Difference between revisions of "Colorectal adenocarcinoma"
(tweak) |
|||
| Line 168: | Line 168: | ||
*No standardized criteria for tumour deposits.<ref name=pmid24112678>{{Cite journal | last1 = Ueno | first1 = H. | last2 = Hashiguchi | first2 = Y. | last3 = Shimazaki | first3 = H. | last4 = Shinto | first4 = E. | last5 = Kajiwara | first5 = Y. | last6 = Nakanishi | first6 = K. | last7 = Kato | first7 = K. | last8 = Maekawa | first8 = K. | last9 = Nakamura | first9 = T. | title = Peritumoral deposits as an adverse prognostic indicator of colorectal cancer. | journal = Am J Surg | volume = | issue = | pages = | month = Oct | year = 2013 | doi = 10.1016/j.amjsurg.2013.04.009 | PMID = 24112678 }}</ref> | *No standardized criteria for tumour deposits.<ref name=pmid24112678>{{Cite journal | last1 = Ueno | first1 = H. | last2 = Hashiguchi | first2 = Y. | last3 = Shimazaki | first3 = H. | last4 = Shinto | first4 = E. | last5 = Kajiwara | first5 = Y. | last6 = Nakanishi | first6 = K. | last7 = Kato | first7 = K. | last8 = Maekawa | first8 = K. | last9 = Nakamura | first9 = T. | title = Peritumoral deposits as an adverse prognostic indicator of colorectal cancer. | journal = Am J Surg | volume = | issue = | pages = | month = Oct | year = 2013 | doi = 10.1016/j.amjsurg.2013.04.009 | PMID = 24112678 }}</ref> | ||
=====Ueno criteria===== | |||
Ueno ''et al.'' propose that a tumour deposit is either:<ref name=pmid24112678/> | Ueno ''et al.'' propose that a tumour deposit is either:<ref name=pmid24112678/> | ||
#>=2 mm from the tumour front | #>=2 mm from the tumour front | ||
Revision as of 04:18, 7 December 2013
| Colorectal adenocarcinoma | |
|---|---|
| Diagnosis in short | |
| LM DDx | other adenocarcinomas |
| IHC | CK20 +ve, CDX2 +ve, CK7 -ve, beta-catenin (nuclear) +ve |
| Site | rectum, colon, cecum, appendix |
|
| |
| Syndromes | familial adenomatous polyposis, Lynch syndrome |
|
| |
| Signs | +/-blood in stools, +/-abdominal mass, +/-rectal mass, +/-signs of bowel obstruction (nausea, vomiting) |
| Symptoms | constipation |
| Prevalence | common |
| Blood work | +/-anemia (microcytic) |
| Radiology | +/-"apple core" lesion (classic), +/-findings of bowel obstruction (air-fluid levels esp. with transition point) |
| Endoscopy | +/-suspicious mass (exophytic or ulcerated) |
| Prognosis | good to poor |
Colorectal adenocarcinoma is very common and a leading cause of death due to cancer. This article deals with colorectal adenocarcinoma not otherwise specified.
Colorectal carcinoma, abbreviated CRC, is typically considered a synonym.
The colon and rectum are lumped together was the mucosa in the large bowel is very similar. Thus, colonic adenocarcinoma and rectal adenocarcinoma redirect to this article.
General
- Very common.
- Rectum and sigmoid > proximal large bowel.
Presentation:
- Bright red blood per rectum (BRBPR).
- Constipation.
- Symptoms of bowel obstruction - nausea, vomiting.
Pathogenesis - see pathogenesis of colorectal carcinoma.
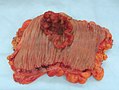
Gross
Often circumferential or near circumferential:
- These are referred to as "apple core lesion" or "napkin-ring" lesion.
Mucosa:
- Granular appearance.
- Raised (exophytic) or heaped edges with ulceration.
Note:
- Total mesorectal excisions should be assessed for completeness.
- The (soft tissue) radial margins, as present in TMEs and right hemicolectomies, should be inked.[1][2]
Images
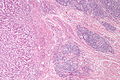
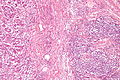
Microscopic
Features:
- Nuclear atypia:
- Nuclear pseudostratification.
- Nuclear hyperchromasia.
- Chromatin clearing or granularity.
- +/-Necrosis.
- Architecture - important for grading:
- Glands.
- Sheets.
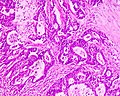
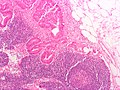
Images
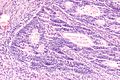
Mucinous adenocarcinoma - very low mag. (WC/Nephron)
CRC lymph node metastasis. (WC/Nephron)
www:
Grading
Based on component composed of glands:
- >=50% of tumour = low-grade (well-differentiated and moderately differentiated).
- <50% of tumour = high-grade (poorly-differentiated and undifferentiated).
Peritumour lymphocytic response
General
- Finding associated with improved survival in CRC.[5]
Microscopic
Onlinepathology advocates use of the Ueno criteria. They have a better inter-rater reproducibility than the older Graham criteria[6] and are less complicated.
Ueno criteria (2013)
Required criteria:[7]
- Non-MALT lymphoid aggregates (peritumoural) >= 1 mm.
Ignore:
- Muscosa-associated lymphoid tissue (MALT) = mucosal lymphoid aggregates, submucosal lymphoid aggregates adjacent to the musuclaris mucosae.
- Lymph nodes - these have a (fibrous) capsule.
- Irregular shape (not round).
Graham criteria (1990)
Required criteria:[6]
- Peritumoral:
- Lymphoid aggregates with germinal centres focally.
- Stellate fibrosis.
- No previous clinical and pathologic evidence of Crohn's disease.
Note:
- Should not be confused with intratumoural lymphocytic response.
- The intratumoural lymphocytic response is associated with MSI-H cancers.
Images
www:
- Peritumour lymphocytic response in endometrial carcinoma (bmjjournals.com).
- Peritumour lymphocytic response in CRC (ascpjournals.org).[8]
Intratumoural lymphocytic response
- AKA tumour-infiltrating lymphocytes, abbreviated TILs.
General
- Finding is suggestive of microsatellite instabillity.[9]
- May be seen in the context of Lynch syndrome.
Microscopic
Features:
- Lymphocytes are between the tumour cells.[10] †
- Other lymphocytes do not count.
Note:
- † Definitions vary substantially - some authors consider lymphocytes adjacent to the tumour (in the stroma around the tumour cells) "intratumoural".[11]
Images
www:
Tumour deposits
General
- Poor prognosticator.
- Can be understood as a type of invasive front/border, e.g. well-circumscribed border versus infiltrative border.[12]
- No standardized criteria for tumour deposits.[12]
Ueno criteria
Ueno et al. propose that a tumour deposit is either:[12]
- >=2 mm from the tumour front
- >=2 mm (radially) from the deepest aspect of the muscularis propria, if the tumour is not present in the section.
Tumour regression
There is a three tiered regression grading system by Ryan et al. for colorectal cancer that has essentially been adopted by CAP:[13]
| Grade | Features |
|---|---|
| Grade 1 | small groups of tumour cells or single tumour cells |
| Grade 2 | definite tumour but more fibrosis ("cancer outgrown by fibrosis") |
| Grade 3 | definite tumour with no fibrosis or tumour with a lesser amount of fibrosis ("fibrosis outgrown by cancer") |
IHC
- CK7 -ve.
- CK20 +ve.
- CEA +ve.
- CDX2 +ve.
Molecular
- KRAS mutation analysis.
- BRAF mutation analysis.
- V600E missense mutation found in ~10% CRC.[15]
Note:
- KRAS mutations and BRAF mutations are considered mutually exclusive as they occur in the same pathway.
Sign out
Right hemicolectomy
TERMINAL ILEUM, CECUM, ASCENDING COLON AND APPENDIX, RIGHT HEMICOLECTOMY: - INVASIVE ADENOCARCINOMA WITH A MUCINOUS COMPONENT, LOW-GRADE, pT1, pN0. -- MARGINS NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. -- PLEASE SEE TUMOUR SUMMARY. - SMALL BOWEL WALL WITHIN NORMAL LIMITS. - APPENDIX WITHOUT SIGNIFICANT PATHOLOGY. - FOURTEEN LYMPH NODES NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 14 ).
See also
References
- ↑ URL: http://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=13954. Accessed on: 6 February 2013.
- ↑ Bateman, AC.; Carr, NJ.; Warren, BF. (Apr 2005). "The retroperitoneal surface in distal caecal and proximal ascending colon carcinoma: the Cinderella surgical margin?". J Clin Pathol 58 (4): 426-8. doi:10.1136/jcp.2004.019802. PMID 15790712.
- ↑ Ogino, S.; Nosho, K.; Irahara, N.; Meyerhardt, JA.; Baba, Y.; Shima, K.; Glickman, JN.; Ferrone, CR. et al. (Oct 2009). "Lymphocytic reaction to colorectal cancer is associated with longer survival, independent of lymph node count, microsatellite instability, and CpG island methylator phenotype.". Clin Cancer Res 15 (20): 6412-20. doi:10.1158/1078-0432.CCR-09-1438. PMID 19825961.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/Colon_12protocol_3200.pdf. Accessed on: 14 September 2012.
- ↑ Harrison, JC.; Dean, PJ.; el-Zeky, F.; Vander Zwaag, R. (Jan 1995). "Impact of the Crohn's-like lymphoid reaction on staging of right-sided colon cancer: results of multivariate analysis.". Hum Pathol 26 (1): 31-8. PMID 7821914.
- ↑ 6.0 6.1 Graham, DM.; Appelman, HD. (May 1990). "Crohn's-like lymphoid reaction and colorectal carcinoma: a potential histologic prognosticator.". Mod Pathol 3 (3): 332-5. PMID 2362940.
- ↑ Ueno, H.; Hashiguchi, Y.; Shimazaki, H.; Shinto, E.; Kajiwara, Y.; Nakanishi, K.; Kato, K.; Maekawa, K. et al. (Apr 2013). "Objective Criteria for Crohn-like Lymphoid Reaction in Colorectal Cancer.". Am J Clin Pathol 139 (4): 434-41. doi:10.1309/AJCPWHUEFTGBWKE4. PMID 23525613.
- ↑ 8.0 8.1 Ross, JS.; Torres-Mora, J.; Wagle, N.; Jennings, TA.; Jones, DM. (Sep 2010). "Biomarker-based prediction of response to therapy for colorectal cancer: current perspective.". Am J Clin Pathol 134 (3): 478-90. doi:10.1309/AJCP2Y8KTDPOAORH. PMID 20716806.
- ↑ Iacopetta, B.; Grieu, F.; Amanuel, B. (Dec 2010). "Microsatellite instability in colorectal cancer.". Asia Pac J Clin Oncol 6 (4): 260-9. doi:10.1111/j.1743-7563.2010.01335.x. PMID 21114775.
- ↑ 10.0 10.1 Garg, K.; Soslow, RA. (Aug 2009). "Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma.". J Clin Pathol 62 (8): 679-84. doi:10.1136/jcp.2009.064949. PMID 19638537.
- ↑ Ropponen, KM.; Eskelinen, MJ.; Lipponen, PK.; Alhava, E.; Kosma, VM. (Jul 1997). "Prognostic value of tumour-infiltrating lymphocytes (TILs) in colorectal cancer.". J Pathol 182 (3): 318-24. doi:10.1002/(SICI)1096-9896(199707)182:3318::AID-PATH8623.0.CO;2-6. PMID 9349235.
- ↑ 12.0 12.1 12.2 Ueno, H.; Hashiguchi, Y.; Shimazaki, H.; Shinto, E.; Kajiwara, Y.; Nakanishi, K.; Kato, K.; Maekawa, K. et al. (Oct 2013). "Peritumoral deposits as an adverse prognostic indicator of colorectal cancer.". Am J Surg. doi:10.1016/j.amjsurg.2013.04.009. PMID 24112678.
- ↑ Ryan, R.; Gibbons, D.; Hyland, JM.; Treanor, D.; White, A.; Mulcahy, HE.; O'Donoghue, DP.; Moriarty, M. et al. (Aug 2005). "Pathological response following long-course neoadjuvant chemoradiotherapy for locally advanced rectal cancer.". Histopathology 47 (2): 141-6. doi:10.1111/j.1365-2559.2005.02176.x. PMID 16045774.
- ↑ Monzon, FA.; Ogino, S.; Hammond, ME.; Halling, KC.; Bloom, KJ.; Nikiforova, MN. (Oct 2009). "The role of KRAS mutation testing in the management of patients with metastatic colorectal cancer.". Arch Pathol Lab Med 133 (10): 1600-6. doi:10.1043/1543-2165-133.10.1600. PMID 19792050.
- ↑ Tie J, Gibbs P, Lipton L, et al. (July 2010). "Optimizing targeted therapeutic development: Analysis of a colorectal cancer patient population with the BRAF(V600E) mutation". Int J Cancer. doi:10.1002/ijc.25555. PMID 20635392.