Difference between revisions of "Glioma"
Jensflorian (talk | contribs) (moved from neuropathology tumors) |
Jensflorian (talk | contribs) (removed frequency because data is from pre-molecular era and does not reflect current changes.) |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
==Classification== | ==Classification== | ||
Gliomas are classified by cell type, by WHO grade, and by location. | Gliomas are classified by cell type, by CNS WHO grade, patient age and by location. | ||
===By type of cell=== | ===By type of cell=== | ||
Gliomas are named according to the specific type of cell with which they share histological features, but not necessarily from which they originate. The main types of gliomas are: | Gliomas are named according to the specific type of cell with which they share histological features, but not necessarily from which they originate. The main types of gliomas are: | ||
* [[ | * [[Glioblastoma]] is a malignant astrocytoma and the most common primary brain tumor among adults. | ||
* [[ | * [[Astrocytoma]]s—[[astrocyte]]s. | ||
* [[ | * [[Oligodendroglioma]]s—[[oligodendrocyte]]s. | ||
* | * [[Ependymoma]]s—ependymal cells. | ||
* | * Glioneuronal and neuronal tumors. | ||
Note: | Note: | ||
Some authors consider [[choroid plexus]] as a specific type of glia, but [[choroid plexus tumors]] are usually not covered under the umberella term '''glioma'''. | Some authors consider [[choroid plexus]] as a specific type of glia, but [[choroid plexus tumors]] are usually not covered under the umberella term '''glioma'''. | ||
===By WHO grade=== | ===By CNS WHO grade=== | ||
Gliomas are further categorized according to their grade, which is determined by [[pathology|pathologic]] evaluation of the tumor. | Gliomas are further categorized according to their grade, which is determined by [[pathology|pathologic]] evaluation of the tumor. Of numerous grading systems in use, the most common is the [[World Health Organization]] (WHO) grading system under which tumors are graded from 1 (least advanced disease—best prognosis) to 4 (most advanced disease—worst prognosis). Historically roman numerals were used for grading, but have been replaced by arabic numerals for grading within tumor types. Specific molecular features may influence tumor grading which is now a combination of histology and molecular neuroathology. Grading is based on expected biological behaviour, although proper treatment may heavily change prognosis. | ||
*Low-grade gliomas [WHO grade | *Low-grade gliomas [CNS WHO grade 1-2] are well-differentiated (not anaplastic); these tend to exhibit [[cancer|benign]] tendencies and portend a better prognosis for the patient. However, they have a uniform rate of recurrence and some diffuse gliomas may increase in grade over time and therefore calling these tumours benign is avoided. | ||
*High-grade [WHO grade | *High-grade [CNS WHO grade 3-4] gliomas are undifferentiated or anaplastic; these are [[cancer|malignant]] and carry a worse prognosis. | ||
===By patient age group=== | |||
The fifth CNS WHO edition recognizes following categories: | |||
* Adult-type diffuse gliomas. | |||
* Pediatric-type diffuse low-grade gliomas. | |||
* Pediatric-type diffuse high-grade gliomas. | |||
* Circumscribed astrocytic gliomas. | |||
===By location=== | ===By location=== | ||
* A supratentorial tumour is above the tentorium, in the cerebrum, and mostly found in adults (70%). | |||
* An infratentorial tumour is below the tentorium, in the cerebellum, and mostly found in children (70%). | |||
* The pontine is located in the pons of the brainstem. The brainstem has three parts (pons, midbrain, and medulla); the pons controls critical functions such as breathing, making surgery on these extremely dangerous. | |||
* | * Anatomic separation is essential in ependymal tumors. They are classfied into three groups: | ||
* | ** Supratentorial ependymoma. | ||
* | ** Posterior fossa ependymoma. | ||
** Spinal ependymoma. | |||
* Some gliomas have a specific anatomic designation in their name, reflecting their predominant tumor location. | |||
** [[Diffuse hemispheric glioma, H3 G34-mutant]]. | |||
** [[Diffuse midline glioma, H3 K27-altered]]. | |||
** Infant-type hemispheric glioma. | |||
===By Molecular profile=== | |||
Some tumors can only diagnosed after a specific alteration has been confirmed. | |||
Examples are: | |||
* Astrocytoma, IDH-mutant. | |||
* Oligodendroglioma, IDH-mutant and 1p/19q codeleted. | |||
* [[Diffuse hemispheric glioma, H3 G34-mutant]]. | |||
* [[Diffuse midline glioma, H3 K27-altered]]. | |||
* [[Diffuse astrocytoma, MYB- or MYBL-altered]]. | |||
* CNS tumour with BCOR internal tandem duplication. | |||
==Table of common gliomas== | ==Table of common gliomas== | ||
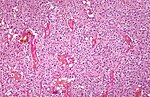
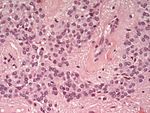
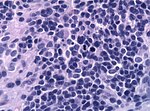
Histomorphologic comparison of common gliomas: | Histomorphologic comparison of common gliomas: | ||
{| class="wikitable" | {| class="wikitable" | ||
|'''Entity''' || '''Rosenthal <br>fibres / EGBs''' ||'''Nuclear atypia''' ||'''Mitoses''' || '''Necrosis | |'''Entity''' || '''Rosenthal <br>fibres / EGBs''' ||'''Nuclear atypia''' ||'''Mitoses''' || '''Necrosis''' ||'''MVP''' || '''Infiltrative''' || '''Image''' | ||
|- | |||
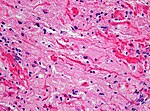
|[[Pilocytic astrocytoma]] || yes || usu. no || usu. no || usu. no || yes || no || [[Image:Rosenthal_HE_40x.jpg|thumb|150px]] | |||
|- | |- | ||
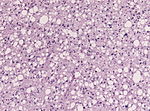
|[[ | |[[Astrocytoma CNS WHO grade 2]] || no || yes || no || no || no || yes || [[File:Astrocytoma_whoII_HE.jpg|thumb|150px]] | ||
|- | |- | ||
|[[ | |[[Astrocytoma CNS WHO grade 3]] || no || yes || yes || no || no || yes || [[Image:Anaplastic_astrocytoma_-_high_mag.jpg|thumb|150px]] | ||
|- | |- | ||
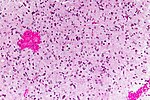
|[[ | |[[Glioblastoma]] || no || yes || yes || yes || yes || yes || [[Image:Glioblastoma_-_high_mag.jpg|thumb|150px]] | ||
|- | |- | ||
|[[ | |[[Oligodendroglioma]] || no || usu. no || yes || no || no || yes || [[Image:Oligodendroglioma1_low_mag.jpg|thumb|150px]] | ||
|- | |- | ||
|[[ | |[[Ependymoma CNS WHO grade 2]] || no || usu. no || usu. no || usu. no || no || discrete || [[Image:Ependymoma_H%26E.jpg|thumb|150px]] | ||
|- | |- | ||
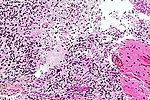
|[[Ependymoma]] || no || | |[[Ependymoma CNS WHO grade 3]] || no || yes || yes || usu. yes || rare || discrete || [[Image:HE anaplastic epedymomas mitoses pleomorphism.jpg|thumb|150px]] | ||
|} | |} | ||
Notes: | Notes: | ||
*''MVP'' = microvascular proliferation. | *''MVP'' = microvascular proliferation. | ||
*''EGBs'' = eosinophilic granular bodies. | *''EGBs'' = eosinophilic granular bodies. | ||
==See also== | ==See also== | ||
Latest revision as of 08:33, 4 April 2022

Gliomas are the most compon primary tumor in the brain and spinal cord. They originate from glial cells and their precursors.
Classification
Gliomas are classified by cell type, by CNS WHO grade, patient age and by location.
By type of cell
Gliomas are named according to the specific type of cell with which they share histological features, but not necessarily from which they originate. The main types of gliomas are:
- Glioblastoma is a malignant astrocytoma and the most common primary brain tumor among adults.
- Astrocytomas—astrocytes.
- Oligodendrogliomas—oligodendrocytes.
- Ependymomas—ependymal cells.
- Glioneuronal and neuronal tumors.
Note: Some authors consider choroid plexus as a specific type of glia, but choroid plexus tumors are usually not covered under the umberella term glioma.
By CNS WHO grade
Gliomas are further categorized according to their grade, which is determined by pathologic evaluation of the tumor. Of numerous grading systems in use, the most common is the World Health Organization (WHO) grading system under which tumors are graded from 1 (least advanced disease—best prognosis) to 4 (most advanced disease—worst prognosis). Historically roman numerals were used for grading, but have been replaced by arabic numerals for grading within tumor types. Specific molecular features may influence tumor grading which is now a combination of histology and molecular neuroathology. Grading is based on expected biological behaviour, although proper treatment may heavily change prognosis.
- Low-grade gliomas [CNS WHO grade 1-2] are well-differentiated (not anaplastic); these tend to exhibit benign tendencies and portend a better prognosis for the patient. However, they have a uniform rate of recurrence and some diffuse gliomas may increase in grade over time and therefore calling these tumours benign is avoided.
- High-grade [CNS WHO grade 3-4] gliomas are undifferentiated or anaplastic; these are malignant and carry a worse prognosis.
By patient age group
The fifth CNS WHO edition recognizes following categories:
- Adult-type diffuse gliomas.
- Pediatric-type diffuse low-grade gliomas.
- Pediatric-type diffuse high-grade gliomas.
- Circumscribed astrocytic gliomas.
By location
- A supratentorial tumour is above the tentorium, in the cerebrum, and mostly found in adults (70%).
- An infratentorial tumour is below the tentorium, in the cerebellum, and mostly found in children (70%).
- The pontine is located in the pons of the brainstem. The brainstem has three parts (pons, midbrain, and medulla); the pons controls critical functions such as breathing, making surgery on these extremely dangerous.
- Anatomic separation is essential in ependymal tumors. They are classfied into three groups:
- Supratentorial ependymoma.
- Posterior fossa ependymoma.
- Spinal ependymoma.
- Some gliomas have a specific anatomic designation in their name, reflecting their predominant tumor location.
- Diffuse hemispheric glioma, H3 G34-mutant.
- Diffuse midline glioma, H3 K27-altered.
- Infant-type hemispheric glioma.
By Molecular profile
Some tumors can only diagnosed after a specific alteration has been confirmed.
Examples are:
- Astrocytoma, IDH-mutant.
- Oligodendroglioma, IDH-mutant and 1p/19q codeleted.
- Diffuse hemispheric glioma, H3 G34-mutant.
- Diffuse midline glioma, H3 K27-altered.
- Diffuse astrocytoma, MYB- or MYBL-altered.
- CNS tumour with BCOR internal tandem duplication.
Table of common gliomas
Histomorphologic comparison of common gliomas:
| Entity | Rosenthal fibres / EGBs |
Nuclear atypia | Mitoses | Necrosis | MVP | Infiltrative | Image |
| Pilocytic astrocytoma | yes | usu. no | usu. no | usu. no | yes | no | |
| Astrocytoma CNS WHO grade 2 | no | yes | no | no | no | yes | |
| Astrocytoma CNS WHO grade 3 | no | yes | yes | no | no | yes | |
| Glioblastoma | no | yes | yes | yes | yes | yes | |
| Oligodendroglioma | no | usu. no | yes | no | no | yes | |
| Ependymoma CNS WHO grade 2 | no | usu. no | usu. no | usu. no | no | discrete | |
| Ependymoma CNS WHO grade 3 | no | yes | yes | usu. yes | rare | discrete |
Notes:
- MVP = microvascular proliferation.
- EGBs = eosinophilic granular bodies.