Difference between revisions of "Serous cystadenoma of the ovary"
(→Images) |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 48: | Line 48: | ||
Cystadenofibroma and adenofibroma:<ref name=pmid23171527>{{Cite journal | last1 = Takeuchi | first1 = M. | last2 = Matsuzaki | first2 = K. | last3 = Harada | first3 = M. | title = Ovarian adenofibromas and cystadenofibromas: magnetic resonance imaging findings including diffusion-weighted imaging. | journal = Acta Radiol | volume = 54 | issue = 2 | pages = 231-6 | month = Mar | year = 2013 | doi = 10.1258/ar.2012.120516 | PMID = 23171527 }}</ref> | Cystadenofibroma and adenofibroma:<ref name=pmid23171527>{{Cite journal | last1 = Takeuchi | first1 = M. | last2 = Matsuzaki | first2 = K. | last3 = Harada | first3 = M. | title = Ovarian adenofibromas and cystadenofibromas: magnetic resonance imaging findings including diffusion-weighted imaging. | journal = Acta Radiol | volume = 54 | issue = 2 | pages = 231-6 | month = Mar | year = 2013 | doi = 10.1258/ar.2012.120516 | PMID = 23171527 }}</ref> | ||
*Solid or solid and cystic. | *Solid or solid and cystic. | ||
Note: | |||
*Cystic lesions must be >=1 cm in size, smaller lesions are ''surface epithelial inclusion cysts''.<ref name=Ref_GP384>{{Ref GP|384}}</ref> | |||
===Image=== | ===Image=== | ||
| Line 54: | Line 57: | ||
==Microscopic== | ==Microscopic== | ||
Features:<ref name=Ref_GP396>{{Ref GP|396}}</ref> | Features:<ref name=Ref_GP396>{{Ref GP|396}}</ref> | ||
*Simple epithelium | *Simple epithelium - '''key feature''' - usually with cilia. | ||
**Cell morphology: columnar, cuboidal or flatted. | **Cell morphology: columnar, cuboidal or flatted. | ||
*Absent or minimal [[nuclear atypia]]. | *Absent or minimal [[nuclear atypia]]. | ||
| Line 65: | Line 68: | ||
DDx: | DDx: | ||
*Cortical inclusion cyst - see ''[[mesothelial inclusion cyst]]''. | *Cortical inclusion cyst - <1 cm in size, see ''[[mesothelial inclusion cyst]]''. | ||
*[[Ovarian serous borderline tumour]] - branching papillae, tufting, mitoses, nuclear atypia. | *[[Ovarian serous borderline tumour]] - branching papillae, tufting, mitoses, nuclear atypia. | ||
| Line 73: | Line 76: | ||
===Images=== | ===Images=== | ||
====Serous cystadenoma==== | |||
<gallery> | <gallery> | ||
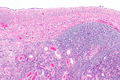
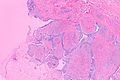
Image: Ovarian serous cystadenoma - alt -- low mag.jpg | OSC - low mag. | Image: Ovarian serous cystadenoma - alt -- low mag.jpg | OSC - low mag. | ||
| Line 82: | Line 86: | ||
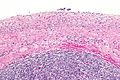
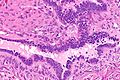
Image: Ovarian serous cystadenoma -- extremely high mag.jpg | OSC - extremely high mag. | Image: Ovarian serous cystadenoma -- extremely high mag.jpg | OSC - extremely high mag. | ||
</gallery> | </gallery> | ||
www | ====Serous cystadenofibroma==== | ||
<gallery> | |||
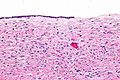
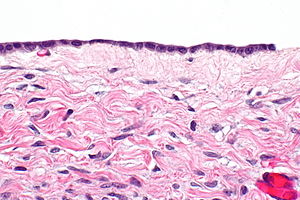
Image: Serous cystadenofibroma -- very low mag.jpg | SCAF - very low mag. | |||
Image: Serous cystadenofibroma -- low mag.jpg | SCAF - low mag. | |||
Image: Serous cystadenofibroma -- intermed mag.jpg | SCAF - intermed. mag. | |||
Image: Serous cystadenofibroma -- high mag.jpg | SCAF - high mag. | |||
</gallery> | |||
=====www===== | |||
*[http://www.webpathology.com/image.asp?case=525&n=4 Serous cystadenofibroma - low mag. (webpathology.com)]. | *[http://www.webpathology.com/image.asp?case=525&n=4 Serous cystadenofibroma - low mag. (webpathology.com)]. | ||
*[http://www.webpathology.com/image.asp?n=5&Case=525 Serous cystadenofibroma - high mag. (webpathology.com)]. | *[http://www.webpathology.com/image.asp?n=5&Case=525 Serous cystadenofibroma - high mag. (webpathology.com)]. | ||
==IHC== | |||
Features:<ref name=Ref_GP396/> | |||
*CK7 +ve. | |||
*EMA +ve. | |||
*WT1 +ve. | |||
*CK20 -ve. | |||
==Sign out== | ==Sign out== | ||
| Line 127: | Line 145: | ||
lesion is best classified as benign with focal atypia. | lesion is best classified as benign with focal atypia. | ||
</pre> | </pre> | ||
===Micro=== | |||
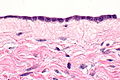
The sections show fibrous tissue consistent with a cyst wall lined by a simple columnar to flat epithelium, focally with cilia. | |||
Cautery is present imparting a pseudostratified appearance focally. No definite papillae or definite tufting is apparent. No significant nuclear atypia is seen. Mitotic activity is not apparent. | |||
==See also== | ==See also== | ||
Latest revision as of 03:20, 7 June 2016
| Serous cystadenoma of the ovary | |
|---|---|
| Diagnosis in short | |
 Ovarian serous cystadenoma. H&E stain. | |
|
| |
| LM | cyst lined by a single layer of cuboidal or columnar epithelium with bland nuclear features +/- cilia |
| Subtypes | cystadenofibroma, adenofibroma |
| Gross | cystadenoma: thin walled cyst, usu. unilocular; cystadenofibroma and adenofibroma: solid and cystic or solid |
| Site | ovary - see ovarian tumours |
|
| |
| Clinical history | +/-abdominal distension, +/-abdominal pain |
| Symptoms | mass lesion |
| Prevalence | common |
| Prognosis | benign |
| Clin. DDx | other ovarian tumours |
| Treatment | cystectomy or oophorectomy |
Serous cystadenoma of the ovary is a common benign finding in the ovary.
It is also known as ovarian serous cystadenoma. It is unrelated the pancreatic serous cystadenoma.
Serous cystadenofibroma and adenofibroma of the ovary can be considered variants, and are also dealt with in this article.
General
- Benign.
- Very common.
- Not related to the serous cystadenoma of the pancreas.
- Thought to arise from a cortical inclusion cyst that has undergone Muellerian metaplasia[1][2] - see mesothelial inclusion cyst.
Gross
Cystadenoma:
- Usually unilocular.
Cystadenofibroma and adenofibroma:[3]
- Solid or solid and cystic.
Note:
- Cystic lesions must be >=1 cm in size, smaller lesions are surface epithelial inclusion cysts.[4]
Image
Microscopic
Features:[5]
- Simple epithelium - key feature - usually with cilia.
- Cell morphology: columnar, cuboidal or flatted.
- Absent or minimal nuclear atypia.
- +/-Rare tufting.
- +/-Non-branching papillae.
- +/-Rare mitoses.
Note:
- May have calcifications - uncommon.[6]
DDx:
- Cortical inclusion cyst - <1 cm in size, see mesothelial inclusion cyst.
- Ovarian serous borderline tumour - branching papillae, tufting, mitoses, nuclear atypia.
Note - the following may be lumped with this entity:
- Serous cystadenofibroma.
- Adenofibroma.
Images
Serous cystadenoma
Serous cystadenofibroma
www
- Serous cystadenofibroma - low mag. (webpathology.com).
- Serous cystadenofibroma - high mag. (webpathology.com).
IHC
Features:[5]
- CK7 +ve.
- EMA +ve.
- WT1 +ve.
- CK20 -ve.
Sign out
OVARY, LEFT, CYSTECTOMY: - BENIGN SEROUS CYSTADENOMA.
FALLOPIAN TUBE AND (PARTIAL) OVARY, LEFT, RESECTION: - COMPATIBLE WITH SEROUS CYSTADENOMA. - BENIGN OVARIAN PARENCHYMA WITH FOCAL EDEMA AND A BENIGN CALCIFICATION. - FALLOPIAN TUBE WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
Cystadenofibroma
FALLOPIAN TUBE AND OVARY, LEFT, UNILATERAL SALPINGO-OOPHORECTOMY: - OVARY WITH BENIGN SEROUS CYSTADENOFIBROMA. - FALLOPIAN TUBE WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
FALLOPIAN TUBES AND OVARIES, BILATERAL SALPINGO-OOPHRECTOMY: - BENIGN OVARIAN SEROUS CYSTADENOFIBROMA (BILATERAL). - FALLOPIAN TUBES WITHIN NORMAL LIMITS.
Atypical
FALLOPIAN TUBE AND OVARY, RIGHT, SALPINGO-OOPHORECTOMY: - BENIGN SEROUS CYSTADENOMA AND SEROUS CYSTADENOFIBROMA WITH FOCAL ATYPIA, SEE COMMENT. - FALLOPIAN TUBE WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY. COMMENT: A small focus of the sampled tissue has a complex architecture, compatible with a borderline tumour; however, it represents less than 10% of the lesion. Thus, the lesion is best classified as benign with focal atypia.
Micro
The sections show fibrous tissue consistent with a cyst wall lined by a simple columnar to flat epithelium, focally with cilia.
Cautery is present imparting a pseudostratified appearance focally. No definite papillae or definite tufting is apparent. No significant nuclear atypia is seen. Mitotic activity is not apparent.
See also
References
- ↑ Feeley, KM.; Wells, M. (Feb 2001). "Precursor lesions of ovarian epithelial malignancy.". Histopathology 38 (2): 87-95. PMID 11207821.
- ↑ Okamoto, S.; Okamoto, A.; Nikaido, T.; Saito, M.; Takao, M.; Yanaihara, N.; Takakura, S.; Ochiai, K. et al. (May 2009). "Mesenchymal to epithelial transition in the human ovarian surface epithelium focusing on inclusion cysts.". Oncol Rep 21 (5): 1209-14. PMID 19360296.
- ↑ Takeuchi, M.; Matsuzaki, K.; Harada, M. (Mar 2013). "Ovarian adenofibromas and cystadenofibromas: magnetic resonance imaging findings including diffusion-weighted imaging.". Acta Radiol 54 (2): 231-6. doi:10.1258/ar.2012.120516. PMID 23171527.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 384. ISBN 978-0443069208.
- ↑ 5.0 5.1 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 396. ISBN 978-0443069208.
- ↑ Okada, S.; Ohaki, Y.; Inoue, K.; Kawamura, T.; Hayashi, T.; Kato, T.; Kumazaki, T. (Feb 2005). "Calcifications in mucinous and serous cystic ovarian tumors.". J Nippon Med Sch 72 (1): 29-33. PMID 15834205.