Difference between revisions of "Pleomorphic adenoma"
Jump to navigation
Jump to search
(+so) |
|||
| Line 62: | Line 62: | ||
*Mesenchymal stroma not required for diagnosis -- if >5% ducts.<ref name=IW_10jan2011>Weinreb I. 10 January 2011.</ref> | *Mesenchymal stroma not required for diagnosis -- if >5% ducts.<ref name=IW_10jan2011>Weinreb I. 10 January 2011.</ref> | ||
**No chondroid stroma ''and'' <5% ductal cells = '''[[myoepithelioma]]'''. | **No chondroid stroma ''and'' <5% ductal cells = '''[[myoepithelioma]]'''. | ||
*Look for, i.e. rule-out, poorly differentiated carcinoma: ''carcinoma ex pleomorphic adenoma''. | *Look for, i.e. rule-out, poorly differentiated carcinoma: ''carcinoma ex pleomorphic adenoma''. | ||
| Line 91: | Line 90: | ||
</pre> | </pre> | ||
Note: | |||
*Complete excision is often elusive; stating "completely excised" on a surgical pathology report is unwise. | |||
==See also== | ==See also== | ||
*[[Salivary glands]]. | *[[Salivary glands]]. | ||
Revision as of 20:53, 22 November 2013
| Pleomorphic adenoma | |
|---|---|
| Diagnosis in short | |
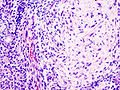
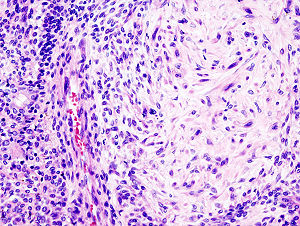 Pleomorphic adenoma. H&E stain. | |
|
| |
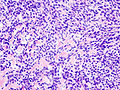
| LM | proliferation of myoepithelium in a mesenchymal stroma +/- epithelium; cells in ducts = epithelial, cells not in ducts = myoepithelial, mesenchymal stroma = chondroid stroma (specific), others (require epithelium) mucochondroid, hyalinized, osseous, fatty, myxoid |
| LM DDx | myoepithelioma, carcinoma ex pleomorphic adenoma, epithelial-myoepithelial carcinoma |
| IHC | S-100 +ve, SMA +ve, GFAP +ve |
| Site | salivary gland - usu. parotid gland, other sites |
|
| |
| Signs | mass lesion |
| Prevalence | common |
| Prognosis | benign |
| Clin. DDx | other salivary gland tumours |
Pleomorphic adenoma, abbreviated PA, is a very common benign salivary gland tumour.
General
Features:
- Very common - approx. 60% of parotid gland tumours.[1]
- May transform into a malignant tumour.
- Other benign salivary gland tumours do not do this.
- Only benign childhood salivary gland tumour of significance.
Weinreb's dictums
- Most common salivary tumour in all age groups.
- Seen in all sites (unlike other benign tumours).
- Recurrence and malignancy risk (unlike other benign salivary gland tumours).
- Any part of a tumour that looks like PA makes it a PA.
Gross
- May be cartilaginous appearing.
Image:
Microscopic
Features:[1]
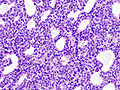
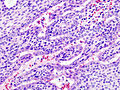
- Proliferation of myoepithelium and epithelium (ductal cells) in mesenchymal stroma.
- Cells in ducts = epithelial.
- Cells not in ducts = myoepithelial.[2]
- Mesenchymal stroma - important feature.
Notes:
- Mesenchymal stroma not required for diagnosis -- if >5% ducts.[2]
- No chondroid stroma and <5% ductal cells = myoepithelioma.
- Look for, i.e. rule-out, poorly differentiated carcinoma: carcinoma ex pleomorphic adenoma.
Memory device: MEC = myoepithelium, epithelium, chondromyxoid stroma.
DDx:
Images
www:
IHC
- S-100 +ve, SMA +ve, GFAP +ve.
Sign out
PAROTID GLAND MASS, RIGHT, EXCISION: - PLEOMORPHIC ADENOMA.
Note:
- Complete excision is often elusive; stating "completely excised" on a surgical pathology report is unwise.