Difference between revisions of "Gallbladder"
(→Cholelithiasis: tweak) |
|||
| (108 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
The '''gallbladder''', in pathology (and '''general surgery'''), is a growth industry... due to the worsening obesity epidemic. | The '''gallbladder''', in pathology (and '''general surgery'''), is a growth industry... due to the worsening [[obesity]] epidemic. | ||
=Normal | =Normal= | ||
* | ==Anatomy== | ||
*Body. | |||
*Fundus. | |||
*Neck. | |||
Variations: | |||
*Hartmann's pouch - invagination of the gallbladder wall at the origin of the cystic duct. | |||
Image: | |||
*[http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder_fichiers/loadBinaryCAS7X571.jpg Hartmann's pouch (uni-plovdiv.bg)].<ref>URL: [http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder.htm http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder.htm]. Accessed on: 13 December 2012.</ref> | |||
==Histology== | |||
*'''No''' muscularis mucosae. | |||
*Small amount of lymphocytes in the lamina propria. | *Small amount of lymphocytes in the lamina propria. | ||
Note: | |||
*[ | *As there is no ''muscularis mucosae'', the [[cancer staging]] is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion. | ||
===Image=== | |||
<gallery> | |||
Image:Gallbladder_-_intermed_mag.jpg | Normal gallbladder - intermed. mag. (WC/Nephron) | |||
</gallery> | |||
=Overview= | =Overview= | ||
| Line 21: | Line 37: | ||
=Common= | =Common= | ||
== | ==Chronic cholecystitis== | ||
{{Main|Chronic cholecystitis}} | |||
==== | ==Acute cholecystitis== | ||
{{Main|Acute cholecystitis}} | |||
==== | ==Gallbladder cholesterolosis== | ||
{{Main|Gallbladder cholesterolosis}} | |||
=== | ==Cholelithiasis== | ||
*[[AKA]] ''gallstones''. | |||
* | {{Main|Cholelithiasis}} | ||
= | =Less common pathologic diagnoses= | ||
==== | ==Adenomyoma of the gallbladder== | ||
*[[AKA]] ''gallbladder adenomyosis''. | |||
* | *[[AKA]] ''adenomyomatosis of the gallbladder''. | ||
*[[AKA]] ''gallbladder adenomyoma''. | |||
* | |||
* | |||
===General=== | ===General=== | ||
* | *Glands in muscle. | ||
* | *Analogous to what happens in the [[uterine adenomyosis|uterus]]. | ||
*Significance - may mimic malignant tumours of the gallbladder.<ref>{{Cite journal | last1 = Saul | first1 = WM. | last2 = Herrmann | first2 = PK. | title = [Adenomyoma of the gallbladder]. | journal = Dtsch Z Verdau Stoffwechselkr | volume = 48 | issue = 2 | pages = 112-6 | month = | year = 1988 | doi = | PMID = 3168899 }}</ref><ref name=pmid9350002 >{{Cite journal | last1 = Sasatomi | first1 = E. | last2 = Miyazaki | first2 = K. | last3 = Mori | first3 = M. | last4 = Satoh | first4 = T. | last5 = Nakano | first5 = S. | last6 = Tokunaga | first6 = O. | title = Polypoid adenomyoma of the gallbladder. | journal = J Gastroenterol | volume = 32 | issue = 5 | pages = 704-7 | month = Oct | year = 1997 | doi = | PMID = 9350002 }} | |||
</ref> | |||
*Uncommon. | |||
===Gross=== | ===Gross=== | ||
*Cystic spaces (Rokitansky-Aschoff sinuses) - may be seen on imaging.<ref name=pmid17579153>{{Cite journal | last1 = Ching | first1 = BH. | last2 = Yeh | first2 = BM. | last3 = Westphalen | first3 = AC. | last4 = Joe | first4 = BN. | last5 = Qayyum | first5 = A. | last6 = Coakley | first6 = FV. | title = CT differentiation of adenomyomatosis and gallbladder cancer. | journal = AJR Am J Roentgenol | volume = 189 | issue = 1 | pages = 62-6 | month = Jul | year = 2007 | doi = 10.2214/AJR.06.0866 | PMID = 17579153 }}</ref><ref name=pmid16702464>{{Cite journal | last1 = Boscak | first1 = AR. | last2 = Al-Hawary | first2 = M. | last3 = Ramsburgh | first3 = SR. | title = Best cases from the AFIP: Adenomyomatosis of the gallbladder. | journal = Radiographics | volume = 26 | issue = 3 | pages = 941-6 | month = | year = | doi = 10.1148/rg.263055180 | PMID = 16702464 | URL = http://radiographics.rsna.org/content/26/3/941.long}}</ref> | |||
* | *Gallbladder wall thickening. | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features:<ref name=Ref_GLP439>{{Ref GLP|439}}</ref> | ||
* | *Glands in muscularis propria of the gallbladder wall - '''key feature'''. | ||
*Significant muscular hypertrophy - '''key feature'''. | |||
*No nuclear atypia. | |||
DDx: | |||
*[http:// | *[[Gallbladder carcinoma]]. | ||
*[[Chronic cholecystitis]] - has less muscular hypertrophy; overlaps with this diagnosis.<ref name=Ref_GLP439>{{Ref GLP|439}}</ref> | |||
*Phrygian cap.<reF>URL: [http://radiopaedia.org/articles/phrygian_cap http://radiopaedia.org/articles/phrygian_cap]. Accessed on: 16 May 2014.</ref> | |||
== | ====Image==== | ||
= | *[http://pubs.rsna.org/na101/home/literatum/publisher/rsna/journals/content/radiographics/2006/radiographics.2006.26.issue-3/rg.263055180/production/images/medium/g06ma19c05x.jpeg Adenomyomatosis of the gallbladder (radiographics.rsna.org)].<ref name=pmid16702464/> | ||
* | |||
===Sign out=== | |||
<pre> | |||
GALLBLADDER, CHOLECYSTECTOMY: | |||
- CHRONIC CHOLECYSTITIS WITH MILD CHOLESTEROLOSIS AND ADENOMYOSIS (FUNDUS). | |||
- CHOLELITHIASIS. | |||
</pre> | |||
==Gallbladder polyps== | |||
* | ===General=== | ||
*Polyps are significant as they may be adenomatous, i.e. pre-cancerous. | |||
*These are similar to [[intestinal polyps|polyps]] found elsewhere GI tract. | |||
===Microscopic=== | |||
:See ''[[intestinal polyps]]''. | |||
= | Flat dysplasia:<ref name=Ref_DCHH172>{{Ref DCHH|172}}</ref> | ||
* | *Nuclear changes. | ||
**Increased [[NC ratio]]. | |||
**Hyperchromasia (essential). | |||
* | **+/-Intestinal metaplasia --> goblet cells. | ||
* | |||
* | |||
= | ==Gallbladder diverticulosis== | ||
===General=== | ===General=== | ||
* | *Uncommon. | ||
* | *Thought to arise in the context of an outflow obstruction.<ref name=pmid4963758>{{Cite journal | last1 = Beilby | first1 = JO. | title = Diverticulosis of the gall bladder. The fundal adenoma. | journal = Br J Exp Pathol | volume = 48 | issue = 4 | pages = 455-61 | month = Aug | year = 1967 | doi = | PMID = 4963758 | PMC = 2093791 | URL = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2093791/}}</ref> | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Mucosal pouch penetrating the muscularis propria of the gallbladder wall - '''key feature'''. | ||
DDx: | |||
*[[Chronic cholecystitis]]. | |||
*[[Gallbladder adenomyosis]]. | |||
== | ===Sign out=== | ||
<pre> | |||
GALLBLADDER, CHOLECYSTECTOMY: | |||
- CHRONIC CHOLECYSTITIS WITH DIVERTICULOSIS. | |||
- CHOLELITHIASIS. | |||
</pre> | |||
== | ==Xanthogranulomatous cholecystitis== | ||
* | *Abbreviated ''XGC''. | ||
{{Main|Xanthogranulomatous cholecystitis}} | |||
==Pancreatic heterotopia== | |||
[[File:Gallbladder mass benign A sl 1.png|Pancreatic heterotopia in 35 year old women]] | |||
[[File:Gallbladder mass benign A sl 2.png|Pancreatic heterotopia in 35 year old women]] | |||
[[File:Gallbladder mass benign A sl 3.png|Pancreatic heterotopia in 35 year old women]] | |||
[[File:Gallbladder mass benign A sl 4.png|Pancreatic heterotopia in 35 year old women]]<br> | |||
Pancreatic heterotopia near cystic duct in 35 year old women. A. The cystic duct margin is at right; the heterotopia, at left. This cannot be a portion of the pancreas because the cystic duct margin lies proximal to the common bile duct. B. Pancreatic ducts with lobular proliferation, but without the inflammation that would usually be present were this obstruction by a gallstone. C. Nuclei of the duct and the proliferated bile ductules are bland. D. Acini are unremarkable; no pancreatic islets were seen in this case. | |||
=Premalignant lesions | =Premalignant lesions= | ||
===General=== | |||
*Metaplasia associated with carcinoma.<ref name=pmid8364865>{{cite journal |author=Duarte I, Llanos O, Domke H, Harz C, Valdivieso V |title=Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples |journal=Cancer |volume=72 |issue=6 |pages=1878–84 |year=1993 |month=September |pmid=8364865 |doi= |url=}}</ref> | *Metaplasia associated with carcinoma.<ref name=pmid8364865>{{cite journal |author=Duarte I, Llanos O, Domke H, Harz C, Valdivieso V |title=Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples |journal=Cancer |volume=72 |issue=6 |pages=1878–84 |year=1993 |month=September |pmid=8364865 |doi= |url=}}</ref> | ||
| Line 126: | Line 139: | ||
*Antral type metaplasia --> intestinal metaplasia --> dysplasia --> carcinoma. | *Antral type metaplasia --> intestinal metaplasia --> dysplasia --> carcinoma. | ||
==Intestinal metaplasia | ==Intestinal metaplasia of the gallbladder== | ||
*[[AKA]] ''gallbladder [[intestinal metaplasia]]''. | |||
{{Main|Intestinal metaplasia of the gallbladder}} | |||
* | |||
==Antral type metaplasia== | ==Antral type metaplasia== | ||
| Line 148: | Line 156: | ||
Notes: | Notes: | ||
*May look similar to cells of the gallbladder neck<ref name=Ref_Sternberg4_1789>{{Ref Sternberg4|1789}}</ref> and common bile duct.<ref> | *May look similar to cells of the gallbladder neck<ref name=Ref_Sternberg4_1789>{{Ref Sternberg4|1789}}</ref> and common bile duct.<ref>Cutz, E. 3 March 2011.</ref> | ||
**These glandular cells are not as columnar and have less well-defined cell borders. | **These glandular cells are not as columnar and have less well-defined cell borders. | ||
***Cells with antral type metaplasia >2:1 (height:width), benign mucosal glands <2:1. | ***Cells with antral type metaplasia >2:1 (height:width), benign mucosal glands <2:1. | ||
| Line 155: | Line 163: | ||
*[http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2 Gallbladder metaplasias (archivesofpathology.org)].<ref name=pmid15737036>{{cite journal |author=Mukhopadhyay S, Landas SK |title=Putative precursors of gallbladder dysplasia: a review of 400 routinely resected specimens |journal=Arch. Pathol. Lab. Med. |volume=129 |issue=3 |pages=386–90 |year=2005 |month=March |pmid=15737036 |doi= |url=http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2 }}</ref> | *[http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2 Gallbladder metaplasias (archivesofpathology.org)].<ref name=pmid15737036>{{cite journal |author=Mukhopadhyay S, Landas SK |title=Putative precursors of gallbladder dysplasia: a review of 400 routinely resected specimens |journal=Arch. Pathol. Lab. Med. |volume=129 |issue=3 |pages=386–90 |year=2005 |month=March |pmid=15737036 |doi= |url=http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2 }}</ref> | ||
== | ===Sign out=== | ||
<pre> | |||
Gallbladder, Cholecystectomy: | |||
- Chronic cholecystitis with antral-type metaplasia, NEGATIVE for dysplasia. | |||
- Cholelithiasis. | |||
</pre> | |||
== | ==Gallbladder adenoma== | ||
:''Gallbladder dysplasia'' is covered in ''[[gallbladder adenoma]]''. | |||
{{Main|Gallbladder adenoma}} | |||
==Intracholecystic Papillary Neoplasm<ref>{{Cite journal | last1 = Adsay | first1 = V. | last2 = Jang | first2 = KT. | last3 = Roa | first3 = JC. | last4 = Dursun | first4 = N. | last5 = Ohike | first5 = N. | last6 = Bagci | first6 = P. | last7 = Basturk | first7 = O. | last8 = Bandyopadhyay | first8 = S. | last9 = Cheng | first9 = JD. | title = Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases. | journal = Am J Surg Pathol | volume = 36 | issue = 9 | pages = 1279-301 | month = Sep | year = 2012 | doi = 10.1097/PAS.0b013e318262787c | PMID = 22895264 }} | |||
</ref>== | |||
===General=== | ===General=== | ||
*Probably some overlap with 'adenoma' above | |||
* | *Lesion defined as being >1cm. | ||
* | *Low-grade lesions previously designated “papillary adenoma” | ||
* | *High-grade lesions previously designated “noninvasive papillary carcinoma.” | ||
*Oten arise in a background of pyloric-gland metaplasia. | |||
*May be associated with invasive adenocarcinoma, which should be reported as intracystic papillary neoplasm with an associated invasive carcinoma and staged. | |||
*Population | |||
* | **Female (F/M=2:1) | ||
* | **Mean age 61 | ||
*Presentations | |||
**Pain | |||
**Incidental | |||
*No particular association with gallstones. | |||
===Microscopic=== | ===Microscopic=== | ||
*Cell types | |||
* | **Pancreatobiliary type | ||
** | **Intestinal types with goblet, Paneth, and/or serotonin-containing cells. | ||
*Architecture | |||
**Papillary | |||
**Tubulopapillary | |||
**Tubular | |||
*Dysplasia - high or low grade | |||
<gallery> | |||
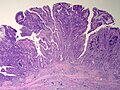
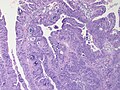
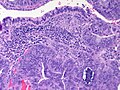
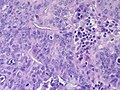
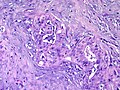
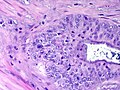
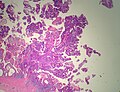
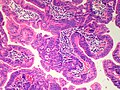
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma LP CTR.jpg|Gall Bladder - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - Low power (SKB) | |||
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma HP CTR.jpg|Gall Bladder - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - High power (SKB) | |||
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma HP3 CTR.jpg|Gall Bladder - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - High power (SKB) | |||
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma HP2 CTR.jpg|Gall Bladder - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - High power (SKB) | |||
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma MP CTR.jpg|Gall Bladder - - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - Malignant gland infiltrating stroma - High power (SKB) | |||
Image:GallBladder IntracysticPapillaryNeoplasm WA InvasiveAdenocarcinoma HP4 CTR.jpg|Gall Bladder - Intracholecystic Papillary Neoplasm with Invasive Adenocarcinoma - - Malignant gland infiltrating stroma - Very high power (SKB) | |||
Image:Gallbladder IntracysticPapillaryNeoplasm HighGradeDysplasia LP PA.JPG|Gall Bladder - Intracholecystic Papillary Neoplasm with high grade dysplasia - Low power (SKB) | |||
Image:Gallbladder IntracysticPapillaryNeoplasm HighGradeDysplasia MP PA.JPG|Gall Bladder - Intracholecystic Papillary Neoplasm with high grade dysplasia - Medium power (SKB) | |||
</gallery> | |||
Notes: | Notes: | ||
All of the gallbladder should be submitted prior to sign out to exclude invasive adenocarcinoma. | |||
=Malignant= | |||
==Gallbladder carcinoma== | |||
{{Main|Gallbladder carcinoma}} | |||
=See also= | =See also= | ||
| Line 192: | Line 228: | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Gallbladder]] | |||
[[Category:Gastrointestinal pathology]] | [[Category:Gastrointestinal pathology]] | ||
Latest revision as of 14:06, 30 October 2017
The gallbladder, in pathology (and general surgery), is a growth industry... due to the worsening obesity epidemic.
Normal
Anatomy
- Body.
- Fundus.
- Neck.
Variations:
- Hartmann's pouch - invagination of the gallbladder wall at the origin of the cystic duct.
Image:
Histology
- No muscularis mucosae.
- Small amount of lymphocytes in the lamina propria.
Note:
- As there is no muscularis mucosae, the cancer staging is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion.
Image
Overview
Most common:
- Cholelithiasis with cholecystitis.
Common:
- Antral-type metaplasia.
Uncommon:
- Intestinal metaplasia.
- Gallbladder dysplasia.
- Gallbladder carcinoma.
Common
Chronic cholecystitis
Acute cholecystitis
Gallbladder cholesterolosis
Cholelithiasis
- AKA gallstones.
Less common pathologic diagnoses
Adenomyoma of the gallbladder
General
- Glands in muscle.
- Analogous to what happens in the uterus.
- Significance - may mimic malignant tumours of the gallbladder.[2][3]
- Uncommon.
Gross
- Cystic spaces (Rokitansky-Aschoff sinuses) - may be seen on imaging.[4][5]
- Gallbladder wall thickening.
Microscopic
Features:[6]
- Glands in muscularis propria of the gallbladder wall - key feature.
- Significant muscular hypertrophy - key feature.
- No nuclear atypia.
DDx:
- Gallbladder carcinoma.
- Chronic cholecystitis - has less muscular hypertrophy; overlaps with this diagnosis.[6]
- Phrygian cap.[7]
Image
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH MILD CHOLESTEROLOSIS AND ADENOMYOSIS (FUNDUS). - CHOLELITHIASIS.
Gallbladder polyps
General
- Polyps are significant as they may be adenomatous, i.e. pre-cancerous.
- These are similar to polyps found elsewhere GI tract.
Microscopic
- See intestinal polyps.
Flat dysplasia:[8]
- Nuclear changes.
- Increased NC ratio.
- Hyperchromasia (essential).
- +/-Intestinal metaplasia --> goblet cells.
Gallbladder diverticulosis
General
- Uncommon.
- Thought to arise in the context of an outflow obstruction.[9]
Microscopic
Features:
- Mucosal pouch penetrating the muscularis propria of the gallbladder wall - key feature.
DDx:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH DIVERTICULOSIS. - CHOLELITHIASIS.
Xanthogranulomatous cholecystitis
- Abbreviated XGC.
Pancreatic heterotopia
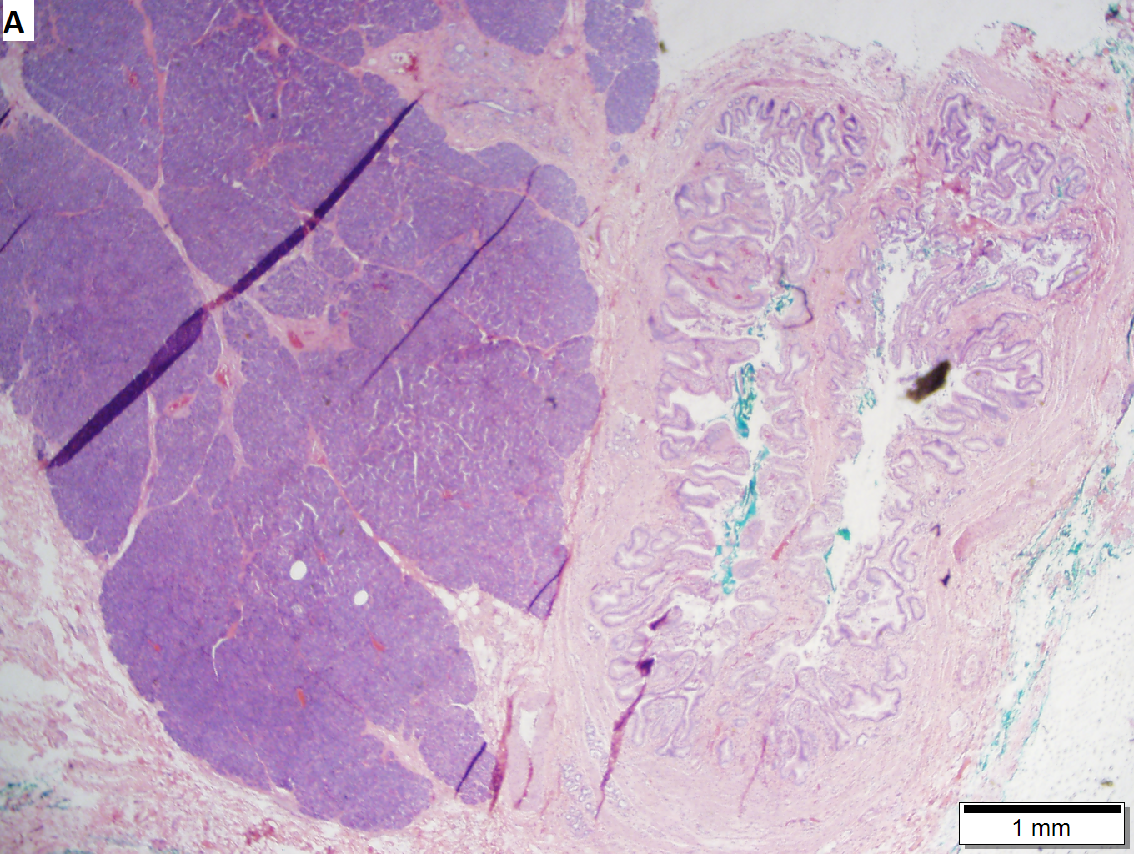
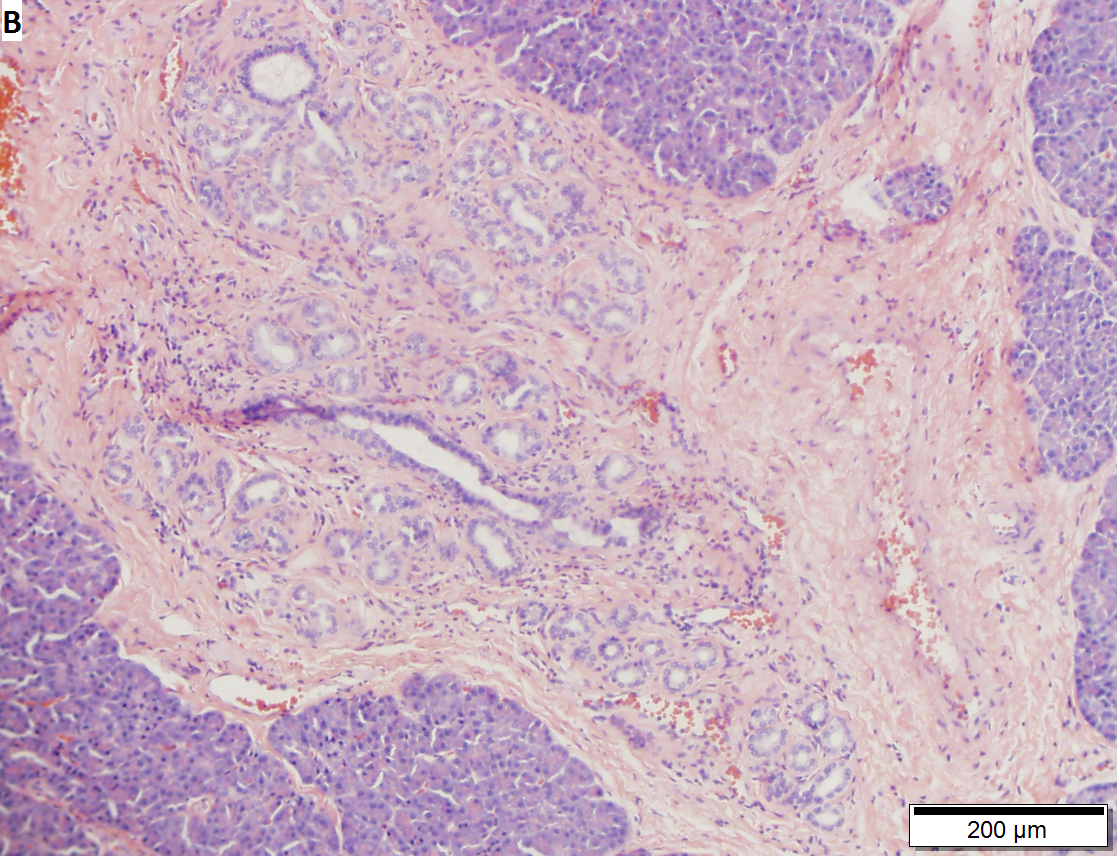


Pancreatic heterotopia near cystic duct in 35 year old women. A. The cystic duct margin is at right; the heterotopia, at left. This cannot be a portion of the pancreas because the cystic duct margin lies proximal to the common bile duct. B. Pancreatic ducts with lobular proliferation, but without the inflammation that would usually be present were this obstruction by a gallstone. C. Nuclei of the duct and the proliferated bile ductules are bland. D. Acini are unremarkable; no pancreatic islets were seen in this case.
Premalignant lesions
General
- Metaplasia associated with carcinoma.[10]
Hypothesis:[11]
- Antral type metaplasia --> intestinal metaplasia --> dysplasia --> carcinoma.
Intestinal metaplasia of the gallbladder
- AKA gallbladder intestinal metaplasia.
Antral type metaplasia
General
Microscopic
Features:[12]
- Columnar cells with:
- Abundant, pale, apical mucin.
- Small basal nucleus.
- Cells often in nests -- below luminal surface.
- Cells vaguely resemble foveollar epithelium of the stomach.
Notes:
- May look similar to cells of the gallbladder neck[12] and common bile duct.[13]
- These glandular cells are not as columnar and have less well-defined cell borders.
- Cells with antral type metaplasia >2:1 (height:width), benign mucosal glands <2:1.
- These glandular cells are not as columnar and have less well-defined cell borders.
Images:
Sign out
Gallbladder, Cholecystectomy: - Chronic cholecystitis with antral-type metaplasia, NEGATIVE for dysplasia. - Cholelithiasis.
Gallbladder adenoma
- Gallbladder dysplasia is covered in gallbladder adenoma.
Intracholecystic Papillary Neoplasm[14]
General
- Probably some overlap with 'adenoma' above
- Lesion defined as being >1cm.
- Low-grade lesions previously designated “papillary adenoma”
- High-grade lesions previously designated “noninvasive papillary carcinoma.”
- Oten arise in a background of pyloric-gland metaplasia.
- May be associated with invasive adenocarcinoma, which should be reported as intracystic papillary neoplasm with an associated invasive carcinoma and staged.
- Population
- Female (F/M=2:1)
- Mean age 61
- Presentations
- Pain
- Incidental
- No particular association with gallstones.
Microscopic
- Cell types
- Pancreatobiliary type
- Intestinal types with goblet, Paneth, and/or serotonin-containing cells.
- Architecture
- Papillary
- Tubulopapillary
- Tubular
- Dysplasia - high or low grade
Notes: All of the gallbladder should be submitted prior to sign out to exclude invasive adenocarcinoma.
Malignant
Gallbladder carcinoma
See also
References
- ↑ URL: http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder.htm. Accessed on: 13 December 2012.
- ↑ Saul, WM.; Herrmann, PK. (1988). "[Adenomyoma of the gallbladder].". Dtsch Z Verdau Stoffwechselkr 48 (2): 112-6. PMID 3168899.
- ↑ Sasatomi, E.; Miyazaki, K.; Mori, M.; Satoh, T.; Nakano, S.; Tokunaga, O. (Oct 1997). "Polypoid adenomyoma of the gallbladder.". J Gastroenterol 32 (5): 704-7. PMID 9350002.
- ↑ Ching, BH.; Yeh, BM.; Westphalen, AC.; Joe, BN.; Qayyum, A.; Coakley, FV. (Jul 2007). "CT differentiation of adenomyomatosis and gallbladder cancer.". AJR Am J Roentgenol 189 (1): 62-6. doi:10.2214/AJR.06.0866. PMID 17579153.
- ↑ 5.0 5.1 Boscak, AR.; Al-Hawary, M.; Ramsburgh, SR.. "Best cases from the AFIP: Adenomyomatosis of the gallbladder.". Radiographics 26 (3): 941-6. doi:10.1148/rg.263055180. PMID 16702464.
- ↑ 6.0 6.1 Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 439. ISBN 978-0443066573.
- ↑ URL: http://radiopaedia.org/articles/phrygian_cap. Accessed on: 16 May 2014.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 172. ISBN 978-0470519035.
- ↑ Beilby, JO. (Aug 1967). "Diverticulosis of the gall bladder. The fundal adenoma.". Br J Exp Pathol 48 (4): 455-61. PMC 2093791. PMID 4963758. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2093791/.
- ↑ Duarte I, Llanos O, Domke H, Harz C, Valdivieso V (September 1993). "Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples". Cancer 72 (6): 1878–84. PMID 8364865.
- ↑ 11.0 11.1 Mukhopadhyay S, Landas SK (March 2005). "Putative precursors of gallbladder dysplasia: a review of 400 routinely resected specimens". Arch. Pathol. Lab. Med. 129 (3): 386–90. PMID 15737036. http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2.
- ↑ 12.0 12.1 12.2 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 1789. ISBN 978-0781740517.
- ↑ Cutz, E. 3 March 2011.
- ↑ Adsay, V.; Jang, KT.; Roa, JC.; Dursun, N.; Ohike, N.; Bagci, P.; Basturk, O.; Bandyopadhyay, S. et al. (Sep 2012). "Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases.". Am J Surg Pathol 36 (9): 1279-301. doi:10.1097/PAS.0b013e318262787c. PMID 22895264.