Difference between revisions of "CSF cytopathology"
Jump to navigation
Jump to search
(move, adjustments) |
|||
| (28 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
This article deal only with cerebrospinal fluid (CSF) cytopathology. An introduction to cytopathology is in the ''[[cytopathology]]'' article. | This article deal only with cerebrospinal fluid (CSF) cytopathology. An introduction to cytopathology is in the ''[[cytopathology]]'' article. | ||
In many institutions, CSF specimens get triaged/rapidly assessed as: | |||
#They are small specimens ~ usually 1-10 ml. | #They are small specimens ~ usually 1-10 ml. | ||
#The procedure to obtain them is non-trivial, i.e. not pleasant for the patient and not risk free. | #The procedure to obtain them is non-trivial, i.e. not pleasant for the patient and not risk free. | ||
#Lymphoma is a common malignancy of malignancies found in the CSF. | #Lymphoma is a common malignancy of malignancies found in the CSF. | ||
In many institutions, all CSF specimens are ''stat''. ''Lumbar puncture'' redirects here. | |||
==Cerebrospinal fluid== | ==Cerebrospinal fluid== | ||
==Normal== | ==Normal== | ||
*Paucicellular. | *Paucicellular. | ||
**Acellular specimens common and considered adequate.<ref>{{cite book |author=Mody, Dina R. |title= [https://www.amazon.ca/Diagnostic-Pathology-Cytopathology-Dina-Mody/dp/1931884552/ Diagnostic Cytopathology] |publisher=Elsevier Canada |location= |year=2018 |pages= {{{1|II-3 2}}} |edition=1st |isbn=978-1931884556 |oclc= |doi= |accessdate=}}</ref> | |||
*protein is around 15-40 mg/dl. | |||
Gobs of anuclear material: | Gobs of anuclear material: | ||
*Protein vs. white | *Protein vs. white matter. | ||
*Ocassionally arachnoid cap cell- | |||
Bark-like flaky material: | Bark-like flaky material: | ||
| Line 26: | Line 28: | ||
*Cytospin - if no abnormality at triage. | *Cytospin - if no abnormality at triage. | ||
**The cellularity of the cytospin will appear to be increased (artifact). | **The cellularity of the cytospin will appear to be increased (artifact). | ||
===Images=== | |||
<gallery> | |||
File:4 vials of human cerebrospinal fluid.jpg | Normal CSF fluid is clear. (WC/James Heilman) | |||
File:CSF normal cytology.jpg | Normal CSF cytology Pappenheim specimen. (WC/jensflorian) | |||
</gallery> | |||
==Hemorrhage== | |||
*Xanthochromatous specimen | |||
**Can be artificial -> due punctuation injuries or rifampin medication.<ref name="pmid7125611">{{Cite journal | last1 = Liggett | first1 = SB. | last2 = Berger | first2 = JR. | last3 = Hush | first3 = J. | title = Cerebrospinal fluid xanthochromia with rifampin. | journal = Ann Neurol | volume = 12 | issue = 2 | pages = 228-9 | month = Aug | year = 1982 | doi = 10.1002/ana.410120240 | PMID = 7125611 }}</ref> | |||
**Can be seen in newborn -> due to increased bilirubin levels. | |||
**Best seen when looking from top through the tube. <ref name="pmid3981778">{{Cite journal | last1 = Bremer | first1 = HL. | title = Identification of xanthochromia. | journal = JAMA | volume = 253 | issue = 17 | pages = 2496 | month = May | year = 1985 | doi = | PMID = 3981778 }}</ref> | |||
**pink (free hemoglobin directly after bleeding) to yellow (bilirubin after one day). | |||
===Cytology=== | |||
*Mostly RBC. | |||
*Neutrophils can be increased. | |||
*+/-Erythro- and Siderophages (usu. after 3-4d). | |||
<gallery> | |||
File:XanthochromeCSF.jpg | Xanthochromatous CSF (WC/Dschafar) | |||
File:Siderophage_CSF_cytology.jpg | A siderophage (WC/jensflorian) | |||
</gallery> | |||
==Acute bacterial meningitis== | ==Acute bacterial meningitis== | ||
*Neutrophils.<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref> | {{Main|Meningitis}} | ||
===Cytology=== | |||
*Neutrophils - none should be present normally.<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref><ref>MUN. 4 November 2010.</ref> | |||
**If the tap is traumatic (i.e. fibrin is present) the finding may be uninterpretable. | |||
**Neutrophils may be present in early exsudative phase of viral meningitis. | |||
*Cell count usually above 1000/µl. | |||
<gallery> | |||
File:CSF_pleocytosis_neutrophils.jpg | CSF (Pappenheim stain) with numerous neutrophils indicating a purulent meningitis (WC/jensflorian) | |||
File:CSF S capitis 2013-11-08.JPG | Streoptococcal meningitis in a neonate with ventriculoperitoneal shunt (WC/Paulo Henrique Orlandi Mourao) | |||
File:Gram Stain Anthrax.jpg | Gram-positive Anthrax bacteria in a CSF specimen (WC/TenOfAllTrades). | |||
</gallery> | |||
DDx: | |||
*[[TBC]] | |||
*Fungal meningitis | |||
==Viral meningitis== | ==Viral meningitis== | ||
{{Main|Meningitis}} | |||
===General=== | |||
*Positive viral culture. | |||
**HSV | |||
**CMV | |||
**Enterovirus | |||
**HIV | |||
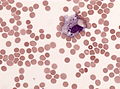
===Cytology=== | |||
*Pleocytosis (usu. 10-1000 cells/µl). | |||
*Polymorphous population of lymphocytes.<ref name=Ref_APBR681/> | *Polymorphous population of lymphocytes.<ref name=Ref_APBR681/> | ||
* Activated lymphocytes. | |||
* Plasma cells (sometimes bi- and multinuclear). | |||
* Occ. mitoses. | |||
* Activated (vacuolated) monocytes. | |||
<gallery> | |||
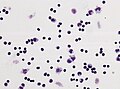
File:Hiv_meningeoencephalitis_csf_pleocytosis.jpg | Lymphocytic plecoytosis in HIV meningeoencephalitis | |||
File:HSV1_encephalitis_CSF_specimen.jpg | Activated lymphocytes in HSV1 encephalitis | |||
</gallery> | |||
==Mollaret's meningitis== | ==Mollaret's meningitis== | ||
General | ===General=== | ||
*Rare aseptic meningitis. | *Rare aseptic meningitis. | ||
*Suspected to be caused by HSV1 and HSV2.<ref name=emed1169489>[http://emedicine.medscape.com/article/1169489-overview http://emedicine.medscape.com/article/1169489-overview]</ref> | *Suspected to be caused by HSV1 and HSV2.<ref name=emed1169489>[http://emedicine.medscape.com/article/1169489-overview http://emedicine.medscape.com/article/1169489-overview]</ref> | ||
| Line 41: | Line 101: | ||
*Recurrent meningismus, headache, +/-fever.<ref name=emed1169489/> | *Recurrent meningismus, headache, +/-fever.<ref name=emed1169489/> | ||
===Cytology=== | |||
Features: | |||
*Mollaret cells - described as ''monocytoid cells''<ref name=Ref_APBR681/> (look like monocytes<ref>[http://www.mondofacto.com/facts/dictionary?monocytoid+cell http://www.mondofacto.com/facts/dictionary?monocytoid+cell]</ref> - but do not phagocytose), and ''large endothelial cells''.<ref name=emed1169489/> | *Mollaret cells - described as ''monocytoid cells''<ref name=Ref_APBR681/> (look like monocytes<ref>[http://www.mondofacto.com/facts/dictionary?monocytoid+cell http://www.mondofacto.com/facts/dictionary?monocytoid+cell]</ref> - but do not phagocytose), and ''large endothelial cells''.<ref name=emed1169489/> | ||
**Features - large cells with: abundant cytoplasm, footprint-shaped" nucleus. | **Features - large cells with: abundant cytoplasm, footprint-shaped" nucleus. | ||
| Line 50: | Line 111: | ||
*[http://www.cmaj.ca/cgi/content/full/174/12/1710-a Mollaret cells (cmaj.ca)]. | *[http://www.cmaj.ca/cgi/content/full/174/12/1710-a Mollaret cells (cmaj.ca)]. | ||
==CNS lymphoma== | ==Meningeosis neoplastica== | ||
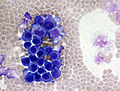
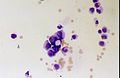
===CNS lymphoma=== | |||
Histology:<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref> | Histology:<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref> | ||
*Too many cells - ''key feature''. | *Too many cells - ''key feature''. | ||
| Line 61: | Line 123: | ||
Notes: | Notes: | ||
*Massive karyorrhexis (nuclear fragmentation) is suggestive of lymphoma<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref> - not common. | *Massive karyorrhexis (nuclear fragmentation) is suggestive of lymphoma<ref name=Ref_APBR681>{{Ref APBR|681 (Q25)}}</ref> - not common. | ||
<gallery> | |||
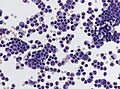
File:NHL b-cell meningiosis.jpg | CSF cytology of a diffuse large B-cell non hodgkin lymphoma. Atypical cells are larger and have a basophilic cytoplasm (WC/jensflorian). | |||
File:CSF Lymphoma on CSF cytospin cluster of blastoid cells 3.jpg | Blastoid cells in a CNS lympoma (WC/Prof. Erhabor Osaro) | |||
</gallery> | |||
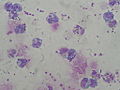
===Meningeal carcinomatosis (Meningeosis carcinomatosa)=== | |||
Histology: | |||
*abnormal cell size / giant multinuclear cells. | |||
*unusual nuclear/cytoplasm ratio. | |||
*hyperchromatic nuclei. | |||
*prominent nucleoli. | |||
*atypical mitoses. | |||
*cell clustering. | |||
Notes: | |||
*cell count can be normal. | |||
*accompanied by granulocytes and monocytes. | |||
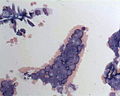
<gallery> | |||
File:Meningeosis carcinomatosa.jpg | Lung adenocarcinoma cells in CSF (WC/Marvin101). | |||
File:Leptomeningeal metastasis.jpg | Atypical mitosis in epithelial cells in CSF (WC/jensflorian). | |||
File:Meningiosis carcinomatosa.jpg | Leptomeningeal carinomatois (WC/jensflorian). | |||
</gallery> | |||
===Non-lymphoid, non-epithelial neoplasm=== | |||
*Non-lymphoid, non-epithelial neoplasms are rarely found in the CSF. | |||
*[[Ependymoma]]s and [[medulloblastoma]]s have a higher rate of dissemination than other primary brain tumors. | |||
Meningeosis gliomatosa ([[Astrocytoma]]/[[Glioblastoma]]): | |||
*May vaguely resemble a neuroendocrine tumour: | |||
**Small cell clusters. | |||
**Nuclear moulding. | |||
**Cells somewhat larger than small cell carcinoma. | |||
**Scant cytoplasm. | |||
<gallery> | |||
File:Bild 01Meningeosis gliomatosa 20x GFAP.jpg | GFAP IHC in a CSF specimen highlighting glioma cells (WC/Marvin101). | |||
</gallery> | |||
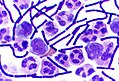
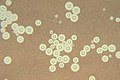
==CNS fungal infections== | ==CNS fungal infections== | ||
*Cryptococcus is the most common.<ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | *Cryptococcus is the most common.<ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
== | ==Cryptococcosis== | ||
* | {{Main|Cryptococcosis}} | ||
*[[AKA]] cryptococcus infection | |||
===General=== | |||
*Usu. immunocompromised host. | |||
===Microscopic=== | |||
Microscopic appearance: | Microscopic appearance: | ||
*Yeast:<ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | *Yeast:<ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| Line 73: | Line 178: | ||
**Thick mucopolysacchardie capsule + refractile centre. | **Thick mucopolysacchardie capsule + refractile centre. | ||
***"Target-like" shape/"bull's eye" appearance. | ***"Target-like" shape/"bull's eye" appearance. | ||
**"Tear drop-shapped" budding pattern (useful to differentiate from Blastomyces, Histoplasma). | **"Tear drop-shapped" budding pattern (useful to differentiate from Blastomyces, [[Histoplasma]]). | ||
Images: | Images: | ||
| Line 79: | Line 184: | ||
*[http://commons.wikimedia.org/wiki/File:Cryptococcosis_of_lung_in_patient_with_AIDS._Mucicarmine_stain_962_lores.jpg Crytococcosis - mucicarmine stain (WC)]. | *[http://commons.wikimedia.org/wiki/File:Cryptococcosis_of_lung_in_patient_with_AIDS._Mucicarmine_stain_962_lores.jpg Crytococcosis - mucicarmine stain (WC)]. | ||
*[http://commons.wikimedia.org/wiki/File:Cryptococcosis_of_lung_in_patient_with_AIDS_Methenamine_silver_stain_963_lores.jpg Crytococcosis - methenamine silver stain (WC)]. | *[http://commons.wikimedia.org/wiki/File:Cryptococcosis_of_lung_in_patient_with_AIDS_Methenamine_silver_stain_963_lores.jpg Crytococcosis - methenamine silver stain (WC)]. | ||
<gallery> | |||
File:Cryptococcus_neoformans_using_a_light_India_ink_staining_preparation_PHIL_3771_lores.jpg | Ink preparation of Cryptococcosis (CDC/Dr. Leanor Haley) | |||
</gallery> | |||
==See also== | ==See also== | ||
Latest revision as of 17:38, 26 June 2024
CSF cytopathology is a subset of CNS cytopathology, which is a subset of cytopathology.
This article deal only with cerebrospinal fluid (CSF) cytopathology. An introduction to cytopathology is in the cytopathology article.
In many institutions, CSF specimens get triaged/rapidly assessed as:
- They are small specimens ~ usually 1-10 ml.
- The procedure to obtain them is non-trivial, i.e. not pleasant for the patient and not risk free.
- Lymphoma is a common malignancy of malignancies found in the CSF.
In many institutions, all CSF specimens are stat. Lumbar puncture redirects here.
Cerebrospinal fluid
Normal
- Paucicellular.
- Acellular specimens common and considered adequate.[1]
- protein is around 15-40 mg/dl.
Gobs of anuclear material:
- Protein vs. white matter.
- Ocassionally arachnoid cap cell-
Bark-like flaky material:
- Contaminant.
Fluffy/smudged large cells (~2-3x RBC dia.) with an indistinct nucleus:
- Degenerated white cells.
- Should prompt a comment about "degeneration", if the population is dominant.
Routine processing
- Cytospin - if no abnormality at triage.
- The cellularity of the cytospin will appear to be increased (artifact).
Images
Hemorrhage
- Xanthochromatous specimen
Cytology
- Mostly RBC.
- Neutrophils can be increased.
- +/-Erythro- and Siderophages (usu. after 3-4d).
Acute bacterial meningitis
Main article: Meningitis
Cytology
- Neutrophils - none should be present normally.[4][5]
- If the tap is traumatic (i.e. fibrin is present) the finding may be uninterpretable.
- Neutrophils may be present in early exsudative phase of viral meningitis.
- Cell count usually above 1000/µl.
DDx:
- TBC
- Fungal meningitis
Viral meningitis
Main article: Meningitis
General
- Positive viral culture.
- HSV
- CMV
- Enterovirus
- HIV
Cytology
- Pleocytosis (usu. 10-1000 cells/µl).
- Polymorphous population of lymphocytes.[4]
- Activated lymphocytes.
- Plasma cells (sometimes bi- and multinuclear).
- Occ. mitoses.
- Activated (vacuolated) monocytes.
Mollaret's meningitis
General
- Rare aseptic meningitis.
- Suspected to be caused by HSV1 and HSV2.[6]
Clinical:
- Recurrent meningismus, headache, +/-fever.[6]
Cytology
Features:
- Mollaret cells - described as monocytoid cells[4] (look like monocytes[7] - but do not phagocytose), and large endothelial cells.[6]
- Features - large cells with: abundant cytoplasm, footprint-shaped" nucleus.
- Mollaret cells not pathognomonic.[6]
- Mixed population of inflammatory cells[4] (PMNs, monocytes, plasma cells, lymphocytes); usually lymphocyte predominant.[6]
Image:
Meningeosis neoplastica
CNS lymphoma
Histology:[4]
- Too many cells - key feature.
- Not diagnostic... but should raise suspicion.
- Single cells (as typical of lymphoma/leukemia).
- Large lymphocytes - >2x RBC diameter.
- +/-Nuclear atypia.
- Radial segmentation - a completely cleaved nucleus/quasi-binucleation.
Notes:
- Massive karyorrhexis (nuclear fragmentation) is suggestive of lymphoma[4] - not common.
Meningeal carcinomatosis (Meningeosis carcinomatosa)
Histology:
- abnormal cell size / giant multinuclear cells.
- unusual nuclear/cytoplasm ratio.
- hyperchromatic nuclei.
- prominent nucleoli.
- atypical mitoses.
- cell clustering.
Notes:
- cell count can be normal.
- accompanied by granulocytes and monocytes.
Non-lymphoid, non-epithelial neoplasm
- Non-lymphoid, non-epithelial neoplasms are rarely found in the CSF.
- Ependymomas and medulloblastomas have a higher rate of dissemination than other primary brain tumors.
Meningeosis gliomatosa (Astrocytoma/Glioblastoma):
- May vaguely resemble a neuroendocrine tumour:
- Small cell clusters.
- Nuclear moulding.
- Cells somewhat larger than small cell carcinoma.
- Scant cytoplasm.
CNS fungal infections
- Cryptococcus is the most common.[8]
Cryptococcosis
Main article: Cryptococcosis
- AKA cryptococcus infection
General
- Usu. immunocompromised host.
Microscopic
Microscopic appearance:
- Yeast:[8]
- Round/ovoid 5-15 micrometres.
- Thick mucopolysacchardie capsule + refractile centre.
- "Target-like" shape/"bull's eye" appearance.
- "Tear drop-shapped" budding pattern (useful to differentiate from Blastomyces, Histoplasma).
Images:
- Cryptococcus in lung FNA - Field stain (WC).
- Crytococcosis - mucicarmine stain (WC).
- Crytococcosis - methenamine silver stain (WC).
See also
References
- ↑ Mody, Dina R. (2018). Diagnostic Cytopathology (1st ed.). Elsevier Canada. pp. II-3 2. ISBN 978-1931884556.
- ↑ Liggett, SB.; Berger, JR.; Hush, J. (Aug 1982). "Cerebrospinal fluid xanthochromia with rifampin.". Ann Neurol 12 (2): 228-9. doi:10.1002/ana.410120240. PMID 7125611.
- ↑ Bremer, HL. (May 1985). "Identification of xanthochromia.". JAMA 253 (17): 2496. PMID 3981778.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q25). ISBN 978-1416025887.
- ↑ MUN. 4 November 2010.
- ↑ 6.0 6.1 6.2 6.3 6.4 http://emedicine.medscape.com/article/1169489-overview
- ↑ http://www.mondofacto.com/facts/dictionary?monocytoid+cell
- ↑ 8.0 8.1 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.