Difference between revisions of "Neurofibromatosis"
Jump to navigation
Jump to search
(→Neurofibromatosis type 1: reorder) |
|||
| (27 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'''Neurofibromatosis''' | '''Neurofibromatosis''' is a genetic conditions, also known as '''von Recklinghausen's disease'''. It is abbreviated as '''NF'''. | ||
It comes in | It comes in several flavours: | ||
#NF1 (peripheral). | #Neurofibromatosis type 1 - NF1 (peripheral). | ||
#NF2 (central). | #Neurofibromatosis type 2 - NF2 (central). | ||
#Neurofibromatosis type 3 - Schwannomatosis. | |||
== | ==Neurofibromatosis type 1== | ||
*Autosomal dominant. | |||
===Diagnosis=== | |||
Features (need 2/7 to diagnose):<ref>URL: [http://emedicine.medscape.com/article/1177266-overview http://emedicine.medscape.com/article/1177266-overview]. Accessed on: 3 May 2010.</ref> | Features (need 2/7 to diagnose):<ref>URL: [http://emedicine.medscape.com/article/1177266-overview http://emedicine.medscape.com/article/1177266-overview]. Accessed on: 3 May 2010.</ref> | ||
#Two or more [[neurofibroma]]s or one [[plexiform neurofibroma]]. | |||
*Café-au-lait spots. | #*May give rise to a [[malignant peripheral nerve sheath tumour]]. | ||
#Café-au-lait spots. | |||
#Freckles in axilla or inguinal area. | |||
#Optic nerve glioma. | |||
#Iris hamartomas (Lisch nodules). | |||
#Sphenoid dysplasia or typical long-bone abnormalities (e.g. bowing). | |||
#First-degree relative with NF1. | |||
===Mnemonic=== | ====Mnemonic==== | ||
''CAFE SPOT'':<ref>URL: [http://www.paeds.co.uk/wiki/index.php?title=Mnemonics#Neurofibromatosis_Type_1_diagnostic_criteria http://www.paeds.co.uk/wiki/index.php?title=Mnemonics#Neurofibromatosis_Type_1_diagnostic_criteria]. Accessed on: 30 May 2011.</ref> | Diagnostic criteria ''CAFE SPOT'':<ref>URL: [http://www.paeds.co.uk/wiki/index.php?title=Mnemonics#Neurofibromatosis_Type_1_diagnostic_criteria http://www.paeds.co.uk/wiki/index.php?title=Mnemonics#Neurofibromatosis_Type_1_diagnostic_criteria]. Accessed on: 30 May 2011.</ref> | ||
* '''C'''afé-au-lait spots. | * '''C'''afé-au-lait spots. | ||
* '''A'''xillary or inguinal freckling. | * '''A'''xillary or inguinal freckling. | ||
| Line 22: | Line 27: | ||
* '''E'''ye hamartomas (Lisch nodules). | * '''E'''ye hamartomas (Lisch nodules). | ||
* '''S'''keletal abnormalities, e.g. ''s''phenoid dysplasia, leg bowing. | * '''S'''keletal abnormalities, e.g. ''s''phenoid dysplasia, leg bowing. | ||
* '''P'''ositive family history. | * '''P'''ositive family history. † | ||
* '''O'''ptic '''T'''umour (optic nerve glioma). | * '''O'''ptic '''T'''umour (optic nerve glioma). | ||
==NF2== | Note: | ||
* † One could include ''paraganglioma'' here. | |||
===Other associations=== | |||
*[[Pancreatic neuroendocrine tumour]].<ref name=pmid15249710>{{Cite journal | last1 = Alexakis | first1 = N. | last2 = Connor | first2 = S. | last3 = Ghaneh | first3 = P. | last4 = Lombard | first4 = M. | last5 = Smart | first5 = HL. | last6 = Evans | first6 = J. | last7 = Hughes | first7 = M. | last8 = Garvey | first8 = CJ. | last9 = Vora | first9 = J. | title = Hereditary pancreatic endocrine tumours. | journal = Pancreatology | volume = 4 | issue = 5 | pages = 417-33; discussion 434-5 | month = | year = 2004 | doi = 10.1159/000079616 | PMID = 15249710 }}</ref> | |||
*[[Gastrointestinal stromal tumour]].<ref name=pmid20848108>{{cite journal |author=Agaimy A, Hartmann A |title=[Hereditary and non-hereditary syndromic gastointestinal stromal tumours] |language=German |journal=Pathologe |volume=31 |issue=6 |pages=430–7 |year=2010 |month=October |pmid=20848108 |doi=10.1007/s00292-010-1354-6 |url=}}</ref> | |||
*[[Glomus tumour]].<ref name=pmid25426397>{{cite journal |authors=Harrison B, Sammer D |title=Glomus tumors and neurofibromatosis: a newly recognized association |journal=Plast Reconstr Surg Glob Open |volume=2 |issue=9 |pages=e214 |date=September 2014 |pmid=25426397 |pmc=4229273 |doi=10.1097/GOX.0000000000000144 |url=}}</ref> | |||
===Possible association=== | |||
*[[Gangliocytic paraganglioma]].<ref name=pmid12754392>{{Cite journal | last1 = Castoldi | first1 = L. | last2 = De Rai | first2 = P. | last3 = Marini | first3 = A. | last4 = Ferrero | first4 = S. | last5 = De Luca | first5 = V. | last6 = Tiberio | first6 = G. | title = Neurofibromatosis-1 and Ampullary Gangliocytic Paraganglioma Causing Biliary and Pancreatic Obstruction. | journal = Int J Gastrointest Cancer | volume = 29 | issue = 2 | pages = 93-98 | month = | year = 2001 | doi = | PMID = 12754392 }}</ref> | |||
===Images=== | |||
<gallery> | |||
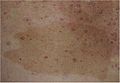
File:Early_neurofibromatosis.jpg | Café-au-lait spot (WC/Haymanj) | |||
File:NF-1-Tache_cafe-au-lait.jpg | Café-au-lait spot (WC/Accrochoc) | |||
File:Lisch_nodules.gif | Lisch nodule (iris hamartoma) in the eye (WC/filip em) | |||
File:Neurofibroma03.jpg | Multiple neurofibromas of the skin in NF1 (WC/Enigma51) | |||
File:Neurofibroma02.jpg | Multiple neurofibromas of the skin in NF1 (WC/Enigma51) | |||
File:Neurofibroma_large_NF1.jpg | Large neurofibroma in a NF1 case (WC/jensflorian) | |||
File:Neurofibromatosis,_bowel.jpg | Neurofibromatosis in the bowel (WC/Dr. Robertson) | |||
File:MPNST Pathology gross.jpg | Malignant peripheral nerve sheath tumor of the forearm (WC/drbloodmoney) | |||
</gallery> | |||
==Neurofibromatosis type 2== | |||
*Caused by mutations in the ''NF2 gene'';<ref name=omim101000>{{OMIM|101000}}</ref> this gene is also known as ''merlin''.<ref name=omim607379>{{OMIM|607379}}</ref> | |||
*Reduced life expectancy. | |||
*Mean age at diagnosis: 35years. | |||
===Diagnosis=== | |||
Features (need 1/3 to diagnose):<ref>URL: [http://emedicine.medscape.com/article/1178283-overview http://emedicine.medscape.com/article/1178283-overview]. Accessed on: 3 May 2010.</ref> | Features (need 1/3 to diagnose):<ref>URL: [http://emedicine.medscape.com/article/1178283-overview http://emedicine.medscape.com/article/1178283-overview]. Accessed on: 3 May 2010.</ref> | ||
#Bilateral CNVIII masses on imaging. | #Bilateral CNVIII masses on imaging. | ||
#Unilateral CNVIII mass + first-degree relative with NF2. | #Unilateral CNVIII mass + first-degree relative with NF2. | ||
#First-degree relative with NF2 ''and'' 2/4 of the following: | #First-degree relative with NF2 ''and'' 2/4 of the following: | ||
## [[Meningioma]] (meningothelial meningioma).<ref>URL: [http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm]. Accessed on: 26 October 2010.</ref> | ## [[Meningioma]] (meningothelial meningioma) up to 50% of the cases.<ref>URL: [http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm]. Accessed on: 26 October 2010.</ref> | ||
## Glioma. | ## Glioma, mostly spinal [[ependymoma]]s (up tp 20% of NF2 cases affected). | ||
## [[Schwannoma]]. | ## [[Schwannoma]]. | ||
## Juvenile cataract. | ## Juvenile cataract. | ||
Mnemonic ''MISME'':<ref>URL: [http://emedicine.medscape.com/article/342667-overview http://emedicine.medscape.com/article/342667-overview]. Accessed on: 20 February 2012.</ref> | |||
*'''M'''ultiple '''I'''nherited [[schwannoma|'''S'''chwannomas]]. | |||
*[[meningioma|'''M'''eningiomas]]. | |||
*[[ependymoma|'''E'''pendymomas]]. | |||
Other: | |||
*Cerebral microhamartomas. | |||
*Schwannosis (Schwann cell proliferations). | |||
*Peripheral neuropathy. | |||
===Meningioangiomatosis=== | |||
*Cortical proliferations of meningeothelial cells around small vessels. | |||
*May occur within NF2 and sporadic. | |||
*Associated with seizures and/or headaches. | |||
**Often asymptomatic. | |||
<gallery> | |||
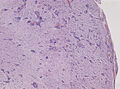
File:Meningoangiomatosis low mag.jpg | Meningioangiomatosis, low mag. (WC/jensflorian) | |||
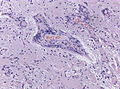
File:Meningoangiomatosis higher mag.jpg | Meningioangiomatosis, higher mag.(WC/jensflorian) | |||
</gallery> | |||
==See also== | ==See also== | ||
*[[Soft tissue lesions]]. | *[[Soft tissue lesions]]. | ||
*[[Neurocutaneous syndromes]]. | *[[Neurocutaneous syndromes]]. | ||
*[[Berry aneurysm]]. | |||
==Schwannomatosis== | |||
*Autosomal dominant. | |||
*Prevalence: 1:155000 (UK). | |||
*Distinct entity from NF2, mainly due to absence of vestibular schwannomas. | |||
*Mean age at diagnosis: 40years. | |||
*Life expectancy better compared to NF2. | |||
===Diagnosis=== | |||
Features:<ref>{{Cite journal | last1 = Evans | first1 = DG. | last2 = Bowers | first2 = NL. | last3 = Tobi | first3 = S. | last4 = Hartley | first4 = C. | last5 = Wallace | first5 = AJ. | last6 = King | first6 = AT. | last7 = Lloyd | first7 = SKW. | last8 = Rutherford | first8 = SA. | last9 = Hammerbeck-Ward | first9 = C. | title = Schwannomatosis: a genetic and epidemiological study. | journal = J Neurol Neurosurg Psychiatry | volume = | issue = | pages = | month = Jun | year = 2018 | doi = 10.1136/jnnp-2018-318538 | PMID = 29909380 }}</ref> | |||
#Two or more non-intradermal [[schwannoma]]s. | |||
#Radiological exclusion of vestibular schwannoma. | |||
#NF2-mutation excluded. | |||
#One schwannoma or meningioma and one relative with confirmed schwannomatosis. | |||
#Germline SMARCB1 or LZTR1 variant and histologically confirmed [[schwannoma]] or [[meningioma]]. | |||
===IHC=== | |||
*INI1 mosaic pattern in schwannomas.<ref>{{Cite journal | last1 = Caltabiano | first1 = R. | last2 = Magro | first2 = G. | last3 = Polizzi | first3 = A. | last4 = Praticò | first4 = AD. | last5 = Ortensi | first5 = A. | last6 = D'Orazi | first6 = V. | last7 = Panunzi | first7 = A. | last8 = Milone | first8 = P. | last9 = Maiolino | first9 = L. | title = A mosaic pattern of INI1/SMARCB1 protein expression distinguishes Schwannomatosis and NF2-associated peripheral schwannomas from solitary peripheral schwannomas and NF2-associated vestibular schwannomas. | journal = Childs Nerv Syst | volume = 33 | issue = 6 | pages = 933-940 | month = Jun | year = 2017 | doi = 10.1007/s00381-017-3340-2 | PMID = 28365909 }}</ref> | |||
==References== | ==References== | ||
{{reflist}} | {{reflist|2}} | ||
[[Category: | [[Category:Neuropathology]] | ||
[[Category:Syndromes]] | |||
Latest revision as of 14:20, 24 August 2021
Neurofibromatosis is a genetic conditions, also known as von Recklinghausen's disease. It is abbreviated as NF.
It comes in several flavours:
- Neurofibromatosis type 1 - NF1 (peripheral).
- Neurofibromatosis type 2 - NF2 (central).
- Neurofibromatosis type 3 - Schwannomatosis.
Neurofibromatosis type 1
- Autosomal dominant.
Diagnosis
Features (need 2/7 to diagnose):[1]
- Two or more neurofibromas or one plexiform neurofibroma.
- May give rise to a malignant peripheral nerve sheath tumour.
- Café-au-lait spots.
- Freckles in axilla or inguinal area.
- Optic nerve glioma.
- Iris hamartomas (Lisch nodules).
- Sphenoid dysplasia or typical long-bone abnormalities (e.g. bowing).
- First-degree relative with NF1.
Mnemonic
Diagnostic criteria CAFE SPOT:[2]
- Café-au-lait spots.
- Axillary or inguinal freckling.
- neuroFibroma (two or more) or plexiform neurofibroma (one).
- Eye hamartomas (Lisch nodules).
- Skeletal abnormalities, e.g. sphenoid dysplasia, leg bowing.
- Positive family history. †
- Optic Tumour (optic nerve glioma).
Note:
- † One could include paraganglioma here.
Other associations
Possible association
Images
Neurofibromatosis type 2
- Caused by mutations in the NF2 gene;[7] this gene is also known as merlin.[8]
- Reduced life expectancy.
- Mean age at diagnosis: 35years.
Diagnosis
Features (need 1/3 to diagnose):[9]
- Bilateral CNVIII masses on imaging.
- Unilateral CNVIII mass + first-degree relative with NF2.
- First-degree relative with NF2 and 2/4 of the following:
- Meningioma (meningothelial meningioma) up to 50% of the cases.[10]
- Glioma, mostly spinal ependymomas (up tp 20% of NF2 cases affected).
- Schwannoma.
- Juvenile cataract.
Mnemonic MISME:[11]
- Multiple Inherited Schwannomas.
- Meningiomas.
- Ependymomas.
Other:
- Cerebral microhamartomas.
- Schwannosis (Schwann cell proliferations).
- Peripheral neuropathy.
Meningioangiomatosis
- Cortical proliferations of meningeothelial cells around small vessels.
- May occur within NF2 and sporadic.
- Associated with seizures and/or headaches.
- Often asymptomatic.
See also
Schwannomatosis
- Autosomal dominant.
- Prevalence: 1:155000 (UK).
- Distinct entity from NF2, mainly due to absence of vestibular schwannomas.
- Mean age at diagnosis: 40years.
- Life expectancy better compared to NF2.
Diagnosis
Features:[12]
- Two or more non-intradermal schwannomas.
- Radiological exclusion of vestibular schwannoma.
- NF2-mutation excluded.
- One schwannoma or meningioma and one relative with confirmed schwannomatosis.
- Germline SMARCB1 or LZTR1 variant and histologically confirmed schwannoma or meningioma.
IHC
- INI1 mosaic pattern in schwannomas.[13]
References
- ↑ URL: http://emedicine.medscape.com/article/1177266-overview. Accessed on: 3 May 2010.
- ↑ URL: http://www.paeds.co.uk/wiki/index.php?title=Mnemonics#Neurofibromatosis_Type_1_diagnostic_criteria. Accessed on: 30 May 2011.
- ↑ Alexakis, N.; Connor, S.; Ghaneh, P.; Lombard, M.; Smart, HL.; Evans, J.; Hughes, M.; Garvey, CJ. et al. (2004). "Hereditary pancreatic endocrine tumours.". Pancreatology 4 (5): 417-33; discussion 434-5. doi:10.1159/000079616. PMID 15249710.
- ↑ Agaimy A, Hartmann A (October 2010). "[Hereditary and non-hereditary syndromic gastointestinal stromal tumours]" (in German). Pathologe 31 (6): 430–7. doi:10.1007/s00292-010-1354-6. PMID 20848108.
- ↑ Harrison B, Sammer D (September 2014). "Glomus tumors and neurofibromatosis: a newly recognized association". Plast Reconstr Surg Glob Open 2 (9): e214. doi:10.1097/GOX.0000000000000144. PMC 4229273. PMID 25426397. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229273/.
- ↑ Castoldi, L.; De Rai, P.; Marini, A.; Ferrero, S.; De Luca, V.; Tiberio, G. (2001). "Neurofibromatosis-1 and Ampullary Gangliocytic Paraganglioma Causing Biliary and Pancreatic Obstruction.". Int J Gastrointest Cancer 29 (2): 93-98. PMID 12754392.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 101000
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 607379
- ↑ URL: http://emedicine.medscape.com/article/1178283-overview. Accessed on: 3 May 2010.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm. Accessed on: 26 October 2010.
- ↑ URL: http://emedicine.medscape.com/article/342667-overview. Accessed on: 20 February 2012.
- ↑ Evans, DG.; Bowers, NL.; Tobi, S.; Hartley, C.; Wallace, AJ.; King, AT.; Lloyd, SKW.; Rutherford, SA. et al. (Jun 2018). "Schwannomatosis: a genetic and epidemiological study.". J Neurol Neurosurg Psychiatry. doi:10.1136/jnnp-2018-318538. PMID 29909380.
- ↑ Caltabiano, R.; Magro, G.; Polizzi, A.; Praticò, AD.; Ortensi, A.; D'Orazi, V.; Panunzi, A.; Milone, P. et al. (Jun 2017). "A mosaic pattern of INI1/SMARCB1 protein expression distinguishes Schwannomatosis and NF2-associated peripheral schwannomas from solitary peripheral schwannomas and NF2-associated vestibular schwannomas.". Childs Nerv Syst 33 (6): 933-940. doi:10.1007/s00381-017-3340-2. PMID 28365909.