Difference between revisions of "Microglandular hyperplasia of the uterine cervix"
(→Images) |
|||
| Line 61: | Line 61: | ||
===Images=== | ===Images=== | ||
<gallery> | |||
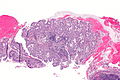
Image: Microglandular hyperplasia -- low mag.jpg | MGH - low mag. | |||
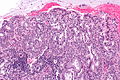
Image: Microglandular hyperplasia -- intermed mag.jpg | MGH - intermed. mag. | |||
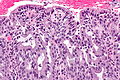
Image: Microglandular hyperplasia -- high mag.jpg | MGH - high mag. | |||
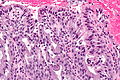
Image: Microglandular hyperplasia - alt 1 -- high mag.jpg | MGH - high mag. | |||
Image: Microglandular hyperplasia - alt 2 -- high mag.jpg | MGH - high mag. | |||
</gallery> | |||
www: | www: | ||
*[http://www.nature.com/modpathol/journal/v13/n3/fig_tab/3880047f14.html#figure-title MGH (nature.com)]. | *[http://www.nature.com/modpathol/journal/v13/n3/fig_tab/3880047f14.html#figure-title MGH (nature.com)]. | ||
Revision as of 00:16, 4 February 2014
| Microglandular hyperplasia of the uterine cervix | |
|---|---|
| Diagnosis in short | |
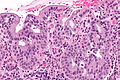
 Microglandular hyperplasia. H&E stain. | |
|
| |
| LM | crowded small glands (classic), reticular or solid, cytologically benign - usually cuboidal morphology, typically clear cytoplasm |
| LM DDx | adenocarcinoma in situ of the uterine cervix, endometrial mucinous microglandular adenocarcinoma, clear cell carcinoma of the uterine cervix |
| Site | uterine cervix |
|
| |
| Associated Dx | OCP use |
| Prevalence | common |
| Prognosis | benign |
Microglandular hyperplasia of the uterine cervix is a relatively common benign finding the uterine cervix that may be confused with malignancy, especially endocervical adenocarcinoma. It is usually referred to simply as microglandular hyperplasia, abbreviated MGH, and is also known as microglandular change.
It should not to be confused with microglandular adenosis.
General
Gross
Features:
Images:
Microscopic
Features:[1]
- Cytologically benign - important.
- Usually cuboidal morphology.
- Typically clear cytoplasm.
- Crowded small glands (classic), reticular or solid.
Significant negatives:
- Nuclear atypia absent.
- NC ratio not significantly increased.
DDx:
- Adenocarcinoma in situ of the uterine cervix.
- Endometrial mucinous microglandular adenocarcinoma - very rare.[4][5]
- Clear cell carcinoma of the uterine cervix.[6]
Images
www:
IHC
Features:[8]
- Ki-67 ~ 0.5% cells.
- Vimentin -ve.
- PR +ve ~ 60% of cases.
- ER +ve/-ve.
Others:[8]
- p53 -ve.
- CEA -ve.
- p16 -ve (scattered cells +ve).[citation needed]
Sign out
UTERINE ENDOCERVIX, CURETTAGE: - MICROGLANDULAR HYPERPLASIA. - SQUAMOUS EPITHELIUM WITH REACTIVE CHANGES AND METAPLASTIC CHANGES.
Micro
The sections show gland forming epithelium without nuclear atypia (no nuclear membrane irregularities, no coarse chromatin). The nuclei are less than 2x the size of a neutrophil, regularly spaced, pale staining and have small regular nucleoli visible with the 20x objective. No mitotic activity is apparent.
Fragments of reactive squamous epithelium with metaplastic changes are present. Benign superficial squamous epithelium is identified.
See also
References
- ↑ 1.0 1.1 Zaino, RJ. (Mar 2000). "Glandular lesions of the uterine cervix.". Mod Pathol 13 (3): 261-74. doi:10.1038/modpathol.3880047. PMID 10757337.
- ↑ 2.0 2.1 Jobo, T.; Kuramoto, H.; Morisawa, T. (May 1981). "[Microglandular hyperplasia of the cervix: reevaluation of the polyp (author's transl)].". Acta Obstet Gynaecol Jpn 33 (5): 651-8. PMID 7234352.
- ↑ 3.0 3.1 URL: http://www.cervicalhealth.com/colposcopy.php. Accessed on: 18 December 2013.
- ↑ Giordano, G.; D'Adda, T.; Gnetti, L.; Merisio, C.; Melpignano, M. (Jan 2006). "Endometrial mucinous microglandular adenocarcinoma: morphologic, immunohistochemical features, and emphasis in the human papillomavirus status.". Int J Gynecol Pathol 25 (1): 77-82. PMID 16306789.
- ↑ Zamecnik, M.; Skalova, A.; Opatrny, V. (Jun 2003). "Microglandular adenocarcinoma of the uterus mimicking microglandular cervical hyperplasia.". Ann Diagn Pathol 7 (3): 180-6. PMID 12808571.
- ↑ Offman, SL.; Longacre, TA. (Sep 2012). "Clear cell carcinoma of the female genital tract (not everything is as clear as it seems).". Adv Anat Pathol 19 (5): 296-312. doi:10.1097/PAP.0b013e31826663b1. PMID 22885379.
- ↑ URL: http://sunnybrook.ca/content/?page=Dept_LabS_APath_GynPath_ImgAt_Cvx_neo_micro. Accessed on: 25 February 2012.
- ↑ 8.0 8.1 Qiu, W.; Mittal, K. (Jul 2003). "Comparison of morphologic and immunohistochemical features of cervical microglandular hyperplasia with low-grade mucinous adenocarcinoma of the endometrium.". Int J Gynecol Pathol 22 (3): 261-5. doi:10.1097/01.PGP.0000071043.12278.8D. PMID 12819393.