Difference between revisions of "Pseudomelanosis coli"
Jump to navigation
Jump to search
(redirect) |
(→General: wikify) |
||
| (19 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Melanosis_coli_intermed_mag.jpg | |||
| Width = | |||
| Caption = Pseudomelanosis coli. [[H&E stain]]. | |||
| Synonyms = melanosis coli | |||
| Micro = brown granular pigment in the lamina propria, abundant | |||
| Subtypes = | |||
| LMDDx = hemorrhage, [[melanocytic lesion]] (rarely) | |||
| Stains = [[PAS stain|PAS]] +ve, [[Prussian blue stain|Prussian blue]] -ve, [[Fontana-Masson stain|Fontana-Masson]] +ve | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[colon]], [[cecum]], occasionally [[small intestine]] | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = use of laxatives and herbals | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = brown discolouration of the mucosa, esp. proximal colon and cecum | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = [[colitis]] | |||
}} | |||
{{ Infobox external links | |||
| Name = {{PAGENAME}} | |||
| EHVSC = | |||
| EHVSC_mult = | |||
| pathprotocols = | |||
| wikipedia = melanosis coli | |||
| pathoutlines = | |||
}} | |||
'''Pseudomelanosis coli''', also known as '''melanosis coli''',<ref>URL: [http://www.medicinenet.com/melanosis_coli/article.htm http://www.medicinenet.com/melanosis_coli/article.htm]. Accessed on: 4 March 2011.</ref> is a relatively common benign change seen in the [[colon]]. | |||
==General== | |||
*''Not melanin'' as the name ''melanosis coli'' suggests; it is actually [[lipofuscin]] (in macrophages).<ref name=pmid18666316>{{cite journal |author=Freeman HJ |title="Melanosis" in the small and large intestine |journal=World J. Gastroenterol. |volume=14 |issue=27 |pages=4296-9 |year=2008 |month=July |pmid=18666316 |doi= |url=http://www.wjgnet.com/1007-9327/14/4296.asp}}</ref> | |||
*Endoscopist may see brown pigmentation of mucosa and suspect the diagnosis. | |||
*Presence may lead to endoscopic misinterpretation of colitis severity.<ref name=pmid21375218>{{Cite journal | last1 = Zapatier | first1 = JA. | last2 = Schneider | first2 = A. | last3 = Parra | first3 = JL. | title = Overestimation of ulcerative colitis due to melanosis coli. | journal = Acta Gastroenterol Latinoam | volume = 40 | issue = 4 | pages = 351-3 | month = Dec | year = 2010 | doi = | PMID = 21375218 }}</ref> | |||
===Epidemiology=== | |||
*Classically associated with anthracene containing laxative (e.g. Senokot) use and herbal remedies.<ref name=pmid18666316/> | |||
**May be seen in individuals not using laxatives.<ref name=pmid9600362/> | |||
*Seen in (long-standing) [[inflammatory bowel disease]], especially [[ulcerative colitis]].<ref name=pmid9600362>{{Cite journal | last1 = Pardi | first1 = DS. | last2 = Tremaine | first2 = WJ. | last3 = Rothenberg | first3 = HJ. | last4 = Batts | first4 = KP. | title = Melanosis coli in inflammatory bowel disease. | journal = J Clin Gastroenterol | volume = 26 | issue = 3 | pages = 167-70 | month = Apr | year = 1998 | doi = | PMID = 9600362 }}</ref> | |||
==Gross== | |||
*Brown pigmentation of the mucosa, especially cecum and proximal colon.<ref name=pmid18666316/> | |||
**Less pigmentation distal. | |||
Note: | |||
*May also been seen in the [[small intestine]].<ref name=pmid18666316>{{cite journal |author=Freeman HJ |title="Melanosis" in the small and large intestine |journal=World J. Gastroenterol. |volume=14 |issue=27 |pages=4296-9 |year=2008 |month=July |pmid=18666316 |doi= |url=http://www.wjgnet.com/1007-9327/14/4296.asp}}</ref> | |||
===Endoscopic image=== | |||
<gallery> | |||
Image:Melanosis_coli.jpg | Melanosis coli - endoscopic image. (WC) | |||
</gallery> | |||
==Microscopic== | |||
Features: | |||
*Brown granular pigment - in the lamina propria. | |||
**Typically more prominent in the cecum and proximal colon.<ref name=pmid18666316/> | |||
Notes: | |||
*DDx of brown pigment: | |||
**Lipofuscin - comes with age (can be demonstrated with a ''[[PAS stain]]''<ref name=pmid5463681 >{{cite journal |author=Kovi J, Leifer C |title=Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse |journal=J Natl Med Assoc |volume=62 |issue=4 |pages=287–90 |year=1970 |month=July |pmid=5463681 |pmc=2611776 |doi= |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf}}</ref> or ''[[Kluver-Barrera stain]]''<ref>URL: [http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exkluvbarr.htm http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exkluvbarr.htm]. Accessed on: 5 May 2010.</ref>). | |||
***Melanosis coli. | |||
**Old haemorrhage, i.e. hemosiderin-laden macrophages (may be demonstrated with ''[[Prussian blue stain]]''<ref>URL: [http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exprussb.htm http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exprussb.htm]. Accessed on: 5 May 2010.</ref>). | |||
**Melanin (from melanocytes) - rare in colon (may be demonstrated with a ''[[Fontana-Masson stain]]''<ref>URL: [http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exfontana.htm http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exfontana.htm]. Accessed on: 5 May 2010.</ref>). | |||
***Fontana-Masson ''not'' useful for differentiating from pseudomelanosis, as pseudomelanosis is Fontana-Masson positive.<ref name=pmid2346038>{{Cite journal | last1 = Park | first1 = C. | last2 = Cho | first2 = NH. | last3 = Jeong | first3 = HJ. | title = Melanosis coli--histochemical and immunohistochemical comparison of the pigments of melanosis coli and Dubin-Johnson syndrome. | journal = Yonsei Med J | volume = 31 | issue = 1 | pages = 27-32 | month = Mar | year = 1990 | doi = | PMID = 2346038 }}</ref> | |||
**Foreign material (e.g. tattoo pigment) - not seen in GI tract. | |||
===Images=== | |||
<gallery> | |||
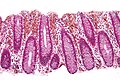
Image:Melanosis_coli_low_mag.jpg | Melanosis coli - low mag. (WC/Nephron) | |||
Image:Melanosis_coli_intermed_mag.jpg | Melanosis coli - intermed. mag. (WC/Nephron) | |||
Image:Melanosis_coli_high_mag.jpg | Melanosis coli - high mag. (WC/Nephron) | |||
</gallery> | |||
Another case: | |||
<gallery> | |||
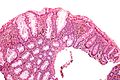
Image:Pseudomelanosis coli - intermed mag.jpg | Melanosis coli - intermed. mag. (WC/Nephron) | |||
Image:Pseudomelanosis coli - high mag.jpg | Melanosis coli - high mag. (WC/Nephron) | |||
Image:Pseudomelanosis coli - very high mag.jpg | Melanosis coli - very high mag. (WC/Nephron) | |||
</gallery> | |||
==Stains== | |||
*Can be demonstrated with a [[PAS stain]].<ref name=pmid9283862>{{cite journal |author=Benavides SH, Morgante PE, Monserrat AJ, Zárate J, Porta EA |title=The pigment of melanosis coli: a lectin histochemical study |journal=Gastrointest. Endosc. |volume=46 |issue=2 |pages=131–8 |year=1997 |month=August |pmid=9283862 |doi= |url=}}</ref> | |||
Note: | |||
*[[Fontana-Masson stain]] is ''not'' useful for differentiating pseudomelanosis from true melanin pigment, as pseudomelanosis is Fontana-Masson positive.<ref name=pmid2346038>{{Cite journal | last1 = Park | first1 = C. | last2 = Cho | first2 = NH. | last3 = Jeong | first3 = HJ. | title = Melanosis coli--histochemical and immunohistochemical comparison of the pigments of melanosis coli and Dubin-Johnson syndrome. | journal = Yonsei Med J | volume = 31 | issue = 1 | pages = 27-32 | month = Mar | year = 1990 | doi = | PMID = 2346038 }}</ref> | |||
==Sign out== | |||
<pre> | |||
ASCENDING COLON, BIOPSY: | |||
- PSEUDOMELANOSIS COLI. | |||
- NEGATIVE FOR ACTIVE COLITIS. | |||
- NEGATIVE FOR DYSPLASIA. | |||
</pre> | |||
==See also== | |||
*[[Gastrointestinal pathology]]. | |||
*[[Colon]]. | |||
*[[Small bowel pseudomelanosis]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Colon]] | |||
Latest revision as of 18:08, 24 May 2020
| Pseudomelanosis coli | |
|---|---|
| Diagnosis in short | |
 Pseudomelanosis coli. H&E stain. | |
|
| |
| Synonyms | melanosis coli |
|
| |
| LM | brown granular pigment in the lamina propria, abundant |
| LM DDx | hemorrhage, melanocytic lesion (rarely) |
| Stains | PAS +ve, Prussian blue -ve, Fontana-Masson +ve |
| Site | colon, cecum, occasionally small intestine |
|
| |
| Clinical history | use of laxatives and herbals |
| Endoscopy | brown discolouration of the mucosa, esp. proximal colon and cecum |
| Prognosis | benign |
| Clin. DDx | colitis |
| Pseudomelanosis coli | |
|---|---|
| External resources | |
| Wikipedia | melanosis coli |
Pseudomelanosis coli, also known as melanosis coli,[1] is a relatively common benign change seen in the colon.
General
- Not melanin as the name melanosis coli suggests; it is actually lipofuscin (in macrophages).[2]
- Endoscopist may see brown pigmentation of mucosa and suspect the diagnosis.
- Presence may lead to endoscopic misinterpretation of colitis severity.[3]
Epidemiology
- Classically associated with anthracene containing laxative (e.g. Senokot) use and herbal remedies.[2]
- May be seen in individuals not using laxatives.[4]
- Seen in (long-standing) inflammatory bowel disease, especially ulcerative colitis.[4]
Gross
- Brown pigmentation of the mucosa, especially cecum and proximal colon.[2]
- Less pigmentation distal.
Note:
- May also been seen in the small intestine.[2]
Endoscopic image
Microscopic
Features:
- Brown granular pigment - in the lamina propria.
- Typically more prominent in the cecum and proximal colon.[2]
Notes:
- DDx of brown pigment:
- Lipofuscin - comes with age (can be demonstrated with a PAS stain[5] or Kluver-Barrera stain[6]).
- Melanosis coli.
- Old haemorrhage, i.e. hemosiderin-laden macrophages (may be demonstrated with Prussian blue stain[7]).
- Melanin (from melanocytes) - rare in colon (may be demonstrated with a Fontana-Masson stain[8]).
- Fontana-Masson not useful for differentiating from pseudomelanosis, as pseudomelanosis is Fontana-Masson positive.[9]
- Foreign material (e.g. tattoo pigment) - not seen in GI tract.
- Lipofuscin - comes with age (can be demonstrated with a PAS stain[5] or Kluver-Barrera stain[6]).
Images
Another case:
Stains
Note:
- Fontana-Masson stain is not useful for differentiating pseudomelanosis from true melanin pigment, as pseudomelanosis is Fontana-Masson positive.[9]
Sign out
ASCENDING COLON, BIOPSY: - PSEUDOMELANOSIS COLI. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA.
See also
References
- ↑ URL: http://www.medicinenet.com/melanosis_coli/article.htm. Accessed on: 4 March 2011.
- ↑ 2.0 2.1 2.2 2.3 2.4 Freeman HJ (July 2008). ""Melanosis" in the small and large intestine". World J. Gastroenterol. 14 (27): 4296-9. PMID 18666316. http://www.wjgnet.com/1007-9327/14/4296.asp.
- ↑ Zapatier, JA.; Schneider, A.; Parra, JL. (Dec 2010). "Overestimation of ulcerative colitis due to melanosis coli.". Acta Gastroenterol Latinoam 40 (4): 351-3. PMID 21375218.
- ↑ 4.0 4.1 Pardi, DS.; Tremaine, WJ.; Rothenberg, HJ.; Batts, KP. (Apr 1998). "Melanosis coli in inflammatory bowel disease.". J Clin Gastroenterol 26 (3): 167-70. PMID 9600362.
- ↑ Kovi J, Leifer C (July 1970). "Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse". J Natl Med Assoc 62 (4): 287–90. PMC 2611776. PMID 5463681. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exkluvbarr.htm. Accessed on: 5 May 2010.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exprussb.htm. Accessed on: 5 May 2010.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exfontana.htm. Accessed on: 5 May 2010.
- ↑ 9.0 9.1 Park, C.; Cho, NH.; Jeong, HJ. (Mar 1990). "Melanosis coli--histochemical and immunohistochemical comparison of the pigments of melanosis coli and Dubin-Johnson syndrome.". Yonsei Med J 31 (1): 27-32. PMID 2346038.
- ↑ Benavides SH, Morgante PE, Monserrat AJ, Zárate J, Porta EA (August 1997). "The pigment of melanosis coli: a lectin histochemical study". Gastrointest. Endosc. 46 (2): 131–8. PMID 9283862.