Difference between revisions of "Esophageal adenocarcinoma"
Jump to navigation
Jump to search
(+bx) |
|||
| Line 110: | Line 110: | ||
==Sign out== | ==Sign out== | ||
===Biopsy=== | |||
<pre> | |||
Esophagus, Biopsy: | |||
- INVASIVE ADENOCARCINOMA, poorly differentiated. | |||
Comment: | |||
Pending IHC (CK7, CK20) and HER2 testing; results of these will be reported in an addendum. | |||
</pre> | |||
===Resection=== | |||
<pre> | <pre> | ||
GASTROESOPHAGEAL JUNCTION, RESECTION: | GASTROESOPHAGEAL JUNCTION, RESECTION: | ||
Revision as of 18:14, 11 April 2016
| Esophageal adenocarcinoma | |
|---|---|
| Diagnosis in short | |
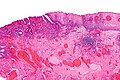
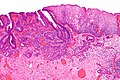
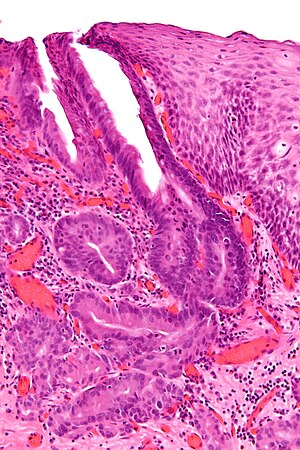 Esophageal adenocarcinoma. H&E stain. | |
|
| |
| LM | "invading" cell clusters or glands (gland cribriforming (more than rare) or desmoplasia or submucosa invasion); nuclear atypia of malignancy (variation of size, shape, staining), +/-mitoses |
| LM DDx | high-grade columnar dysplasia of the esophagus, squamous cell carcinoma of the esophagus,gastric adenocarcinoma |
| IHC | CK7 +ve, CK20 +ve, p63 -ve |
| Site | esophagus |
|
| |
| Associated Dx | Barrett's esophagus, high-grade columnar dysplasia of the esophagus |
| Symptoms | dysphagia |
| Prevalence | uncommon |
| Prognosis | often poor - as typically high stage at diagnosis |
| Treatment | EMR (early), surgery - esophagectomy |
Esophageal adenocarcinoma, also adenocarcinoma of the esophagus, is a common malignant epithelial-derived tumour of the distal esophagus, that classically arises in the context of Barrett's esophagus.
General
- Often a prognosis poor - as diagnosed in a late stage.
- May be difficult to distinguish from adenocarcinoma of the stomach.
- By convention (in the CAP checklist) gastroesophageal junction carcinomas are staged as esophageal carcinomas.[1]
Symptoms:
- Dysphagia - difficulty swallowing.
Associations:
- Barrett's esophagus.
- Hiatal hernia.[2]
- Family history - prostate cancer.[2]
Treatment
- Adenocarcinoma in situ (AIS) - may be treated with endoscopic mucosal resection & follow-up.[3]
- Surgery - esophagectomy.
Esophagus versus stomach
The convention is it's esophageal if both of the following are true:[4]
- Epicenter of tumour is in the esophagus.
- Barrett's mucosa is present.
Microscopic
Features:
- Adenocarcinoma:
- "Invading" cell clusters or glands.
- Cribriforming (more than rare) or desmoplasia or "deep" invasion (into submucosa).
- Nuclear atypia of malignancy:
- Size variation.
- Shape variation.
- Staining variation.
- +/-Mitoses (common).
- "Invading" cell clusters or glands.
DDx:
- High-grade columnar dysplasia of the esophagus - see table in esophagus article
- Squamous cell carcinoma of the esophagus.
- Gastric adenocarcinoma.
Images
Grading
Graded like other adenocarcinoma:[4]
- >95 % of tumour in glandular arrangement = well-differentiated.
- 95-50% of tumour in glandular arrangement= moderately-differentiated.
- <50% of tumour in glandular arrangment = poorly-differentiated.
Staging
Early esophageal adenocarcinoma has its own staging system:[5][6]
- M1 = lamina propria.
- M2 = superficial muscularis mucosae.
- M3 = submucosa.
- M4 = muscularis propria.
IHC
- CK7 +ve.
- CK20 +ve.
To rule-out SCC:
- p63 -ve.
- HWMK -ve.
Others:[7]
- p53 +ve.
- COX-2 +ve.
- p16 +ve - but not that useful as it's frequently positive in the precursors.[8]
Staging
- The number of lymph nodes is important for staging, as a small number may lead to stage migration (Will Rogers phenomenon).
- There is no established standard for esophageal cancer (as per UICC/AJCC staging - based on Li et al.[9]), several studies give different numbers (18 lymph nodes Greenstein et al.,[10] 23 lymph nodes Peyre et al.[11]).
Sign out
Biopsy
Esophagus, Biopsy: - INVASIVE ADENOCARCINOMA, poorly differentiated. Comment: Pending IHC (CK7, CK20) and HER2 testing; results of these will be reported in an addendum.
Resection
GASTROESOPHAGEAL JUNCTION, RESECTION: - INTRAMUCOSAL ADENOCARCINOMA, pT1a, pNx, SEE TUMOUR SUMMARY. -- MUCOSAL MARGIN HAS CAUTERIZED DYSPLASTIC EPITHELIUM, SEE COMMENT. -- DEEP MARGIN NEGATIVE FOR MALIGNANCY. COMMENT: The cauterized dysplastic epithelium cannot be further interpreted. Malignant-appearing glands are within 1 mm of the cauterized epithelium. Close follow-up and re-biopsy (or endoscopic re-resection if clinically indicated) is recommended. This case was partially reviewed internally. There is agreement on the presence of intramucosal adenocarcinoma and dysplastic epithelium at the mucosal margin.
See also
References
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Esophagus_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ 2.0 2.1 Jiang X, Tseng CC, Bernstein L, Wu AH (2014). "Family history of cancer and gastroesophageal disorders and risk of esophageal and gastric adenocarcinomas: a case-control study". BMC Cancer 14: 60. doi:10.1186/1471-2407-14-60. PMC 3915076. PMID 24495377. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3915076/.
- ↑ Sampliner, RE. (Jul 2009). "Endoscopic therapy for Barrett's esophagus.". Clin Gastroenterol Hepatol 7 (7): 716-20. doi:10.1016/j.cgh.2009.03.011. PMID 19306943.
- ↑ 4.0 4.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 168. ISBN 978-0781765275.
- ↑ Pech, O.; May, A.; Rabenstein, T.; Ell, C. (Nov 2007). "Endoscopic resection of early oesophageal cancer.". Gut 56 (11): 1625-34. doi:10.1136/gut.2006.112110. PMC 2095648. PMID 17938435. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2095648/.
- ↑ Thosani, N.; Singh, H.; Kapadia, A.; Ochi, N.; Lee, JH.; Ajani, J.; Swisher, SG.; Hofstetter, WL. et al. (Nov 2011). "Diagnostic accuracy of EUS in differentiating mucosal versus submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis.". Gastrointest Endosc. doi:10.1016/j.gie.2011.09.016. PMID 22115605.
- ↑ Liu, YS.; Yu, CH.; Li, L.; Zhang, BF.; Fang, J.; Zhou, Q.; Hu, Y.; Li, YM. et al. (Aug 2007). "Expression of p53, p16 and cyclooxygenase-2 in esophageal cancer with tissue microarray.". J Dig Dis 8 (3): 133-8. doi:10.1111/j.1443-9573.2007.00299.x. PMID 17650224.
- ↑ Hardie, LJ.; Darnton, SJ.; Wallis, YL.; Chauhan, A.; Hainaut, P.; Wild, CP.; Casson, AG. (Jan 2005). "p16 expression in Barrett's esophagus and esophageal adenocarcinoma: association with genetic and epigenetic alterations.". Cancer Lett 217 (2): 221-30. doi:10.1016/j.canlet.2004.06.025. PMID 15617840.
- ↑ Li, Q.; Wu, SG.; Gao, JM.; Xu, JJ.; Hu, LY.; Xu, T. (Mar 2013). "Impact of esophageal cancer staging on overall survival and disease-free survival based on the 2010 AJCC classification by lymph nodes.". J Radiat Res 54 (2): 307-14. doi:10.1093/jrr/rrs096. PMID 23124992.
- ↑ Greenstein, AJ.; Litle, VR.; Swanson, SJ.; Divino, CM.; Packer, S.; Wisnivesky, JP. (Mar 2008). "Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer.". Cancer 112 (6): 1239-46. doi:10.1002/cncr.23309. PMID 18224663.
- ↑ Peyre, CG.; Hagen, JA.; DeMeester, SR.; Altorki, NK.; Ancona, E.; Griffin, SM.; Hölscher, A.; Lerut, T. et al. (Oct 2008). "The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection.". Ann Surg 248 (4): 549-56. doi:10.1097/SLA.0b013e318188c474. PMID 18936567.