Difference between revisions of "Mixed germ cell tumour"
Jump to navigation
Jump to search
(→General: tweak) |
(+ref) |
||
| Line 69: | Line 69: | ||
*[[Ovarian tumours]]. | *[[Ovarian tumours]]. | ||
==References== | ==References== | ||
{{Reflist|1}} | {{Reflist|1}} | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Germ cell tumours]] | [[Category:Germ cell tumours]] | ||
[[Category:Genitourinary pathology]] | [[Category:Genitourinary pathology]] | ||
[[Category:Gynecologic pathology]] | [[Category:Gynecologic pathology]] | ||
Revision as of 21:25, 20 July 2013
| Mixed germ cell tumour | |
|---|---|
| Diagnosis in short | |
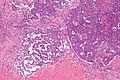
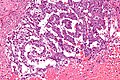
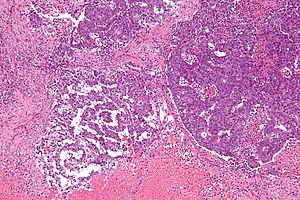 Mixed germ cell tumour. H&E stain. | |
|
| |
| LM | depends on the components |
| LM DDx | other germ cell tumours |
| IHC | variable |
| Site | ovary, testis, mediastinum, other |
|
| |
| Signs | mass lesion |
Mixed germ cell tumour, abbreviated MGCT, is a lesion composed of different germ cell tumours. Most germ cell tumours are mixed.
General
- 60% of GCTs are mixed. †
Common combinations:
- Teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- Seminoma + embryonal (SE).
- Teratoma + embryonal +(TE).
Memory device: TEE + all combinations have embryonal carcinoma.
Note:
- † Numbers vary between sources. One series suggests it is almost 70%.[1]
Microscopic
Features:
- Depends on components.
Notes:
- If one cannot identify the component... it is probably yolk sac as this has so many different patterns.
Images
www:
- Mixed germ cell tumour - several images (upmc.edu).
- Mixed germ cell tumour - several cases (upmc.edu).
IHC
- Beta-hCG +ve - if syncytiotrophoblasts are present.
- AFP +ve - a yolk sac tumour component is present.
- GFAP +ve - if neuroepithelium is present.
See also
References
- ↑ Mosharafa, AA.; Foster, RS.; Leibovich, BC.; Ulbright, TM.; Bihrle, R.; Einhorn, LH.; Donohue, JP. (Apr 2004). "Histology in mixed germ cell tumors. Is there a favorite pairing?". J Urol 171 (4): 1471-3. doi:10.1097/01.ju.0000116841.30826.85. PMID 15017200.