Difference between revisions of "Atrophy of the prostate gland"
Jump to navigation
Jump to search
| (4 intermediate revisions by the same user not shown) | |||
| Line 9: | Line 9: | ||
| LMDDx = [[prostate carcinoma]] - esp. [[atrophic prostate carcinoma]], [[atypical small acinar proliferation]] | | LMDDx = [[prostate carcinoma]] - esp. [[atrophic prostate carcinoma]], [[atypical small acinar proliferation]] | ||
| Stains = | | Stains = | ||
| IHC = AMACR -ve, p63 +ve (basal cells), CK34betaE12 +ve (basal cells) | | IHC = [[AMACR]] -ve, [[p63]] +ve (basal cells), [[CK34betaE12]] +ve (basal cells) | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| Line 31: | Line 31: | ||
}} | }} | ||
'''Atrophy of the prostate gland''', also '''prostatic atrophy''', is a common change in the [[prostate gland]]. | '''Atrophy of the prostate gland''', also '''prostatic atrophy''', is a common change in the [[prostate gland]]. | ||
==General== | ==General== | ||
*Considered to be the most common mimicker of [[prostate carcinoma]].<ref name=pmid18408595>{{Cite journal | last1 = Wang | first1 = W. | last2 = Sun | first2 = X. | last3 = Epstein | first3 = JI. | title = Partial atrophy on prostate needle biopsy cores: a morphologic and immunohistochemical study. | journal = Am J Surg Pathol | volume = 32 | issue = 6 | pages = 851-7 | month = Jun | year = 2008 | doi = 10.1097/PAS.0b013e31815a0508 | PMID = 18408595 }}</ref> | *Considered to be the most common mimicker of [[prostate carcinoma]].<ref name=pmid18408595>{{Cite journal | last1 = Wang | first1 = W. | last2 = Sun | first2 = X. | last3 = Epstein | first3 = JI. | title = Partial atrophy on prostate needle biopsy cores: a morphologic and immunohistochemical study. | journal = Am J Surg Pathol | volume = 32 | issue = 6 | pages = 851-7 | month = Jun | year = 2008 | doi = 10.1097/PAS.0b013e31815a0508 | PMID = 18408595 }}</ref> | ||
*Small glands | *Small glands - may mimic [[Gleason score|Gleason pattern]] 3. | ||
*Inflammatory atrophy seems to be related to [[HGPIN]] and [[prostate cancer]];<ref name=pmid10595928>{{Cite journal | last1 = De Marzo | first1 = AM. | last2 = Marchi | first2 = VL. | last3 = Epstein | first3 = JI. | last4 = Nelson | first4 = WG. | title = Proliferative inflammatory atrophy of the prostate: implications for prostatic carcinogenesis. | journal = Am J Pathol | volume = 155 | issue = 6 | pages = 1985-92 | month = Dec | year = 1999 | doi = 10.1016/S0002-9440(10)65517-4 | PMID = 10595928 }}</ref> however, the epidemiology is not compelling that this is a significant (clinical) association.<ref name=pmid24129226>{{Cite journal | last1 = Celma | first1 = A. | last2 = Servián | first2 = P. | last3 = Planas | first3 = J. | last4 = Placer | first4 = J. | last5 = Quilez | first5 = MT. | last6 = Arbós | first6 = MA. | last7 = de Torres | first7 = I. | last8 = Morote | first8 = J. | title = Clinical Significance of Proliferative Inflammatory Atrophy in Prostate Biopsy. | journal = Actas Urol Esp | volume = 38 | issue = 2 | pages = 122-126 | month = Mar | year = 2014 | doi = 10.1016/j.acuro.2013.04.008 | PMID = 24129226 }}</ref> | *Inflammatory atrophy seems to be related to [[HGPIN]] and [[prostate cancer]];<ref name=pmid10595928>{{Cite journal | last1 = De Marzo | first1 = AM. | last2 = Marchi | first2 = VL. | last3 = Epstein | first3 = JI. | last4 = Nelson | first4 = WG. | title = Proliferative inflammatory atrophy of the prostate: implications for prostatic carcinogenesis. | journal = Am J Pathol | volume = 155 | issue = 6 | pages = 1985-92 | month = Dec | year = 1999 | doi = 10.1016/S0002-9440(10)65517-4 | PMID = 10595928 }}</ref> however, the epidemiology is not compelling that this is a significant (clinical) association.<ref name=pmid24129226>{{Cite journal | last1 = Celma | first1 = A. | last2 = Servián | first2 = P. | last3 = Planas | first3 = J. | last4 = Placer | first4 = J. | last5 = Quilez | first5 = MT. | last6 = Arbós | first6 = MA. | last7 = de Torres | first7 = I. | last8 = Morote | first8 = J. | title = Clinical Significance of Proliferative Inflammatory Atrophy in Prostate Biopsy. | journal = Actas Urol Esp | volume = 38 | issue = 2 | pages = 122-126 | month = Mar | year = 2014 | doi = 10.1016/j.acuro.2013.04.008 | PMID = 24129226 }}</ref> | ||
===Classification=== | |||
It can be classified into:<ref name=pmid20815946>{{Cite journal | last1 = Billis | first1 = A. | title = Prostatic atrophy. Clinicopathological significance. | journal = Int Braz J Urol | volume = 36 | issue = 4 | pages = 401-9 | month = | year = | doi = | PMID = 20815946 }}</ref> | |||
#Focal prostatic atrophy. | |||
#Diffuse prostatic atrophy. | |||
Focal atrophy can be subclassified as:<ref name=pmid20815946/> | |||
#Partial. | |||
#Complete. | |||
#Combined. | |||
==Microscopic== | ==Microscopic== | ||
| Line 103: | Line 111: | ||
*[http://webpathology.com/image.asp?case=16&n=5 Partial atrophy (webpathology.com)]. | *[http://webpathology.com/image.asp?case=16&n=5 Partial atrophy (webpathology.com)]. | ||
*[http://webpathology.com/image.asp?case=16&n=6 Sclerotic atrophy (webpathology.com)]. | *[http://webpathology.com/image.asp?case=16&n=6 Sclerotic atrophy (webpathology.com)]. | ||
==IHC== | |||
*Classically like normal prostate (AMACR -ve, p63 +ve, CK34betaE12 +ve). | |||
**May be negative for basal cell markers, i.e. p63 and CK34betaE12.<ref name=pmid18408595>{{cite journal |author=Wang W, Sun X, Epstein JI |title=Partial atrophy on prostate needle biopsy cores: a morphologic and immunohistochemical study |journal=Am. J. Surg. Pathol. |volume=32 |issue=6 |pages=851–7 |year=2008 |month=June |pmid=18408595 |doi=10.1097/PAS.0b013e31815a0508 |url=}}</ref> | |||
==Sign out== | ==Sign out== | ||
Generally, this finding is ''not'' reported; it is considered a normal finding. | Generally, this finding is ''not'' reported; it is considered a normal finding. | ||
<pre> | |||
Left Apex: | |||
- Benign prostate tissue with glandular atrophy. | |||
</pre> | |||
===Micro=== | |||
The core shows rare, spaced, atrophic appearing glands, mostly with a wavy border and a decreased quantity of cytoplasm. Prominent nucleoli and significant nuclear enlargement are not identified. | |||
There are none of the following: mitoses, adjacent PIN, suspicious luminal material, nuclear hyperchromasia. | |||
==See also== | ==See also== | ||
Latest revision as of 14:50, 4 August 2022
| Atrophy of the prostate gland | |
|---|---|
| Diagnosis in short | |
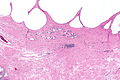
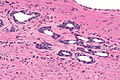
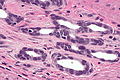
 Atrophic prostatic glands. H&E stain. | |
|
| |
| LM | glands typically have a jagged edges/prows (in cancer the glands tend to have round edges), gland density is usually lower than in prostate carcinoma (glands are not back-to-back), nuclei small & hyperchromatic, scant cytoplasm |
| LM DDx | prostate carcinoma - esp. atrophic prostate carcinoma, atypical small acinar proliferation |
| IHC | AMACR -ve, p63 +ve (basal cells), CK34betaE12 +ve (basal cells) |
| Site | prostate gland |
|
| |
| Symptoms | none |
| Prevalence | very common |
| Prognosis | benign |
| Treatment | none |
Atrophy of the prostate gland, also prostatic atrophy, is a common change in the prostate gland.
General
- Considered to be the most common mimicker of prostate carcinoma.[1]
- Small glands - may mimic Gleason pattern 3.
- Inflammatory atrophy seems to be related to HGPIN and prostate cancer;[2] however, the epidemiology is not compelling that this is a significant (clinical) association.[3]
Classification
It can be classified into:[4]
- Focal prostatic atrophy.
- Diffuse prostatic atrophy.
Focal atrophy can be subclassified as:[4]
- Partial.
- Complete.
- Combined.
Microscopic
Features:
- Glands often have a jagged edges/prows (in cancer the glands tend to have round edges) - key feature.
- Prow = forward most part of a ship's bow that cuts through the water.[5]
- You may have come across prow in the context of breast cancer, i.e. tubular carcinoma.
- Prow = forward most part of a ship's bow that cuts through the water.[5]
- Gland density is usually lower than in prostate carcinoma, i.e. glands are not back-to-back - key feature.
- Atrophic glands are often hyperchromatic.[6]
- Scant cytoplasm - usually.
Negatives:
- Nuclei like normal, i.e. nucleoli uncommon.
- Should have two cell layers, i.e. epithelial and myoepithelial (may be difficult to see).
Notes:
- Atrophic glands may be scattered with non-atrophic ones.
- IHC may be misleading - basal cell loss.
DDx:
- Atrophic prostate carcinoma.
- Atypical small acinar proliferation.
- Prostate carcinoma - focal, low grade.
Atrophy versus cancer
| Histologic feature | Atrophy | Cancer |
|---|---|---|
| Glandular architecture/ arrangement |
angulated glands, may look like they originate from one large duct |
round glands, often back-to-back |
| Nuclear hyperchromasia |
marked | moderate |
| Cytoplasm | scant/minimal | moderate, may be amphophilic |
| Basal cells | may be visible | absent |
| Nucleoli | absent | present |
| Secretions in glands |
no | yes - eosinophilic or blue |
Images
www:
- Atrophy (webpathology.com).
- Partial atrophy (webpathology.com).
- Sclerotic atrophy (webpathology.com).
IHC
- Classically like normal prostate (AMACR -ve, p63 +ve, CK34betaE12 +ve).
- May be negative for basal cell markers, i.e. p63 and CK34betaE12.[1]
Sign out
Generally, this finding is not reported; it is considered a normal finding.
Left Apex: - Benign prostate tissue with glandular atrophy.
Micro
The core shows rare, spaced, atrophic appearing glands, mostly with a wavy border and a decreased quantity of cytoplasm. Prominent nucleoli and significant nuclear enlargement are not identified.
There are none of the following: mitoses, adjacent PIN, suspicious luminal material, nuclear hyperchromasia.
See also
References
- ↑ 1.0 1.1 Wang, W.; Sun, X.; Epstein, JI. (Jun 2008). "Partial atrophy on prostate needle biopsy cores: a morphologic and immunohistochemical study.". Am J Surg Pathol 32 (6): 851-7. doi:10.1097/PAS.0b013e31815a0508. PMID 18408595. Cite error: Invalid
<ref>tag; name "pmid18408595" defined multiple times with different content - ↑ De Marzo, AM.; Marchi, VL.; Epstein, JI.; Nelson, WG. (Dec 1999). "Proliferative inflammatory atrophy of the prostate: implications for prostatic carcinogenesis.". Am J Pathol 155 (6): 1985-92. doi:10.1016/S0002-9440(10)65517-4. PMID 10595928.
- ↑ Celma, A.; Servián, P.; Planas, J.; Placer, J.; Quilez, MT.; Arbós, MA.; de Torres, I.; Morote, J. (Mar 2014). "Clinical Significance of Proliferative Inflammatory Atrophy in Prostate Biopsy.". Actas Urol Esp 38 (2): 122-126. doi:10.1016/j.acuro.2013.04.008. PMID 24129226.
- ↑ 4.0 4.1 Billis, A.. "Prostatic atrophy. Clinicopathological significance.". Int Braz J Urol 36 (4): 401-9. PMID 20815946.
- ↑ http://en.wikipedia.org/wiki/Prow
- ↑ SN. June 3, 2009.