Difference between revisions of "Vermiform appendix"
Jump to navigation
Jump to search
| (34 intermediate revisions by 2 users not shown) | |||
| Line 41: | Line 41: | ||
VERMIFORM APPENDIX WITHIN NORMAL LIMITS. | VERMIFORM APPENDIX WITHIN NORMAL LIMITS. | ||
</pre> | </pre> | ||
Note: | |||
*This is for a normal appendix within a larger operation. The article ''[[negative appendectomy]]'' deals with a normal appearing appendix that was removed for presumed appendicitis. | |||
==Negative appendectomy== | ==Negative appendectomy== | ||
{{Main|Negative appendectomy}} | |||
An appendectomy done for presumed [[acute appendicitis]] that is pathologically within normal limits | |||
=Inflammatory pathologies= | =Inflammatory pathologies= | ||
==Acute appendicitis== | ==Acute appendicitis== | ||
{{Main|Acute appendicitis}} | |||
==Adenovirus appendicitis== | ==Adenovirus appendicitis== | ||
{{Main|Adenovirus appendicitis}} | |||
==Enterobius vermicularis== | ==Enterobius vermicularis== | ||
| Line 178: | Line 62: | ||
*May be found in the appendix. | *May be found in the appendix. | ||
*The incidence is higher in normal appendices than inflamed ones.<ref name=pmid1853157>{{Cite journal | last1 = Wiebe | first1 = BM. | title = Appendicitis and Enterobius vermicularis. | journal = Scand J Gastroenterol | volume = 26 | issue = 3 | pages = 336-8 | month = Mar | year = 1991 | doi = | PMID = 1853157 }}</ref><ref name=pmid7945067/> | *The incidence is higher in normal appendices than inflamed ones.<ref name=pmid1853157>{{Cite journal | last1 = Wiebe | first1 = BM. | title = Appendicitis and Enterobius vermicularis. | journal = Scand J Gastroenterol | volume = 26 | issue = 3 | pages = 336-8 | month = Mar | year = 1991 | doi = | PMID = 1853157 }}</ref><ref name=pmid7945067/> | ||
*Clinically mimics appendicitis.<ref>{{cite journal |author=Ariyarathenam AV, Nachimuthu S, Tang TY, Courtney ED, Harris SA, Harris AM |title=Enterobius vermicularis infestation of the appendix and management at the time of laparoscopic appendectomy: case series and literature review |journal=Int J Surg |volume=8 |issue=6 |pages=466–9 |year=2010 |pmid=20637320 |doi=10.1016/j.ijsu.2010.06.007 |url=}}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 183: | Line 68: | ||
*Usu. the appendiceal wall has no inflammation, i.e. there is no appendicitis.<ref name=pmid1853157/><ref name=pmid7945067>{{Cite journal | last1 = Dahlstrom | first1 = JE. | last2 = Macarthur | first2 = EB. | title = Enterobius vermicularis: a possible cause of symptoms resembling appendicitis. | journal = Aust N Z J Surg | volume = 64 | issue = 10 | pages = 692-4 | month = Oct | year = 1994 | doi = | PMID = 7945067 }}</ref> | *Usu. the appendiceal wall has no inflammation, i.e. there is no appendicitis.<ref name=pmid1853157/><ref name=pmid7945067>{{Cite journal | last1 = Dahlstrom | first1 = JE. | last2 = Macarthur | first2 = EB. | title = Enterobius vermicularis: a possible cause of symptoms resembling appendicitis. | journal = Aust N Z J Surg | volume = 64 | issue = 10 | pages = 692-4 | month = Oct | year = 1994 | doi = | PMID = 7945067 }}</ref> | ||
*''[[Enterobius vermicularis]]'' organisms. | *''[[Enterobius vermicularis]]'' organisms. | ||
====Image==== | |||
<gallery> | |||
Image:Enterobius_-_very_low_mag.jpg | Enterobius - very low mag. (WC/Nephron) | |||
Image:Enterobius_-_high_mag.jpg | Enterobius - high mag. (WC/Nephron) | |||
Image:Pinworms_in_the_Appendix_%281%29.jpg | Pinworm (WC/Uthman) | |||
</gallery> | |||
==Granulomatous appendicitis== | ==Granulomatous appendicitis== | ||
{{Main|Granulomatous appendicitis}} | |||
==Inflammatory bowel disease== | ==Inflammatory bowel disease== | ||
| Line 223: | Line 94: | ||
*Acute inflammation of the serosa. | *Acute inflammation of the serosa. | ||
**[[Neutrophil]]s in the serosa. | **[[Neutrophil]]s in the serosa. | ||
DDx: | |||
*[[Acute appendicitis]]. | |||
=Tumours of the appendix= | =Tumours of the appendix= | ||
| Line 229: | Line 103: | ||
==Mucinous tumours of the appendix== | ==Mucinous tumours of the appendix== | ||
{{Main|Mucinous tumours of the appendix}} | |||
This grouping includes ''mucinous cystadenoma'' and ''mucinous cystadenocarcinoma''. | |||
==Goblet cell adenocarcinoma== | |||
{{Main|Goblet cell adenocarcinoma}} | |||
*Previously known as ''goblet cell carcinoid''. | |||
==Goblet cell | |||
* | |||
==Neuroendocrine tumour of the appendix== | ==Neuroendocrine tumour of the appendix== | ||
*Previously known as ''appendiceal carcinoid''. | *Previously known as ''appendiceal carcinoid''. | ||
*[[AKA]] ''appendiceal neuroendocrine tumour'', abbreviated ''appendiceal NET''. | *[[AKA]] ''appendiceal neuroendocrine tumour'', abbreviated ''appendiceal NET''. | ||
{{Main|Neuroendocrine tumour of the appendix}} | |||
=See also= | =See also= | ||
| Line 432: | Line 123: | ||
[[Category:Gastrointestinal pathology]] | [[Category:Gastrointestinal pathology]] | ||
[[Category:Vermiform appendix]] | |||
Latest revision as of 15:11, 4 December 2023
The vermiform appendix, usually just appendix, is a little thingy that is attached to the cecum. Taking it out is the bread 'n butter of general surgery.
The appendix is a vestigial structure that is thought to have arisen from a larger cecum. Larger cecae are often seen in herbivores and thought to facilitate better digestion of plant matter.[1]
Normal
Normal vermiform appendix
General
- Seen in:
- Right hemicolectomies.
- Surgeries for ovarian mucinous tumours.
Gross
- Shiny serosal surface.
- No exudate.
- Normal diameter.
- 6.6 +/- 1.5 mm -- based on CT.[2]
Microscopic
Features:
- +/-Lymphoid hyperplasia - mucosa or submucosa.
- Normal colorectal-type mucosa.
- Fatty submucosa.
- Benign smooth muscle.
- Serosa.
Negatives:
- No neutrophils in the muscularis propria.
- No lesion in appendiceal tip.
- No serosal inflammation (periappendicitis).
- No organisms in the appendiceal lumen, e.g. Enterobius vermicularis.
DDx:
- Adenovirus appendicitis.
- Cryptosporidiosis.
- Mild colitis.
Sign out
VERMIFORM APPENDIX WITHIN NORMAL LIMITS.
Note:
- This is for a normal appendix within a larger operation. The article negative appendectomy deals with a normal appearing appendix that was removed for presumed appendicitis.
Negative appendectomy
Main article: Negative appendectomy
An appendectomy done for presumed acute appendicitis that is pathologically within normal limits
Inflammatory pathologies
Acute appendicitis
Main article: Acute appendicitis
Adenovirus appendicitis
Main article: Adenovirus appendicitis
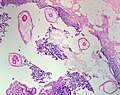
Enterobius vermicularis
Main article: Enterobius vermicularis
- AKA pinworm.
General
- May be found in the appendix.
- The incidence is higher in normal appendices than inflamed ones.[3][4]
- Clinically mimics appendicitis.[5]
Microscopic
Features:
- Usu. the appendiceal wall has no inflammation, i.e. there is no appendicitis.[3][4]
- Enterobius vermicularis organisms.
Image
Granulomatous appendicitis
Main article: Granulomatous appendicitis
Inflammatory bowel disease
Periappendicitis
General
Definition: inflammation of tissues around the (vermiform) appendix.[6]
- May be seen in association of appendicitis or alone.
Microscopic
Features:
- Acute inflammation of the serosa.
- Neutrophils in the serosa.
DDx:
Tumours of the appendix
Adenocarcinoma
- Like colorectal adenocarcinoma - see colorectal tumours.
Mucinous tumours of the appendix
Main article: Mucinous tumours of the appendix
This grouping includes mucinous cystadenoma and mucinous cystadenocarcinoma.
Goblet cell adenocarcinoma
Main article: Goblet cell adenocarcinoma
- Previously known as goblet cell carcinoid.
Neuroendocrine tumour of the appendix
- Previously known as appendiceal carcinoid.
- AKA appendiceal neuroendocrine tumour, abbreviated appendiceal NET.
Main article: Neuroendocrine tumour of the appendix
See also
References
- ↑ Dawkins, R. (2009). The Greatest Show on Earth: The Evidence for Evolution (1st ed.). Free Press. pp. 115. ISBN 978-1416594789.
- ↑ Charoensak, A.; Pongpornsup, S.; Suthikeeree, W. (Dec 2010). "Wall thickness and outer diameter of the normal appendix in adults using 64 slices multidetector CT.". J Med Assoc Thai 93 (12): 1437-42. PMID 21344807.
- ↑ 3.0 3.1 Wiebe, BM. (Mar 1991). "Appendicitis and Enterobius vermicularis.". Scand J Gastroenterol 26 (3): 336-8. PMID 1853157.
- ↑ 4.0 4.1 Dahlstrom, JE.; Macarthur, EB. (Oct 1994). "Enterobius vermicularis: a possible cause of symptoms resembling appendicitis.". Aust N Z J Surg 64 (10): 692-4. PMID 7945067.
- ↑ Ariyarathenam AV, Nachimuthu S, Tang TY, Courtney ED, Harris SA, Harris AM (2010). "Enterobius vermicularis infestation of the appendix and management at the time of laparoscopic appendectomy: case series and literature review". Int J Surg 8 (6): 466–9. doi:10.1016/j.ijsu.2010.06.007. PMID 20637320.
- ↑ URL: http://www.medilexicon.com/medicaldictionary.php?t=66889. Accessed on: 1 June 2011.
- ↑ Fink, AS.; Kosakowski, CA.; Hiatt, JR.; Cochran, AJ. (Jun 1990). "Periappendicitis is a significant clinical finding.". Am J Surg 159 (6): 564-8. PMID 2349982.
- ↑ O'Neil, MB.; Moore, DB. (Sep 1977). "Periappendicitis: Clinical reality or pathologic curiosity?". Am J Surg 134 (3): 356-7. PMID 900337.