||
# Benign cells have a small nucleus that is peripheral. | |||
===Images=== | |||
<gallery> | |||
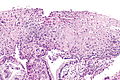
Image: Low-grade squamous intraepithelial lesion -- intermed mag.jpg | LSIL - intermed. mag. (WC) | |||
Image: Low-grade squamous intraepithelial lesion -- p16 - intermed mag.jpg | LSIL - intermed. mag. (WC) | |||
Image: Low-grade squamous intraepithelial lesion -- high mag.jpg | LSIL - high mag. (WC) | |||
Image: Low-grade squamous intraepithelial lesion -- very high mag.jpg | LSIL - very high mag. (WC) | |||
</gallery> | |||
<gallery> | |||
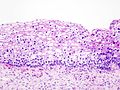
Image:Cervical intraepithelial neoplasia (2) koilocytosis.jpg| CIN I. (WC/KGH) | |||
</gallery> | |||
www: | |||
*[http://www.flickr.com/photos/jian-hua_qiao_md/3987000055/ CIN 1 (flickr.com/Qiao)]. | |||
*[http://www.eurocytology.eu/static/eurocytology/eng/cervical/mod6img1a.html CIN 1 (eurocytology.eu)]. | |||
==See also== | ==See also== | ||
Revision as of 19:50, 30 January 2014
Low-grade squamous intraepithelial lesion, abbreviated LSIL, is a pre-cancerous lesions of the uterine cervix.
Increasingly, the term is being applied to other anatomical sites, e.g. vagina.
It is in the larger category of squamous intraepithelial lesion, abbreviated SIL.
General
- Precursor lesion of cervical squamous cell carcinoma.
- Usually associated with human papilloma virus.
SIL is divided into grades:
- Low-grade.
- High-grade.
The new and old terminology
| SIL (current terminology) | LSIL | HSIL |
|---|---|---|
| Recent terminology | CIN I | CIN II, CIN III |
| Very old terminology | mild dysplasia | moderate dysplasia, severe dysplasia |
Treatment
Overview:
- LSIL: follow-up unless persistent. It usually regresses on its own.
Microscopic
Features:[1]
- "Koilocytic atypia":[2]
Note:
- Atypical cells usually close to basement membrane.
- May be seen, focally, in the upper layers.[2]
DDx:
Koilocytes versus benign squamous
Koilocytes:
- Perinuclear clearing.
- Nuclear changes.
- Size similar (or larger) to those in the basal layer of the epithelium.
- Nuclear enlargement should be evident on low power, i.e. 25x. [4]
- Central location - nucleus should be smack in the middle of the cell.
Notes:
- Both perinuclear clearing and nuclear changes are essential.
- Benign cells have a small nucleus that is peripheral.
Images
www:
See also
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1075-6. ISBN 0-7216-0187-1.
- ↑ 2.0 2.1 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 146. ISBN 978-0443069208.
- ↑ Roteli-Martins CM, Derchain SF, Martinez EZ, Siqueira SA, Alves VA, Syrjänen KJ (2001). "Morphological diagnosis of HPV lesions and cervical intraepithelial neoplasia (CIN) is highly reproducible". Clin Exp Obstet Gynecol 28 (2): 78–80. PMID 11491378.
- ↑ V. Dube 2008.