Difference between revisions of "Seminal vesicles"
Jump to navigation
Jump to search
(tweak) |
(→Pathology: create link) |
||
| Line 55: | Line 55: | ||
==Amyloid in the seminal vesicles== | ==Amyloid in the seminal vesicles== | ||
{{Main|Amyloid in the seminal vesicles}} | {{Main|Amyloid in the seminal vesicles}} | ||
=Benign= | |||
==Stromal lipofuscinosis of the seminal vesicle== | |||
{{Main|Stromal lipofuscinosis of the seminal vesicle}} | |||
=See also= | =See also= | ||
Revision as of 17:56, 24 May 2020
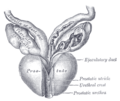
The seminal vesicles, abbreviated SV, are a pair of organs closely associated with the prostate gland that add fluid to the ejaculate. They are seen attached to radical prostatectomy specimens.
Normal seminal vesicles
General
- Seen in radical prostatectomies and occasionally in core biopsies.
- Very rarely a site of a primary cancer.
Gross
- Worm-like paired organs.
- Empty into the ejaculatory ducts (as does the vas deferens).
Relationship between the SVs, ejaculatory ducts and vas deferens.
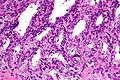
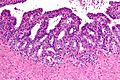
Microscopic
- Fern-like architecture - epithelial component clustered closely, looks like it connects.
- Epithelium surrounded by a thick layer of muscle (>10 cells across ~80 microns).
- Lipofuscin (coarse cytoplasmic yellow granules approximately 1-2 micrometers) - key feature.
- Nucleoli - common.
- Nuclear inclusions - common.[1]
Notes:
- The ejaculatory ducts have the same epithelium as the seminal vesicles.[2]
Images
www:
IHC
Sign out
B. PROSTATE, RIGHT MEDIAL SUPERIOR, BIOPSY: - BENIGN PROSTATE TISSUE. - BENIGN SEMINAL VESICLE/EJACULATORY DUCT.
Pathology
Primary seminal vesicle carcinoma
Main article: Primary seminal vesicle carcinoma
Amyloid in the seminal vesicles
Main article: Amyloid in the seminal vesicles
Benign
Stromal lipofuscinosis of the seminal vesicle
Main article: Stromal lipofuscinosis of the seminal vesicle
See also
References
- ↑ URL: http://surgpathcriteria.stanford.edu/prostate/adenocarcinoma/benign-vs-carcinoma.html. Accessed on: 10 January 2013.
- ↑ Leroy X, Ballereau C, Villers A, et al. (April 2003). "MUC6 is a marker of seminal vesicle-ejaculatory duct epithelium and is useful for the differential diagnosis with prostate adenocarcinoma". Am. J. Surg. Pathol. 27 (4): 519–21. PMID 12657938.
- ↑ Itami, Y.; Nagai, Y.; Kobayashi, Y.; Shimizu, N.; Yamamoto, Y.; Minami, T.; Hayashi, T.; Nozawa, M. et al. (Jul 2012). "[A case of prostatic cancer with a low PSA level accompanied with cystic formation requiring differentiation from adenocarcinoma of the seminal vesicle].". Hinyokika Kiyo 58 (7): 349-53. PMID 22895132.
- ↑ 4.0 4.1 Tarján, M.; Ottlecz, I.; Tot, T. (Jan 2009). "Primary adenocarcinoma of the seminal vesicle.". Indian J Urol 25 (1): 143-5. doi:10.4103/0970-1591.45557. PMID 19468449.
- ↑ 5.0 5.1 5.2 5.3 Terada, T. (2011). "Monstrous epithelial cell clusters in the seminal vesicle.". Int J Clin Exp Pathol 4 (7): 727-30. PMID 22076175.