Difference between revisions of "Acute cholecystitis"
Jump to navigation
Jump to search
| (7 intermediate revisions by the same user not shown) | |||
| Line 6: | Line 6: | ||
| Micro = edema, hemorrhage, +/-neutrophils, +/-reactive epithelial changes | | Micro = edema, hemorrhage, +/-neutrophils, +/-reactive epithelial changes | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[chronic cholecystitis]], [[intestinal metaplasia of the gallbladder]], [[gallbladder dysplasia]], [[adenocarcinoma of the gallbladder]] | | LMDDx = [[chronic cholecystitis]], [[intestinal metaplasia of the gallbladder]], [[gallbladder dysplasia]], [[adenocarcinoma of the gallbladder]]. [[eosinophilic cholecystitis]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = | ||
| Line 13: | Line 13: | ||
| IF = | | IF = | ||
| Gross = wall thickening (due to edema), gallstone(s) in the neck (classic finding), +/-mucosal erosions | | Gross = wall thickening (due to edema), gallstone(s) in the neck (classic finding), +/-mucosal erosions | ||
| Grossing = | | Grossing = [[gallbladder grossing]] | ||
| Site = [[gallbladder]] | | Site = [[gallbladder]] | ||
| Assdx = [[cholelithiasis]] | | Assdx = [[cholelithiasis]] | ||
| Line 34: | Line 34: | ||
*Less common than ''chronic cholecystitis''. | *Less common than ''chronic cholecystitis''. | ||
*Usually due to gallstones.<ref name=Ref_Sternberg5_1606>{{Ref Sternberg5|1606}}</ref> | *Usually due to gallstones.<ref name=Ref_Sternberg5_1606>{{Ref Sternberg5|1606}}</ref> | ||
*Classically older individuals (50s and 60s) with a slight female predominance.<ref name=Ref_Sternberg5_1606>{{Sternberg5|1606}}</ref> | *Classically older individuals (50s and 60s) with a slight female predominance.<ref name=Ref_Sternberg5_1606>{{Ref Sternberg5|1606}}</ref> | ||
Notes: | Notes: | ||
| Line 66: | Line 66: | ||
*[[Gallbladder adenocarcinoma]]. | *[[Gallbladder adenocarcinoma]]. | ||
*[[Intestinal metaplasia of the gallbladder]]. | *[[Intestinal metaplasia of the gallbladder]]. | ||
*[[Eosinophilic cholecystitis]] - has >90% eosinophils. | |||
===Images=== | ===Images=== | ||
| Line 100: | Line 101: | ||
====Necrosis of wall==== | ====Necrosis of wall==== | ||
<pre> | |||
Gallbladder, Cholecystectomy: | |||
- Acute cholecystitis with multiple mucosal erosions and focal necrosis of the gallbladder wall. | |||
</pre> | |||
<pre> | <pre> | ||
GALLBLADDER, CHOLECYSTECTOMY: | GALLBLADDER, CHOLECYSTECTOMY: | ||
| Line 111: | Line 117: | ||
- GANGRENOUS CHOLECYSTITIS. | - GANGRENOUS CHOLECYSTITIS. | ||
- CHOLELITHIASIS. | - CHOLELITHIASIS. | ||
</pre> | |||
<pre> | |||
Gallbladder, Cholecystectomy: | |||
- Gangrenous (acute) cholecystitis with cholelithiasis. | |||
</pre> | </pre> | ||
Latest revision as of 14:43, 15 August 2024
| Acute cholecystitis | |
|---|---|
| Diagnosis in short | |
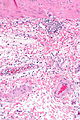
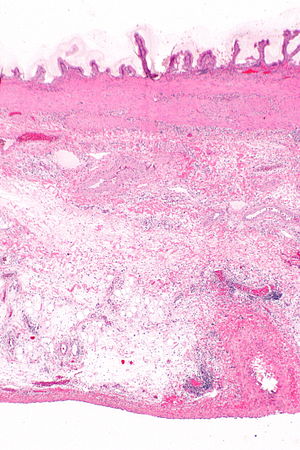 Acute cholecystitis. H&E stain. | |
|
| |
| LM | edema, hemorrhage, +/-neutrophils, +/-reactive epithelial changes |
| LM DDx | chronic cholecystitis, intestinal metaplasia of the gallbladder, gallbladder dysplasia, adenocarcinoma of the gallbladder. eosinophilic cholecystitis |
| Gross | wall thickening (due to edema), gallstone(s) in the neck (classic finding), +/-mucosal erosions |
| Grossing notes | gallbladder grossing |
| Site | gallbladder |
|
| |
| Associated Dx | cholelithiasis |
| Clinical history | elderly individuals (50s and 60s) |
| Signs | Murphy's sign present |
| Prevalence | uncommon |
| Radiology | wall thickening (>3 mm), gallstone(s) in the neck |
| Prognosis | benign, good |
| Treatment | cholecystectomy |
Acute cholecystitis, abbreviated AC, is a relatively uncommon gallbladder pathology when compared to chronic cholecystitis. It is usually associated with gallstones and seen in older individuals.
General
- Less common than chronic cholecystitis.
- Usually due to gallstones.[1]
- Classically older individuals (50s and 60s) with a slight female predominance.[1]
Notes:
- Pathologic diagnosis very often discordant with clinical impression.[2]
Gross
Features:[1]
- Wall thickening - due to edema and hemorrhage.†
- Gallstone(s) - classically obstructing the gallbladder neck.
- +/-Mucosal erosions.
Note:
Microscopic
Features:[1]
- Edema.
- Hemorrhage.
- +/-Fibrin thrombi in small veins.
- +/-Mucosal erosions.
- +/-Neutrophils - useful
- +/-Reactive epithelial changes.[6]
Notes:
- May see activated fibroblasts.
DDx:
- Chronic cholecystitis - has less inflammation, fibrotic wall thickening/muscular hypertrophy, may have RK sinuses.
- Gallbladder adenocarcinoma.
- Intestinal metaplasia of the gallbladder.
- Eosinophilic cholecystitis - has >90% eosinophils.
Images
Special types
Gangrenous cholecystitis
General:[7]
- Older.
- Clinically "sicker".
- Worse outcome than (acute) non-gangrenous cholecystitis.
Microscopic:
Sign out
Gallbladder, Cholecystectomy: - Acute cholecystitis with cholelithiasis.
Block letters
GALLBLADDER, CHOLECYSTECTOMY: - ACUTE CHOLECYSTITIS. - CHOLELITHIASIS.
Necrosis of wall
Gallbladder, Cholecystectomy: - Acute cholecystitis with multiple mucosal erosions and focal necrosis of the gallbladder wall.
GALLBLADDER, CHOLECYSTECTOMY: - ACUTE AND CHRONIC CHOLECYSTITIS WITH MULTIPLE MUCOSAL EROSIONS AND FOCAL NECROSIS OF THE GALLBLADDER WALL.
Gangrenous cholecystitis
GALLBLADDER, CHOLECYSTECTOMY: - GANGRENOUS CHOLECYSTITIS. - CHOLELITHIASIS.
Gallbladder, Cholecystectomy: - Gangrenous (acute) cholecystitis with cholelithiasis.
Xanthomatous lymph node present
GALLBLADDER, CHOLECYSTECTOMY: - ACUTE CHOLECYSTITIS. - CHOLELITHIASIS. - BENIGN LYMPH NODE WITH NONNECROTIZING GRANULOMAS, XANTHOMATOUS APPEARANCE. - NEGATIVE FOR DYSPLASIA.
Micro
The sections show gallbladder wall with hemorrhage, and activated fibroblasts. The superficial mucosa has clusters of neutrophils.
Alternate
The sections show an inflamed gallbladder wall with hemorrhage, activated fibroblasts and focal necrosis. The mucosa is partially eroded. Abundant neutrophils and eosinophils are present. No significant nuclear changes are apparent.
See also
References
- ↑ 1.0 1.1 1.2 1.3 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 1606. ISBN 978-0781779425.
- ↑ Fitzgibbons, RJ.; Tseng, A.; Wang, H.; Ryberg, A.; Nguyen, N.; Sims, KL. (Dec 1996). "Acute cholecystitis. Does the clinical diagnosis correlate with the pathological diagnosis?". Surg Endosc 10 (12): 1180-4. PMID 8939838.
- ↑ Tsung, JW.; Raio, CC.; Ramirez-Schrempp, D.; Blaivas, M. (Mar 2010). "Point-of-care ultrasound diagnosis of pediatric cholecystitis in the ED.". Am J Emerg Med 28 (3): 338-42. doi:10.1016/j.ajem.2008.12.003. PMID 20223393.
- ↑ Kim, HJ.; Park, JH.; Park, DI.; Cho, YK.; Sohn, CI.; Jeon, WK.; Kim, BI.; Choi, SH. (Feb 2012). "Clinical usefulness of endoscopic ultrasonography in the differential diagnosis of gallbladder wall thickening.". Dig Dis Sci 57 (2): 508-15. doi:10.1007/s10620-011-1870-0. PMID 21879282.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 174. ISBN 978-0470519035.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 439. ISBN 978-0443066573.
- ↑ Nikfarjam, M.; Niumsawatt, V.; Sethu, A.; Fink, MA.; Muralidharan, V.; Starkey, G.; Jones, RM.; Christophi, C. (Aug 2011). "Outcomes of contemporary management of gangrenous and non-gangrenous acute cholecystitis.". HPB (Oxford) 13 (8): 551-8. doi:10.1111/j.1477-2574.2011.00327.x. PMID 21762298.
- ↑ Struetker C. 25 February 2009.