|
|
| (40 intermediate revisions by 3 users not shown) |
| Line 1: |
Line 1: |
| '''Peripheral nerve sheath tumours''', abbreviated '''PNSTs''', are common in [[neuropathology]] and occasionally show-up elsewhere. A very common PNST is the [[Peripheral nerve sheath tumours#Schwannoma|schwannoma]]. | | '''Peripheral nerve sheath tumours''', abbreviated '''PNSTs''', are common in [[neuropathology]] and occasionally show-up elsewhere. A very common PNST is the [[schwannoma]]. |
|
| |
|
| =Classification= | | =Classification= |
| Line 13: |
Line 13: |
| =Specific diagnoses= | | =Specific diagnoses= |
| ==Schwannoma== | | ==Schwannoma== |
| ===General===
| | {{Main|Schwannoma}} |
| *A common [[neuropathology]] [[CNS tumours|tumour]] that occasionally shows-up elsewhere.
| |
| *Tumour of tissue surrounding a nerve.
| |
| **Axons adjacent to the tumour are normal... but may be compressed.
| |
| *May be a part of [[neurofibromatosis type 2]].
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid17893219>{{cite journal |author=Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A |title=Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns |journal=AJNR Am J Neuroradiol |volume=28 |issue=9 |pages=1633–8 |year=2007 |month=October |pmid=17893219 |doi=10.3174/ajnr.A0682 |url=http://www.ajnr.org/cgi/reprint/28/9/1633}}</ref>
| |
| *Antoni A:
| |
| **Cellular.
| |
| **'Fibrillary, polar, elongated'.
| |
| *Antoni B:
| |
| **Pauci-cellular.
| |
| **Loose microcystic tissue.
| |
| *Verocay bodies - paucinuclear area surrounded by nuclei - '''diagnostic feature'''.
| |
| *Hyaline thickened [[blood vessel]]s.
| |
| *Thick capsule.
| |
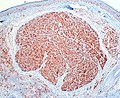
| *In the GI tract: classically have a ''peripheral lymphoid cuff''.<ref name=pmid15728600>{{cite journal |author=Levy AD, Quiles AM, Miettinen M, Sobin LH |title=Gastrointestinal schwannomas: CT features with clinicopathologic correlation |journal=AJR Am J Roentgenol |volume=184 |issue=3 |pages=797–802 |year=2005 |month=March |pmid=15728600 |doi= |url=http://www.ajronline.org/cgi/content/full/184/3/797}}</ref>
| |
| *+/-Hemosiderin deposition within tumour.
| |
| | |
| Notes:
| |
| *Tumour does ''not'' smear well.<ref>MUN. 24 November 2010.</ref>
| |
| *Antoni A: may look somewhat like scattered matchsticks.
| |
| | |
| DDx:
| |
| *[[Meningioma]].
| |
| *[[Intranodal palisaded myofibroblastoma]] - if surrounded by a rim of lymphoid tissue, i.e. [[Lymph node pathology|intranodal]].
| |
| *[[Leiomyoma]].
| |
| | |
| Images:
| |
| *www:
| |
| **[http://www.pathguy.com/~lulo/lulo0003.htm Antoni A (pathguy.com)].
| |
| **[http://www.ajnr.org/cgi/content/full/28/9/1633/F8 Antoni A & Antoni B side-by-side (ajnr.org)].
| |
| **[http://path.upmc.edu/cases/case639.html Cystic schwannoma - several images (upmc.edu)].
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Schwannoma_-_Antoni_A_and_B_-_intermed_mag.jpg Schwannoma - Antoni A & B - intermed. mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Schwannoma_-_Antoni_A_and_B_-_very_high_mag.jpg Scwhannoma - Antoni A & B - very high mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Psammomatous_melanotic_schwannoma_-_high_mag.jpg Psammomatous melanotic schwannoma - high mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Nerve_root_schwannoma_-_intermed_mag.jpg Nerve root schwannoma - intermed. mag. (WC)].
| |
| | |
| ====Schwannoma subtypes====
| |
| There are four:<ref name=pmid12792904>{{cite journal |author=Kurtkaya-Yapicier O, Scheithauer B, Woodruff JM |title=The pathobiologic spectrum of Schwannomas |journal=Histol. Histopathol. |volume=18 |issue=3 |pages=925–34 |year=2003 |month=July |pmid=12792904 |doi= |url=}}</ref>
| |
| #Conventional schwannoma.
| |
| #Cellular schwannoma.
| |
| #Plexiform schwannoma.
| |
| #Melanotic schwannoma.
| |
| | |
| =====Conventional schwannoma=====
| |
| *Most common.
| |
| | |
| =====Cellular schwannoma=====
| |
| *May mimic [[MPNST]].
| |
| | |
| Images:
| |
| *[http://path.upmc.edu/cases/case518.html Cellular schwannoma (upmc.edu)].
| |
| | |
| =====Plexiform schwannoma=====
| |
| *May mimic [[MPNST]] if cellular - esp. in childhood.
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Plexiform_Schwannoma_2.jpg Plexiform schwannoma - low mag. (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Plexiform_Schwannoma_1.jpg Plexiform schwannoma - high mag. (WC)].
| |
| | |
| =====Melanotic schwannoma=====
| |
| *May be confused with [[melanoma]].
| |
| *Psammomatous form (''psammomatous melanotic schwannoma'') associated with a heritable disorder ([[Carney complex]]).
| |
| | |
| Note:
| |
| *[[Carney complex]]:<ref name=pmid12792904/>
| |
| **Cutaneous lentigines.
| |
| **Myxomas (skin (subcutaneous), subcutanous, [[Atrial myxoma|heart]]).
| |
| **Endocrine neoplasms.
| |
| | |
| Images:
| |
| *[http://path.upmc.edu/cases/case387.html Psammomatous melanotic schwannoma - several images (upmc.edu)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid12692193>{{cite journal |author=Hirose T, Tani T, Shimada T, Ishizawa K, Shimada S, Sano T |title=Immunohistochemical demonstration of EMA/Glut1-positive perineurial cells and CD34-positive fibroblastic cells in peripheral nerve sheath tumors |journal=Mod. Pathol. |volume=16 |issue=4 |pages=293–8 |year=2003 |month=April |pmid=12692193 |doi=10.1097/01.MP.0000062654.83617.B7 |url=http://www.nature.com/modpathol/journal/v16/n4/full/3880761a.html }}</ref>
| |
| *S-100 +ve.
| |
| *Glut1 +ve.
| |
| *CD34 +ve.
| |
| *Cytokeratins ~70% +ve.{{fact}}
| |
| *SOX10 +ve.<ref name=pmid18636017>{{cite journal |author=Nonaka D, Chiriboga L, Rubin BP |title=Sox10: a pan-schwannian and melanocytic marker |journal=Am. J. Surg. Pathol. |volume=32 |issue=9 |pages=1291–8 |year=2008 |month=September |pmid=18636017 |doi=10.1097/PAS.0b013e3181658c14 |url=}}</ref>
| |
| **-ve in [[synovial sarcoma]], [[rhabdomyosarcoma]], [[chondrosarcoma]].
| |
| *EMA -ve. (???)
| |
| **Usually +ve (~75% of the time) in meningiomas.<ref>{{Cite journal | last1 = Rushing | first1 = EJ. | last2 = Bouffard | first2 = JP. | last3 = McCall | first3 = S. | last4 = Olsen | first4 = C. | last5 = Mena | first5 = H. | last6 = Sandberg | first6 = GD. | last7 = Thompson | first7 = LD. | title = Primary extracranial meningiomas: an analysis of 146 cases. | journal = Head Neck Pathol | volume = 3 | issue = 2 | pages = 116-30 | month = Jun | year = 2009 | doi = 10.1007/s12105-009-0118-1 | PMID = 19644540 }}
| |
| </ref>
| |
|
| |
|
| ==Perineurioma== | | ==Perineurioma== |
| ===General===
| | {{Main|Perineurioma}} |
| *Benign tumour derived from perineurial cells.
| |
| | |
| Variant:
| |
| *Reticular perineurioma.<ref name=pmid11257623>{{Cite journal | last1 = Graadt van Roggen | first1 = JF. | last2 = McMenamin | first2 = ME. | last3 = Belchis | first3 = DA. | last4 = Nielsen | first4 = GP. | last5 = Rosenberg | first5 = AE. | last6 = Fletcher | first6 = CD. | title = Reticular perineurioma: a distinctive variant of soft tissue perineurioma. | journal = Am J Surg Pathol | volume = 25 | issue = 4 | pages = 485-93 | month = Apr | year = 2001 | doi = | PMID = 11257623 }}</ref>
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_Sternberg5_424>{{Ref Sternberg5|424}}</ref>
| |
| *Perineural epithelioid cells.
| |
| **Abundant pale, fluffy appearing cytoplasm.
| |
| | |
| Note:
| |
| *May be intraneural.<ref name=Ref_Sternberg5_424>{{Ref Sternberg5|424}}</ref>
| |
| | |
| DDx:
| |
| *[[Neuroma]].
| |
| *[[Neurofibroma]].
| |
| *[[Schwannoma]].
| |
| **S100 +ve, EMA -ve.<ref name=Ref_Sternberg5_424>{{Ref Sternberg5|424}}</ref>
| |
| *[[Liposarcoma]] - reticular perineurioma.
| |
| | |
| Images:
| |
| *[http://www.conganat.org/seap/reuniones/almagro2000/scruz/tnerviog5.htm Perineuroma (conganat.org)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid15958848>{{Cite journal | last1 = Hornick | first1 = JL. | last2 = Fletcher | first2 = CD. | title = Soft tissue perineurioma: clinicopathologic analysis of 81 cases including those with atypical histologic features. | journal = Am J Surg Pathol | volume = 29 | issue = 7 | pages = 845-58 | month = Jul | year = 2005 | doi = | PMID = 15958848 }}</ref><ref name=pmid1497116>{{Cite journal | last1 = Tsang | first1 = WY. | last2 = Chan | first2 = JK. | last3 = Chow | first3 = LT. | last4 = Tse | first4 = CC. | title = Perineurioma: an uncommon soft tissue neoplasm distinct from localized hypertrophic neuropathy and neurofibroma. | journal = Am J Surg Pathol | volume = 16 | issue = 8 | pages = 756-63 | month = Aug | year = 1992 | doi = | PMID = 1497116 }}</ref>
| |
| *S100 -ve.
| |
| *EMA +ve.
| |
| *CD34 ~65% +ve.<ref name=pmid15958848/>
| |
|
| |
|
| ==Traumatic neuroma== | | ==Traumatic neuroma== |
| ===General===
| | :May be referred to as ''[[neuroma]]''. |
| *Consequence of trauma - diagnosis requires history of trauma.
| | {{Main|Traumatic neuroma}} |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_DCHH317>{{Ref DCHH|317}}</ref><ref name=pmid22330690/>
| |
| *+/-Nerve - that was injured.
| |
| *Grouping of disordered nerve fibre bundles in fibrous tissue (collagen) - '''key feature'''.
| |
| *+/-Myxoid change.
| |
| *+/-Axonal swellings (ovoid pink/purple blobs).
| |
| | |
| DDx:
| |
| *[[Morton neuroma]] (foot).
| |
| | |
| Images:
| |
| *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296625/figure/F2/ Traumatic neuroma (nih.gov)].<ref name=pmid22330690>{{Cite journal | last1 = Li | first1 = Q. | last2 = Gao | first2 = EL. | last3 = Yang | first3 = YL. | last4 = Hu | first4 = HY. | last5 = Hu | first5 = XQ. | title = Traumatic neuroma in a patient with breast cancer after mastectomy: a case report and review of the literature. | journal = World J Surg Oncol | volume = 10 | issue = | pages = 35 | month = | year = 2012 | doi = 10.1186/1477-7819-10-35 | PMID = 22330690 }}</ref>
| |
| *[http://path.upmc.edu/cases/case502.html Traumatic neuroma - several images (upmc.edu)].
| |
| *[http://www.sarcomaimages.com/index.php?v=Neuroma,-Traumatic Traumatic neuroma (sarcomaimages.com)].
| |
| *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627419/figure/F1/ Traumatic neuroma (nih.gov)].<ref name=pmid17554193>{{Cite journal | last1 = Kwon | first1 = JH. | last2 = Ryu | first2 = SW. | last3 = Kang | first3 = YN. | title = Traumatic neuroma around the celiac trunk after gastrectomy mimicking a nodal metastasis: a case report. | journal = Korean J Radiol | volume = 8 | issue = 3 | pages = 242-5 | month = | year = | doi = | PMID = 17554193 | PMC = 2627419 }}</ref>
| |
| | |
| ===Sign out===
| |
| <pre>
| |
| SOFT TISSUE LESION, RIGHT WRIST, EXCISION:
| |
| - TRAUMATIC NEUROMA.
| |
| - BENIGN FIBROADIPOSE TISSUE.
| |
| </pre>
| |
| | |
| ====Micro====
| |
| The sections show disordered nerve fibre bundles in fibrous tissue.
| |
|
| |
|
| ==Palisaded encapsulated neuroma== | | ==Palisaded encapsulated neuroma== |
| *Abbreviated ''PEN''. | | *Abbreviated ''PEN''. |
| *[[AKA]] ''palisaded and encapsulated neuroma''. | | *[[AKA]] ''palisaded and encapsulated neuroma''. |
| | *[[AKA]] ''solitary circumscribed neuroma''. |
| | |
| ===General=== | | ===General=== |
| *Flesh-colour [[papule]] - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> | | *Flesh-colour [[papule]] - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> |
| *Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | | *Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> |
| *Superficial skin.<ref>S. Sade. 8 September 2011.</ref> | | *Superficial skin papule.<ref>S. Sade. 8 September 2011.</ref> |
| | *It is considered hyperplastic rather than neoplastic. <ref>Rosai & Ackermann, Surgical Pathology, 10th ed. p183</ref> |
|
| |
|
| ===Microscopic=== | | ===Microscopic=== |
| Line 177: |
Line 40: |
| **#Not vacuolated. | | **#Not vacuolated. |
| **#Nuclei have pointy ends. | | **#Nuclei have pointy ends. |
| | **#Sometimes epitheloid appearance. |
| *Intralesional clefts. | | *Intralesional clefts. |
| **Useful to differentiate from schwannoma. | | **Useful to differentiate from schwannoma. |
| Line 191: |
Line 55: |
| Images: | | Images: |
| *[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | | *[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> |
| | |
| | <gallery> |
| | File:Palisaded_and_Encapsulated_Neuroma_(3952635881).jpg | Palisaded and encapsulated neuroma (Ed Uthman) |
| | File:Palisaded_and_Encapsulated_Neuroma,_S-100_Immunostain_(3953412396).jpg| PEN, S-100 staining (Ed Uthman) |
| | |
| | </gallery> |
| | [[File:569 dp sl 1.png| Palisading/encapcuslated neuroma]] |
| | [[File:569 dp sl 2.png| Palisading/encapcuslated neuroma]]<br> |
| | Palisading/encapsulated (Reed’s) neuroma. A. A dermal nodule shows an attenuated capsule (black arrows) about a fasciculated spindle cell lesion with artefactual clefts (green arrows). B. The bland spindled nuclei, amid clear cytoplasm with thin eosinophilic wisps, are often wavy (black arrows), with pointed ends (green arrows); leiomyomas have blunt ended nuclei and more eosinophilic cytoplasm. These benign neoplasms, unlike neurofibromas, lack an association with neurofibromatosis. |
|
| |
|
| ===IHC=== | | ===IHC=== |
| Line 198: |
Line 71: |
|
| |
|
| ==Neurofibroma== | | ==Neurofibroma== |
| ===General===
| | {{Main|Neurofibroma}} |
| *May be a part of [[neurofibromatosis]] 1 (NF1).
| | Includes discussion of ''plexiform neurofibroma''. |
| *A [[painful skin lesion]].
| |
| *Composed of Schwann cells, axons, fibrous material.<ref name=pmid17893219/>
| |
| | |
| Classification:<ref name=pmid15486243>{{Cite journal | last1 = Wilkinson | first1 = LM. | last2 = Manson | first2 = D. | last3 = Smith | first3 = CR. | title = Best cases from the AFIP: plexiform neurofibroma of the bladder. | journal = Radiographics | volume = 24 Suppl 1 | issue = | pages = S237-42 | month = Oct | year = 2004 | doi = 10.1148/rg.24si035170 | PMID = 15486243 }}</ref>
| |
| #Localized - sporatic.
| |
| #Diffuse - usually poorly defined, young adults and children; sporatic.
| |
| #Plexiform - associated with NF1.
| |
| | |
| ===Gross/radiologic===
| |
| Gross features (plexiform NF):<ref name=pmid15486243>{{Cite journal | last1 = Wilkinson | first1 = LM. | last2 = Manson | first2 = D. | last3 = Smith | first3 = CR. | title = Best cases from the AFIP: plexiform neurofibroma of the bladder. | journal = Radiographics | volume = 24 Suppl 1 | issue = | pages = S237-42 | month = Oct | year = 2004 | doi = 10.1148/rg.24si035170 | PMID = 15486243 }}</ref>
| |
| *"Bag of worms" appearance.
| |
| | |
| Radiologic:<ref name=pmid15486243/>
| |
| *Fusiform mass.
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Spindle cells with wavy nuclei without pleomorphism - '''key feature'''.
| |
| **Often described as "shredded carrots".
| |
| *May be arranged in fascicles and intermixed with collagen.
| |
| **Often no pattern is apparent.
| |
| *Moderate increase of cellularity vis-a-vis normal dermis.
| |
| *May be poorly or well-circumscribed.
| |
| *+/-Plexiform growth pattern - "bag of worms".<ref name=pmid17893219/>
| |
| **Multiple well-circumscribed nests.
| |
| *Mast cells<ref name=pmid20233971>{{Cite journal | last1 = Staser | first1 = K. | last2 = Yang | first2 = FC. | last3 = Clapp | first3 = DW. | title = Mast cells and the neurofibroma microenvironment. | journal = Blood | volume = 116 | issue = 2 | pages = 157-64 | month = Jul | year = 2010 | doi = 10.1182/blood-2009-09-242875 | PMID = 20233971 }}</ref> - one has to look for them at high power.
| |
| **Very useful for confirming the low power suspicion.
| |
| | |
| DDx:
| |
| *[[Schwannoma]].
| |
| *[[Dermatofibrosarcoma protuberans]] (DFSP) - S-100 -ve, CD34 +ve.
| |
| *[[Ganglioneuroma]].
| |
| | |
| Images:
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Neurofibroma_(1).jpg Neurofibroma - low mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Neurofibroma_(2).jpg Neurofibroma - high mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Neurofibroma_(3).jpg Neurofibroma - high mag. (WC)].
| |
| *www:
| |
| **[http://radiographics.rsna.org/content/24/suppl_1/S237/F9.expansion.html Plexiform neurofibroma (rsna.org)].
| |
| **[http://radiographics.rsna.org/content/24/suppl_1/S237/F10.expansion.html Plexiform neurofibroma (rsna.org)].
| |
| *[http://path.upmc.edu/cases/case304/micro.html Plexiform neurofibroma - several images (upmc.edu)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid12692193>{{cite journal |author=Hirose T, Tani T, Shimada T, Ishizawa K, Shimada S, Sano T |title=Immunohistochemical demonstration of EMA/Glut1-positive perineurial cells and CD34-positive fibroblastic cells in peripheral nerve sheath tumors |journal=Mod. Pathol. |volume=16 |issue=4 |pages=293–8 |year=2003 |month=April |pmid=12692193 |doi=10.1097/01.MP.0000062654.83617.B7 |url=http://www.nature.com/modpathol/journal/v16/n4/full/3880761a.html }}</ref>
| |
| *S100 +ve.
| |
| *CD34 +ve.
| |
| *Glut1 +ve.
| |
| *EMA +ve/-ve.
| |
|
| |
|
| ==Neurothekeoma== | | ==Neurothekeoma== |
| *[[AKA]] ''myxoma of the nerve sheath'', [[AKA]] ''nerve sheath myxoma''.
| | {{Main|Neurothekeoma}} |
| ===General===
| |
| *Rare.
| |
| *Female > male.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid17325474>{{cite journal |author=Hornick JL, Fletcher CD |title=Cellular neurothekeoma: detailed characterization in a series of 133 cases |journal=Am. J. Surg. Pathol. |volume=31 |issue=3 |pages=329–40 |year=2007 |month=March |pmid=17325474 |doi=10.1097/01.pas.0000213360.03133.89 |url=}}</ref>
| |
| *Superficial dermal lesion:
| |
| **Usu. lobulated or micronodular architecture - '''key feature'''.
| |
| ***+/-Focal sheeting.
| |
| **Spindle/epithelioid morphology with pale eosinophilic cytoplasm - '''key feature'''.
| |
| **+/-Inflammation around lesion.
| |
| **+/-Surrounded by collagen.
| |
| | |
| Notes:
| |
| *No atypia.
| |
| *Mitoses rare/none.
| |
| *Often poorly circumscribed.
| |
| | |
| Subtypes:<ref name=pmid10555009>{{cite journal |author=Wang AR, May D, Bourne P, Scott G |title=PGP9.5: a marker for cellular neurothekeoma |journal=Am. J. Surg. Pathol. |volume=23 |issue=11 |pages=1401–7 |year=1999 |month=November |pmid=10555009 |doi= |url=}}</ref>
| |
| *Cellular.
| |
| *[[Myxoid]].
| |
| *Intermediate.
| |
| | |
| DDx:
| |
| *[[Dermatofibroma]].
| |
| *[[Angiomatoid fibrous histiocytoma]] -- have cystic blood filled spaces, inflammation.<ref>URL: [http://surgpathcriteria.stanford.edu/softfib/angiomatoid_fibrous_histiocytoma/ http://surgpathcriteria.stanford.edu/softfib/angiomatoid_fibrous_histiocytoma/]. Accessed on: 11 May 2011.</ref>
| |
| | |
| Images:
| |
| *[http://en.wikipedia.org/wiki/File:Neurothekeoma2.JPG Neurothekeoma (WP)].
| |
| *[http://path.upmc.edu/cases/case586.html Neurothekeoma - several images (upmc.edu)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid17325474/>
| |
| *NKI/C3 ([[AKA]] NKI-C3) +ve.
| |
| *NSE +/-ve.
| |
| | |
| Others:<ref name=pmid17592278>{{cite journal |author=Fetsch JF, Laskin WB, Hallman JR, Lupton GP, Miettinen M |title=Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information |journal=Am. J. Surg. Pathol. |volume=31 |issue=7 |pages=1103–14 |year=2007 |month=July |pmid=17592278 |doi=10.1097/PAS.0b013e31802d96af |url=}}</ref>
| |
| *Vimentin +ve.
| |
| *CD10 +ve.
| |
| *Microphthalmia transcription factor +ve.
| |
| *PGP9.5 +ve.
| |
| | |
| Exclusionary:
| |
| *S100 -ve.
| |
| **Exclude other peripheral nerve sheath tumours. (???)
| |
|
| |
|
| ==Malignant peripheral nerve sheath tumour== | | ==Malignant peripheral nerve sheath tumour== |
| *[[AKA]] ''neurofibrosarcoma''.<ref name=pmid21317712>{{Cite journal | last1 = Mills | first1 = AM. | last2 = Karamchandani | first2 = JR. | last3 = Vogel | first3 = H. | last4 = Longacre | first4 = TA. | title = Endocervical fibroblastic malignant peripheral nerve sheath tumor (neurofibrosarcoma): report of a novel entity possibly related to endocervical CD34 fibrocytes. | journal = Am J Surg Pathol | volume = 35 | issue = 3 | pages = 404-12 | month = Mar | year = 2011 | doi = 10.1097/PAS.0b013e318208f72e | PMID = 21317712 }}</ref>
| | {{Main|Malignant peripheral nerve sheath tumour}} |
| *Commonly abbreviated ''MPNST''.
| |
| | |
| ===General===
| |
| *Malignant - as the name implies.
| |
| *Usu. assoc. with a peripheral nerve.{{Fact}}
| |
| *May be seen in the context of [[neurofibromatosis type 1]].
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Cellular.
| |
| *Nuclear atypia.
| |
| *Mitoses.
| |
| *+/-Herring bone pattern.
| |
| | |
| Notes:
| |
| *May be diagnosed in a poorly diff. tumour if patient has [[NF1]].
| |
| | |
| DDx:
| |
| *Cellular [[schwannoma]].
| |
| *Plexiform schwannoma.
| |
| *[[Malignant triton tumour]].
| |
| | |
| DDx of herring bone:
| |
| *MPNST.
| |
| *[[Synovial sarcoma]].
| |
| *[[Fibrosarcoma]].
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Malignant_peripheral_nerve_sheath_tumour_-_intermed_mag.jpg MPNST - intermed. mag. (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Malignant_peripheral_nerve_sheath_tumour_-_high_mag.jpg MPNST - high mag. (WC)].
| |
| *[http://path.upmc.edu/cases/case112/micro.html MPNST - several images (upmc.edu)].
| |
| *[http://path.upmc.edu/cases/case406.html MPNST - case 2 - several images (upmc.edu)].
| |
| | |
| ====Grading====
| |
| *Can be graded histologically,<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref> and this is prognostic.<ref name=pmid16923196>{{cite journal |author=Kar M, Deo SV, Shukla NK, ''et al.'' |title=Malignant peripheral nerve sheath tumors (MPNST)--clinicopathological study and treatment outcome of twenty-four cases |journal=World J Surg Oncol |volume=4 |issue= |pages=55 |year=2006 |pmid=16923196 |pmc=1560134 |doi=10.1186/1477-7819-4-55 |url=}}</ref>
| |
| | |
| Sarcoma grading system<ref name=pmid6693192>{{cite journal |author=Trojani M, Contesso G, Coindre JM, ''et al.'' |title=Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system |journal=Int. J. Cancer |volume=33 |issue=1 |pages=37–42 |year=1984 |month=January |pmid=6693192 |doi= |url=}}</ref> - based on:
| |
| *Tumour differentiation.
| |
| *Mitotic rate.
| |
| *[[Necrosis]].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid18636017>{{cite journal |author=Nonaka D, Chiriboga L, Rubin BP |title=Sox10: a pan-schwannian and melanocytic marker |journal=Am. J. Surg. Pathol. |volume=32 |issue=9 |pages=1291–8 |year=2008 |month=September |pmid=18636017 |doi=10.1097/PAS.0b013e3181658c14 |url=}}</ref>
| |
| *S-100 +ve ~ 30% of tumours.
| |
| *SOX10 +ve ~ 50% of tumours.
| |
| | |
| Others:<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref>
| |
| *p53.
| |
| *p16.
| |
| *p27.
| |
| *MIB1.
| |
|
| |
|
| ==Malignant triton tumour== | | ==Malignant triton tumour== |
| Line 397: |
Line 125: |
|
| |
|
| ==Morton neuroma== | | ==Morton neuroma== |
| ===General=== | | :[[AKA]] ''plantar interdigital neuroma''.<ref name=pmid22995258>{{Cite journal | last1 = Makki | first1 = D. | last2 = Haddad | first2 = BZ. | last3 = Mahmood | first3 = Z. | last4 = Shahid | first4 = MS. | last5 = Pathak | first5 = S. | last6 = Garnham | first6 = I. | title = Efficacy of corticosteroid injection versus size of plantar interdigital neuroma. | journal = Foot Ankle Int | volume = 33 | issue = 9 | pages = 722-6 | month = Sep | year = 2012 | doi = DOI: 10.3113/FAI.2012.0722 | PMID = 22995258 }}</ref> |
| *Benign foot condition.
| | {{Main|Morton neuroma}} |
| *Uncommon.
| |
| *Usu. interdigital nerves.
| |
| | |
| Etiology:
| |
| *Indirect nerve trauma.
| |
| | |
| Clinical:<ref name=Ref_Sternberg4>{{Ref Sternberg4|243}}</ref>
| |
| *Foot pain.
| |
| | |
| ===Microscopic=== | |
| Features:<ref name=Ref_Sternberg4>{{Ref Sternberg4|243}}</ref>
| |
| *Extensive fibrosis around and within the nerve.
| |
| *Digital artery:
| |
| **+/-[[Thrombosis]].
| |
| **+/-Arterial thickening.
| |
| | |
| DDx:
| |
| *[[Traumatic neuroma]].
| |
| | |
| Image:
| |
| *[http://www.tumorlibrary.com/case/detail.jsp?image_id=2324 Morton neuroma (tumorlibrary.com)].
| |
|
| |
|
| =See also= | | =See also= |
| Line 429: |
Line 136: |
|
| |
|
| [[Category:Neuropathology]] | | [[Category:Neuropathology]] |
| | [[Category:Peripheral nerve sheath tumours]] |