Difference between revisions of "Amyloid"
m (→Classification: w) |
m |
||
| (35 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Cardiac amyloidosis very high mag he.jpg | |||
| Width = | |||
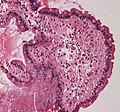
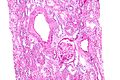
| Caption = Cardiac amyloidosis. [[H&E stain]]. | |||
| Micro = typically extracellular, amorphous (no specific shape), acellular and pink (on [[H&E stain]]) -- cotton candy like, classically has a "cracked" appearance | |||
| Subtypes = multiple subclassifications: ''Robbins'' (AL amyloidosis, AA amyloidosis, non-AA and non-AL), ''set of six subtypes'' (primary (AL amyloidosis), secondary (AA amyloidosis, hemodialysis-related, localized), hereditary, senile systemic amyloidosis) | |||
| LMDDx = fibrin, collagen, smooth muscle | |||
| Stains = [[Congo red]] +ve, [[Masson trichrome]] blue-gray staining | |||
| IHC = | |||
| EM = non-branching fine fibrils - usually 8-12 nm in diameter (accepted range 8-15 nm) | |||
| Molecular = beta sheet | |||
| IF = | |||
| Gross = waxy appearance | |||
| Grossing = | |||
| Site = pretty much anywhere, [[blood vessel]]s | |||
| Assdx = very many | |||
| Syndromes = | |||
| Clinicalhx = variable | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = dependent on subtype | |||
| Other = | |||
| ClinDDx = | |||
}} | |||
'''Amyloid''' is one of those things clinicians can put in many [[differential diagnoses]]. The [[pathologist]] can diagnose it. | '''Amyloid''' is one of those things clinicians can put in many [[differential diagnoses]]. The [[pathologist]] can diagnose it. | ||
This article is a general overview of the topic. Links are provided to articles that deal with amyloidosis at specific sites, see ''[[Amyloid#Site specific|site specific]]'' section below. | |||
=Overview= | =Overview= | ||
| Line 8: | Line 39: | ||
===Light microscopy=== | ===Light microscopy=== | ||
Features:<ref>{{Ref_PBoD|259}}</ref> | Features:<ref>{{Ref_PBoD|259}}</ref> | ||
*Pink (on H&E stain). | *Pink (on [[H&E stain]]). | ||
*Extracellular location. | *Extracellular location. | ||
*Amorphous - no specific shape. | *Amorphous - no specific shape. | ||
*May have a "cracked" appearance.{{fact}} | |||
Classic DDx - ''ABCs'' of pink: | |||
* | *Amyloid. | ||
*Blood (fibrin). | |||
*Collagen. | |||
*Smooth muscle. | |||
Other considerations: | |||
*Foreign material, e.g. lifting agent "O'rise".<ref name=pmid31934919>{{cite journal |authors=Pezhouh MK, Burgart LJ, Chiu K, Cohen DA, Hutchings DA, Sanderson SO, Shirazi M, Stanich PP, VandenBussche CJ, Voltaggio L, Willhoit ED, Xue Y, Arnold CA |title=Characterization of Novel Injectable Lifting Agents Used in Colonic Polyp Removal: An Emerging Amyloid Mimic |journal=Am J Surg Pathol |volume=44 |issue=6 |pages=793–798 |date=June 2020 |pmid=31934919 |doi=10.1097/PAS.0000000000001435 |url=}}</ref> | |||
Images | ====Images==== | ||
<gallery> | |||
Image:Small_bowel_duodenum_with_amyloid_deposition_20X.jpg | Amyloid - H&E stain. (WC) | |||
Image:Small bowel duodenum with amyloid deposition congo red 10X.jpg | Amyloid - congo red stain. (WC) | |||
</gallery> | |||
===Electron microscopy=== | ===Electron microscopy=== | ||
| Line 32: | Line 71: | ||
*[[CADASIL]] (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy). | *[[CADASIL]] (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy). | ||
**Typically has basophilic granularity in the blood vessels.<ref name=pmid17076524>{{cite journal |author=Kleinschmidt-DeMasters BK, Prayson RA |title=An algorithmic approach to the brain biopsy--part I |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=11 |pages=1630–8 |year=2006 |month=November |pmid=17076524 |doi= |url=}}</ref> | **Typically has basophilic granularity in the blood vessels.<ref name=pmid17076524>{{cite journal |author=Kleinschmidt-DeMasters BK, Prayson RA |title=An algorithmic approach to the brain biopsy--part I |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=11 |pages=1630–8 |year=2006 |month=November |pmid=17076524 |doi= |url=}}</ref> | ||
==Stains== | |||
*[[Congo red]] +ve. | |||
**Positive:<ref name=pmid18076735>{{cite journal |author=Ebert EC, Nagar M |title=Gastrointestinal manifestations of amyloidosis |journal=Am. J. Gastroenterol. |volume=103 |issue=3 |pages=776-87 |year=2008 |month=March |pmid=18076735 |doi=10.1111/j.1572-0241.2007.01669.x |url=}}</ref> | |||
***Orange/light red (non-polarized light). | |||
***Apple green birefringence ([[polarized light]]). | |||
**Negative: | |||
***Blue birefringence (polarized light) = collagen fibers.<ref name=pmid21760829/> | |||
*[[Thioflavin T stain]].<ref name=pmid18175051>{{cite journal |author=Nishi S, Alchi B, Imai N, Gejyo F |title=New advances in renal amyloidosis |journal=Clin. Exp. Nephrol. |volume=12 |issue=2 |pages=93-101 |year=2008 |month=April |pmid=18175051 |doi=10.1007/s10157-007-0008-3 |url=}}</ref> | |||
*Sodium sulphate-Alcian Blue stain +ve.<ref name=pmid55419>{{Cite journal | last1 = Pomerance | first1 = A. | last2 = Slavin | first2 = G. | last3 = McWatt | first3 = J. | title = Experience with the sodium sulphate-Alcian Blue stain for amyloid in cardiac pathology. | journal = J Clin Pathol | volume = 29 | issue = 1 | pages = 22-6 | month = Jan | year = 1976 | doi = | PMID = 55419 }}</ref> | |||
*[[Masson trichrome stain]]: blue-gray staining.<ref name=pmid33002919>{{cite journal |authors=Kunnath-Velayudhan S, Larsen BT, Coley SM, De Michele S, Santoriello D, Colby TV, Bhagat G, Saqi A |title=Masson Trichrome and Sulfated Alcian Blue Stains Distinguish Light Chain Deposition Disease From Amyloidosis in the Lung |journal=Am J Surg Pathol |volume=45 |issue=3 |pages=405–413 |date=March 2021 |pmid=33002919 |doi=10.1097/PAS.0000000000001593 |url=}}</ref> | |||
==Sign out== | ==Sign out== | ||
| Line 124: | Line 174: | ||
**Considered to be the definitive test.<ref name=pmid11447744/><ref name=pmid17046651>{{cite journal |author=Murphy CL, Wang S, Williams T, Weiss DT, Solomon A |title=Characterization of systemic amyloid deposits by mass spectrometry |journal=Meth. Enzymol. |volume=412 |issue= |pages=48–62 |year=2006 |pmid=17046651 |doi=10.1016/S0076-6879(06)12004-2 |url=}}</ref> | **Considered to be the definitive test.<ref name=pmid11447744/><ref name=pmid17046651>{{cite journal |author=Murphy CL, Wang S, Williams T, Weiss DT, Solomon A |title=Characterization of systemic amyloid deposits by mass spectrometry |journal=Meth. Enzymol. |volume=412 |issue= |pages=48–62 |year=2006 |pmid=17046651 |doi=10.1016/S0076-6879(06)12004-2 |url=}}</ref> | ||
***High specificity and sensitivity vis-à-vis clinicopathologic correlation.<ref name=pmid19797517>{{cite journal |author=Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR, Dogan A |title=Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens |journal=Blood |volume=114 |issue=24 |pages=4957–9 |year=2009 |month=December |pmid=19797517 |doi=10.1182/blood-2009-07-230722 |url=}}</ref> | ***High specificity and sensitivity vis-à-vis clinicopathologic correlation.<ref name=pmid19797517>{{cite journal |author=Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR, Dogan A |title=Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens |journal=Blood |volume=114 |issue=24 |pages=4957–9 |year=2009 |month=December |pmid=19797517 |doi=10.1182/blood-2009-07-230722 |url=}}</ref> | ||
**May be done on formalin-fixed paraffin embedded (FFPE) material.<ref name=pmid19797517/> | **May be done on [[formalin-fixed paraffin embedded]] (FFPE) material.<ref name=pmid19797517/> | ||
=Types= | =Types= | ||
| Line 139: | Line 189: | ||
===General=== | ===General=== | ||
*Previously known as ''senile cardiac amyloidosis''.<ref name=pmid15645642>{{Cite journal | last1 = Ikeda | first1 = S. | title = Cardiac amyloidosis: heterogenous pathogenic backgrounds. | journal = Intern Med | volume = 43 | issue = 12 | pages = 1107-14 | month = Dec | year = 2004 | doi = | PMID = 15645642 }}</ref> | *Previously known as ''senile cardiac amyloidosis''.<ref name=pmid15645642>{{Cite journal | last1 = Ikeda | first1 = S. | title = Cardiac amyloidosis: heterogenous pathogenic backgrounds. | journal = Intern Med | volume = 43 | issue = 12 | pages = 1107-14 | month = Dec | year = 2004 | doi = | PMID = 15645642 }}</ref> | ||
*May be referred to as ''ATTR'' = amyloidosis TTR; in SSA the TTR is not mutated. | *May be referred to as ''ATTR'' = amyloidosis TTR; in SSA the TTR is not mutated, some call it: wt transthyretin amyloidosis (ATTR). | ||
**There is a hereditary form of amyloidosis with mutated TTR deposition known as ''ATTR type FAP'' = ATTR type Familial Amyloid Polyneuropathy. | **There is a hereditary form of amyloidosis with mutated TTR deposition known as ''ATTR type FAP'' = ATTR type Familial Amyloid Polyneuropathy. | ||
***Hereditary TTR: deposits in the heart, nerves and leptomeningeal amyloidosis. | |||
Epidemiology: | Epidemiology: | ||
| Line 147: | Line 198: | ||
Treatment: | Treatment: | ||
* | *Liver transplantation, RNAi therapy (patisiran) and antisense oligonucleotides (inotersen).<ref>{{Cite journal | last1 = Adams | first1 = D. | last2 = Koike | first2 = H. | last3 = Slama | first3 = M. | last4 = Coelho | first4 = T. | title = Hereditary transthyretin amyloidosis: a model of medical progress for a fatal disease. | journal = Nat Rev Neurol | volume = 15 | issue = 7 | pages = 387-404 | month = Jul | year = 2019 | doi = 10.1038/s41582-019-0210-4 | PMID = 31209302 }}</ref> | ||
===Gross pathology=== | ===Gross pathology=== | ||
| Line 160: | Line 211: | ||
*Amyloid often present in the subepicardial tissue<ref name=pmid18329550/> - less commonly affected by ischemia. | *Amyloid often present in the subepicardial tissue<ref name=pmid18329550/> - less commonly affected by ischemia. | ||
Images | ====Images==== | ||
<gallery> | |||
Image:Cardiac_amyloidosis_very_high_mag_he.jpg | Senile systemic amyloidosis - H&E. (WC) | |||
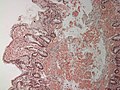
Image:Cardiac_amyloidosis_intermed_mag.jpg | Senile systemic amyloidosis - congo red. (WC) | |||
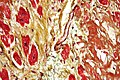
Image:Cardiac_amyloidosis_very_high_mag_movat.jpg | Senile systemic amyloidosis - Movat's. (WC) | |||
</gallery> | |||
=Site specific= | =Site specific= | ||
==Abdomen== | |||
:''Abdominal fat pad biopsy'' redirects here. | |||
===General=== | |||
*Abdominal fat pad biopsy - common screen for amyloidosis. | |||
**May be done with FNA. | |||
***Suffers for poor sensitivity.<ref name=pmid21760829>{{Cite journal | last1 = Devata | first1 = S. | last2 = Hari | first2 = P. | last3 = Markelova | first3 = N. | last4 = Li | first4 = R. | last5 = Komorowski | first5 = R. | last6 = Shidham | first6 = VB. | title = Detection of amyloid in abdominal fat pad aspirates in early amyloidosis: Role of electron microscopy and Congo red stained cell block sections. | journal = Cytojournal | volume = 8 | issue = | pages = 11 | month = | year = 2011 | doi = 10.4103/1742-6413.82278 | PMID = 21760829 }}</ref> | |||
===Microscopic=== | |||
Features: | |||
*Small-to-intermediate sized arteries with a thickened amorphous eosinophilic media. | |||
**Thickening classically nodular. | |||
**Apple green-birefringence -- with polarization. | |||
Note: | |||
*Evaluation of at least 15 small blood vessels is recommended.<ref name=pmid21760829/> | |||
===Sign out=== | |||
<pre> | |||
SOFT TISSUE, ABDOMEN, BIOPSY: | |||
- AMYLOIDOSIS. | |||
</pre> | |||
====Negative==== | |||
<pre> | |||
SOFT TISSUE, ABDOMEN, BIOPSY: | |||
- BENIGN FIBROADIPOSE TISSUE. | |||
- NEGATIVE FOR AMYLOIDOSIS WITH CONGO RED STAINING AND POLARIZED LIGHT. | |||
COMMENT: | |||
Correlation with serum protein electrophoresis, urine protein electrophoresis | |||
and bone marrow sampling should be considered within the clinical context. | |||
</pre> | |||
==Cardiac amyloidosis== | ==Cardiac amyloidosis== | ||
===General=== | ===General=== | ||
*Common cause of restrictive cardiomyopathy.<ref>Cardiac amyloidosis. Medlineplus.org. URL: [http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm]. Accessed on: 3 December 2009.</ref> | *Common cause of [[restrictive cardiomyopathy]].<ref>Cardiac amyloidosis. Medlineplus.org. URL: [http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm]. Accessed on: 3 December 2009.</ref> | ||
Cardiac amyloidosis - subtypes: | Cardiac amyloidosis - subtypes: | ||
#AL amyloidosis - associated with plasma cell dyscrasia - most common cardiac amyloidosis.<ref name=pmid18329550>{{Cite journal | last1 = Sharma | first1 = PP. | last2 = Payvar | first2 = S. | last3 = Litovsky | first3 = SH. | title = Histomorphometric analysis of intramyocardial vessels in primary and senile amyloidosis: epicardium versus endocardium. | journal = Cardiovasc Pathol | volume = 17 | issue = 2 | pages = 65-71 | month = | year = | doi = 10.1016/j.carpath.2007.05.008 | PMID = 18329550 }}</ref> | #AL amyloidosis - associated with plasma cell dyscrasia - most common cardiac amyloidosis.<ref name=pmid18329550>{{Cite journal | last1 = Sharma | first1 = PP. | last2 = Payvar | first2 = S. | last3 = Litovsky | first3 = SH. | title = Histomorphometric analysis of intramyocardial vessels in primary and senile amyloidosis: epicardium versus endocardium. | journal = Cardiovasc Pathol | volume = 17 | issue = 2 | pages = 65-71 | month = | year = | doi = 10.1016/j.carpath.2007.05.008 | PMID = 18329550 }}</ref> | ||
#Senile systemic amyloidosis - TTR-related amyloidosis (unmutated TTR). | #[[Senile systemic amyloidosis]] - TTR-related amyloidosis (unmutated TTR). | ||
#Hereditary amyloidosis. | #Hereditary amyloidosis. | ||
#AA amyloidosis is uncommon. | #[[AA amyloidosis]] is uncommon. | ||
Clinical: | Clinical: | ||
| Line 205: | Line 291: | ||
*[[Immunotactoid glomerulopathy]]. | *[[Immunotactoid glomerulopathy]]. | ||
Images | ====Images==== | ||
<gallery> | |||
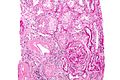
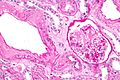
Image:Renal_amyloidosis_-_high_mag.jpg | Renal amyloidosis - high mag. (WC) | |||
Image:Renal_amyloidosis_-_2_-_high_mag.jpg | Renal amyloidosis - high mag. (WC) | |||
Image:Renal_amyloidosis_-_2_-_very_high_mag.jpg | Renal amyloidosis - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://path.upmc.edu/cases/case125.html Renal amyloidosis - several images (upmc.edu)]. | |||
==Urinary bladder amyloidosis== | |||
{{Main|Urinary bladder amyloidosis}} | |||
==GI amyloidosis== | ==GI amyloidosis== | ||
| Line 221: | Line 311: | ||
*Parenchymal deposition (common). | *Parenchymal deposition (common). | ||
*Portal triad deposition (less common). | *Portal triad deposition (less common). | ||
===Gastric amyloidosis=== | |||
{{Main|Amyloidosis of the stomach}} | |||
==Bone== | ==Bone== | ||
Latest revision as of 15:53, 1 May 2024
| Amyloid | |
|---|---|
| Diagnosis in short | |
 Cardiac amyloidosis. H&E stain. | |
|
| |
| LM | typically extracellular, amorphous (no specific shape), acellular and pink (on H&E stain) -- cotton candy like, classically has a "cracked" appearance |
| Subtypes | multiple subclassifications: Robbins (AL amyloidosis, AA amyloidosis, non-AA and non-AL), set of six subtypes (primary (AL amyloidosis), secondary (AA amyloidosis, hemodialysis-related, localized), hereditary, senile systemic amyloidosis) |
| LM DDx | fibrin, collagen, smooth muscle |
| Stains | Congo red +ve, Masson trichrome blue-gray staining |
| EM | non-branching fine fibrils - usually 8-12 nm in diameter (accepted range 8-15 nm) |
| Molecular | beta sheet |
| Gross | waxy appearance |
| Site | pretty much anywhere, blood vessels |
|
| |
| Associated Dx | very many |
| Clinical history | variable |
| Prevalence | uncommon |
| Prognosis | dependent on subtype |
Amyloid is one of those things clinicians can put in many differential diagnoses. The pathologist can diagnose it.
This article is a general overview of the topic. Links are provided to articles that deal with amyloidosis at specific sites, see site specific section below.
Overview
Definition
- Disorder of protein folding - structure: beta sheet.[1]
Appearance
Light microscopy
Features:[2]
- Pink (on H&E stain).
- Extracellular location.
- Amorphous - no specific shape.
- May have a "cracked" appearance.[citation needed]
Classic DDx - ABCs of pink:
- Amyloid.
- Blood (fibrin).
- Collagen.
- Smooth muscle.
Other considerations:
- Foreign material, e.g. lifting agent "O'rise".[3]
Images
Electron microscopy
Features:[4]
- Fine fibrils, non-branching.
- Usually 8-12 nm in diameter; accepted range 8-15 nm.[5]
Images:
DDx
- CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy).
- Typically has basophilic granularity in the blood vessels.[6]
Stains
- Congo red +ve.
- Positive:[7]
- Orange/light red (non-polarized light).
- Apple green birefringence (polarized light).
- Negative:
- Blue birefringence (polarized light) = collagen fibers.[8]
- Positive:[7]
- Thioflavin T stain.[9]
- Sodium sulphate-Alcian Blue stain +ve.[10]
- Masson trichrome stain: blue-gray staining.[11]
Sign out
BONE LESION, RIGHT ILIAC, BIOPSY: - AMYLOID ASSOCIATED WITH HISTOCYTES, GIANT CELLS AND A FEW LYMPHOCYTES AND PLASMA CELLS. COMMENT: The presence of amyloid is confirmed with congo red staining and polarization. There are no histomorphologic findings suggestive of a plasma cell neoplasm in this biopsy. Clinical correlation with serum protein electrophoresis, urine protein electrophoresis and bone marrow sampling is suggested.
Associations - DDx
- Infections:[12][13]
- Tuberculosis.
- Leprosy.
- Chronic osteomyelitis.
- Bronchiectasis.
- Idiopathic conditions:
- Rheumatoid arthritis - relatively common (compared to others below).
- Anklyosing spondylitis - renal amyloidosis.
- Crohn's disease.[12]
- Familial Mediterranean fever.[12]
- Malignancy.
- Plasmacytoma.
- 5-15% of patients with multiple myeloma develop amyloidosis[14] - some say 10-20%.[12]
- Medullary thyroid carcinoma.
- Renal cell carcinoma.
- Plasmacytoma.
- Many other conditions...
Classification
Amyloidosis can be classified a number of different ways.
Six subtypes classification
Amyloid classified into six groups:[7]
- Primary (AL amyloidosis).
- Monoclonal light chains in serum and/or urine, may be due to plasma cell dyscrasia.
- Secondary (AA amyloidosis).
- Infections (osteomyelitis), neoplasia (Hodgkin's lymphoma).
- Hemodialysis-related.
- Beta-2 microglobulin.[15]
- Localized.
- Abeta amyloid found in Alzheimer's disease.
- Pancreatic amyloid deposition associated with diabetes mellitus type 2.[16]
- Image: Amyloid in DM (med.utah.edu).[17]
- Hereditary.
- Senile systemic amyloidosis.
How to remember: Two As = secondary amyloidosis.
Three main types - Robbins classification
Amyloid classified into three groups:[1]
- AL amyloidosis - "AL" = Amyloid Light chain.[18]
- AA amyloidosis - "AA" = Amyloid Associated.[20]
- Secondary amyloidosis.
- Abeta amyloid - found in Alzheimer's disease.[21]
Additional types:
- ATTR = Amyloid Transthyretin (TTR)
- Transthyretin - serum protein that transport thyroxine and retinol; transthyretin AKA prealbumin.
Treatment
The very short version:
Classification of amyloid - differentiation
Biochemical techniques
- Pre-treated with potassium permanganate, to obliterate congo red reactivity, was though be definitive for AA amyloidosis;[22] this is now generally considered to be unreliable.[23]
Immunohistochemistry
Possibly useful immunostains:
- Kappa.
- Lambda.
- Transthyretin.
- The name transthyretin is from transports thyroxine and retinol (previous unknown as prealbumin).
Mass spectroscopy
- Can be typed using mass spectroscopy.[27]
- Considered to be the definitive test.[26][28]
- High specificity and sensitivity vis-à-vis clinicopathologic correlation.[29]
- May be done on formalin-fixed paraffin embedded (FFPE) material.[29]
- Considered to be the definitive test.[26][28]
Types
Secondary amyloidosis
- AKA AA amyloidosis.
- Pathophysiology: acute-phase reactant serum amyloid A (SAA) - degraded + deposits.[12][30]
Cerebral amyloid angiopathy
A common cause of lobar hemorrhage (cerebral cortex, cerebellar cortex) in the elderly.
Senile systemic amyloidosis
- Abbreviated SSA.
General
- Previously known as senile cardiac amyloidosis.[31]
- May be referred to as ATTR = amyloidosis TTR; in SSA the TTR is not mutated, some call it: wt transthyretin amyloidosis (ATTR).
- There is a hereditary form of amyloidosis with mutated TTR deposition known as ATTR type FAP = ATTR type Familial Amyloid Polyneuropathy.
- Hereditary TTR: deposits in the heart, nerves and leptomeningeal amyloidosis.
- There is a hereditary form of amyloidosis with mutated TTR deposition known as ATTR type FAP = ATTR type Familial Amyloid Polyneuropathy.
Epidemiology:
- Common in the elderly, as the word senile suggests.
- Found in approx. 25% of elderly over 80 years old,[31] and in upto 65% of patients over 90 years old.[32]
Treatment:
- Liver transplantation, RNAi therapy (patisiran) and antisense oligonucleotides (inotersen).[33]
Gross pathology
- Grey/black "peppering" of left atrial endocardium - in fixed specimens.[34]
- "Peppering" should be present if severe.
Microscopic
Features:
- Heart most commonly involved, followed by lungs and then by kidney (renal papilla).
- DDx of pink of H&E is important to remember: amyloid, muscle, collagen, clotted blood.
- Amyloid vs. Fibrosis? Subendocardial fibrosis may have rim of (diffusion) preserved myocytes. (???)
- Amyloid often present in the subepicardial tissue[32] - less commonly affected by ischemia.
Images
Site specific
Abdomen
- Abdominal fat pad biopsy redirects here.
General
- Abdominal fat pad biopsy - common screen for amyloidosis.
- May be done with FNA.
- Suffers for poor sensitivity.[8]
- May be done with FNA.
Microscopic
Features:
- Small-to-intermediate sized arteries with a thickened amorphous eosinophilic media.
- Thickening classically nodular.
- Apple green-birefringence -- with polarization.
Note:
- Evaluation of at least 15 small blood vessels is recommended.[8]
Sign out
SOFT TISSUE, ABDOMEN, BIOPSY: - AMYLOIDOSIS.
Negative
SOFT TISSUE, ABDOMEN, BIOPSY: - BENIGN FIBROADIPOSE TISSUE. - NEGATIVE FOR AMYLOIDOSIS WITH CONGO RED STAINING AND POLARIZED LIGHT. COMMENT: Correlation with serum protein electrophoresis, urine protein electrophoresis and bone marrow sampling should be considered within the clinical context.
Cardiac amyloidosis
General
- Common cause of restrictive cardiomyopathy.[35]
Cardiac amyloidosis - subtypes:
- AL amyloidosis - associated with plasma cell dyscrasia - most common cardiac amyloidosis.[32]
- Senile systemic amyloidosis - TTR-related amyloidosis (unmutated TTR).
- Hereditary amyloidosis.
- AA amyloidosis is uncommon.
Clinical:
- CHF, conduction abnormalities.
- Kidney disease (proteinuria) - associated with AL amyloidosis.
Pulmonary amyloidosis
- Very rare.
Renal amyloidosis
General
- Both AL and AA amyloidosis can affect the kidney.[9]
Clinical:
Microscopic
Features:
- Paucicellular mesangial expansion.
- Fluffy hyaline material in medium-sized blood vessels.
DDx:
- Diabetic nephropathy.
- Idiopathic nodular glomerulosclerosis.
- Light chain deposition disease.
- Fibrillary glomerulopathy.
- Immunotactoid glomerulopathy.
Images
www:
Urinary bladder amyloidosis
GI amyloidosis
- GI amyloidosis can lead to obstruction and usually is greatest in the small bowel.[7]
Liver amyloidosis
Features:
- Parenchymal deposition (common).
- Portal triad deposition (less common).
Gastric amyloidosis
Bone
Amyloid is reported in association with:
- Multiple myeloma ~40% of patients in one series.[37]
- Chronic osteomyelitis ~10% of patients in one series.[38]
- Diabetes (one case).[39]
See also
References
- ↑ 1.0 1.1 Lachmann HJ, Hawkins PN (2006). "Amyloidosis and the lung". Chron Respir Dis 3 (4): 203-14. PMID 17190124. http://crd.sagepub.com/cgi/pmidlookup?view=long&pmid=17190124.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ Pezhouh MK, Burgart LJ, Chiu K, Cohen DA, Hutchings DA, Sanderson SO, Shirazi M, Stanich PP, VandenBussche CJ, Voltaggio L, Willhoit ED, Xue Y, Arnold CA (June 2020). "Characterization of Novel Injectable Lifting Agents Used in Colonic Polyp Removal: An Emerging Amyloid Mimic". Am J Surg Pathol 44 (6): 793–798. doi:10.1097/PAS.0000000000001435. PMID 31934919.
- ↑ 4.0 4.1 URL: http://www.fondazionedamico.org/biopsiarenale_atlas/seco/amil/amil21.htm. Accessed on: 9 November 2010.
- ↑ Alpers, CE.; Kowalewska, J. (Jan 2008). "Fibrillary glomerulonephritis and immunotactoid glomerulopathy.". J Am Soc Nephrol 19 (1): 34-7. doi:10.1681/ASN.2007070757. PMID 18045849.
- ↑ Kleinschmidt-DeMasters BK, Prayson RA (November 2006). "An algorithmic approach to the brain biopsy--part I". Arch. Pathol. Lab. Med. 130 (11): 1630–8. PMID 17076524.
- ↑ 7.0 7.1 7.2 7.3 7.4 Ebert EC, Nagar M (March 2008). "Gastrointestinal manifestations of amyloidosis". Am. J. Gastroenterol. 103 (3): 776-87. doi:10.1111/j.1572-0241.2007.01669.x. PMID 18076735.
- ↑ 8.0 8.1 8.2 Devata, S.; Hari, P.; Markelova, N.; Li, R.; Komorowski, R.; Shidham, VB. (2011). "Detection of amyloid in abdominal fat pad aspirates in early amyloidosis: Role of electron microscopy and Congo red stained cell block sections.". Cytojournal 8: 11. doi:10.4103/1742-6413.82278. PMID 21760829.
- ↑ 9.0 9.1 Nishi S, Alchi B, Imai N, Gejyo F (April 2008). "New advances in renal amyloidosis". Clin. Exp. Nephrol. 12 (2): 93-101. doi:10.1007/s10157-007-0008-3. PMID 18175051.
- ↑ Pomerance, A.; Slavin, G.; McWatt, J. (Jan 1976). "Experience with the sodium sulphate-Alcian Blue stain for amyloid in cardiac pathology.". J Clin Pathol 29 (1): 22-6. PMID 55419.
- ↑ Kunnath-Velayudhan S, Larsen BT, Coley SM, De Michele S, Santoriello D, Colby TV, Bhagat G, Saqi A (March 2021). "Masson Trichrome and Sulfated Alcian Blue Stains Distinguish Light Chain Deposition Disease From Amyloidosis in the Lung". Am J Surg Pathol 45 (3): 405–413. doi:10.1097/PAS.0000000000001593. PMID 33002919.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 Amyloidosis. Merck Manual. URL: http://www.merck.com/mmpe/sec12/ch160/ch160a.html. Accessed on: 3 December 2009.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 260. ISBN 0-7216-0187-1.
- ↑ URL: http://www.umm.edu/altmed/articles/amyloidosis-000007.htm. Accessed on: 23 October 2010.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/enfrm.html. Accessed on: 6 December 2010.
- ↑ Comenzo, RL.; Vosburgh, E.; Falk, RH.; Sanchorawala, V.; Reisinger, J.; Dubrey, S.; Dember, LM.; Berk, JL. et al. (May 1998). "Dose-intensive melphalan with blood stem-cell support for the treatment of AL (amyloid light-chain) amyloidosis: survival and responses in 25 patients.". Blood 91 (10): 3662-70. PMID 9573002.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ van Rijswijk MH, van Heusden CW (October 1979). "The potassium permanganate method. A reliable method for differentiating amyloid AA from other forms of amyloid in routine laboratory practice". Am. J. Pathol. 97 (1): 43–58. PMC 2042379. PMID 495695. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2042379/.
- ↑ Picken, MM. (Apr 2010). "Amyloidosis-where are we now and where are we heading?". Arch Pathol Lab Med 134 (4): 545-51. doi:10.1043/1543-2165-134.4.545. PMID 20367306.
- ↑ Röcken C (December 2009). "[Update on immunohistological classification of amyloidoses]" (in German). Pathologe 30 Suppl 2: 121–3. doi:10.1007/s00292-009-1183-7. PMID 19756621.
- ↑ Solomon, A.; Murphy, CL.; Westermark, P. (Jan 2008). "Unreliability of immunohistochemistry for typing amyloid deposits.". Arch Pathol Lab Med 132 (1): 14; author reply 14-5. doi:10.1043/1543-2165(2008)132[14b:IR]2.0.CO;2. PMID 18181665. http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282008%29132%5B14b%3AIR%5D2.0.CO%3B2.
- ↑ 26.0 26.1 Murphy CL, Eulitz M, Hrncic R, et al. (July 2001). "Chemical typing of amyloid protein contained in formalin-fixed paraffin-embedded biopsy specimens". Am. J. Clin. Pathol. 116 (1): 135–42. doi:10.1309/TWBM-8L4E-VK22-FRH5. PMID 11447744.
- ↑ Chee, CE.; Lacy, MQ.; Dogan, A.; Zeldenrust, SR.; Gertz, MA. (Jun 2010). "Pitfalls in the diagnosis of primary amyloidosis.". Clin Lymphoma Myeloma Leuk 10 (3): 177-80. doi:10.3816/CLML.2010.n.027. PMID 20511161.
- ↑ Murphy CL, Wang S, Williams T, Weiss DT, Solomon A (2006). "Characterization of systemic amyloid deposits by mass spectrometry". Meth. Enzymol. 412: 48–62. doi:10.1016/S0076-6879(06)12004-2. PMID 17046651.
- ↑ 29.0 29.1 Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR, Dogan A (December 2009). "Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens". Blood 114 (24): 4957–9. doi:10.1182/blood-2009-07-230722. PMID 19797517.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 260. ISBN 0-7216-0187-1.
- ↑ 31.0 31.1 Ikeda, S. (Dec 2004). "Cardiac amyloidosis: heterogenous pathogenic backgrounds.". Intern Med 43 (12): 1107-14. PMID 15645642.
- ↑ 32.0 32.1 32.2 Sharma, PP.; Payvar, S.; Litovsky, SH.. "Histomorphometric analysis of intramyocardial vessels in primary and senile amyloidosis: epicardium versus endocardium.". Cardiovasc Pathol 17 (2): 65-71. doi:10.1016/j.carpath.2007.05.008. PMID 18329550.
- ↑ Adams, D.; Koike, H.; Slama, M.; Coelho, T. (Jul 2019). "Hereditary transthyretin amyloidosis: a model of medical progress for a fatal disease.". Nat Rev Neurol 15 (7): 387-404. doi:10.1038/s41582-019-0210-4. PMID 31209302.
- ↑ Pomerance, A. (Sep 1965). "Senile cardiac amyloidosis.". Br Heart J 27 (5): 711-8. PMID 5829755. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC469777/pdf/brheartj00340-0085.pdf.
- ↑ Cardiac amyloidosis. Medlineplus.org. URL: http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm. Accessed on: 3 December 2009.
- ↑ Satoskar, AA.; Burdge, K.; Cowden, DJ.; Nadasdy, GM.; Hebert, LA.; Nadasdy, T. (Jun 2007). "Typing of amyloidosis in renal biopsies: diagnostic pitfalls.". Arch Pathol Lab Med 131 (6): 917-22. doi:10.1043/1543-2165(2007)131[917:TOAIRB]2.0.CO;2. PMID 17550319. http://www.archivesofpathology.org/doi/full/10.1043/1543-2165(2007)131%5B917:TOAIRB%5D2.0.CO;2.
- ↑ Petruzziello, F.; Zeppa, P.; Catalano, L.; Cozzolino, I.; Gargiulo, G.; Musto, P.; D'Auria, F.; Liso, V. et al. (May 2010). "Amyloid in bone marrow smears of patients affected by multiple myeloma.". Ann Hematol 89 (5): 469-74. doi:10.1007/s00277-009-0857-9. PMID 19894050.
- ↑ Alabi, ZO.; Ojo, OS.; Odesanmi, WO. (1991). "Secondary amyloidosis in chronic osteomyelitis.". Int Orthop 15 (1): 21-2. PMID 2071276.
- ↑ Miossec, P.; Lormeau, B.; Valensi, P.; Arthuis, F.; Amouroux, J.; Attali, JR. (Sep 1999). "Bone amyloidoma in a diabetic patient with morbid obesity.". Diabetes Metab 25 (3): 261-3. PMID 10499196.
External links
- Amyloidosis - wikipedia.org.