Urothelium
The urothelium lines the upper portion of the genitourinary tract, i.e. ureters, urinary bladder), and a bit of the lower part.
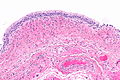
Normal urothelium
Gross
Extent of urothelium
- Ureters.
- Renal pelvis.
- Urinary bladder.
- Part of the urethra.
Urethra in males
- Pre-prostatic urethra - transitional epithelium.
- Prostatic urethra - transitional epithelium.
- Cancer arising at this site is prostatic urothelial carcinoma.
- Membranous urethra (from apex of prostate to bulb of penis (bulb of the corpus spongiosusm)) - pseudostratified columnar epithelium.
- Spongy urethra - pseudostratified columnar epithelium (proximal) & stratified squamous (distal).
Microscopic
Features:
- Maturation (cuboidal at base - squamoid at surface).
- Surface cells called 'umbrella cells' (umbrella cells CK20 +ve).
- Urothelium should be 4-5 cell layers thick.
- +/-Prominent nucleoli.
Note:
- Should not have a papillary architecture -- if it does it is likely cancer!
- If it is 'papillary' -- it must have fibrovascular cores.
IHC
- Rare superficial CK20 staining.
Image
Sign out
URINARY BLADDER LESION, TRANSURETHRAL RESECTION: - UROTHELIAL MUCOSA WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
Micro
The sections shows urothelium with underlying tissue. The urothelium is 4-5 cells thick. Umbrella cells are present. Few mononuclear inflammatory cells are seen in the subepithelial tissue.
The urothelium has no nuclear hyperchromasia and no significant nuclear enlargement. Mitotic activity is not identified. No papillary structures are present.
Approach
Where to start
July 1st PGY-2:
- Urothelial carcinoma - essentially defined by increased nuclear size +/- irreg. nuclear contour.
- Nucleoli are common in urothelium.
- This can be confusing... prostate carcinoma has nucleoli.
- Mitosis - these are key if the nuclear enlargement is not present.[1]
- Cell-depleted urothelium, where the cells have shed-off--but a few remain, should raise suspicions to cancer.
- Thickness of the urothelium, otherwise, isn't very useful for diagnosing cancer.
- Nucleoli are common in urothelium.
- Round structures should make you think of papillae and prompt looking for fibrovascular cores.
- Fibrovascular cores = papillae... may be cancer!
A checklist-like approach
- Papillary structure - with fibrovascular cores?
- Nuclear pleomorphism?
- Yes - high grade (4-5x lymphocyte) --> Dx: high grade papillary urothelial carcinoma
- No - low grade or normal (2-3x lymphocyte) --> DDx: low grade papillary urothelial carcinoma, PUNLMP, papilloma
- Nuclear pleomorphism?
- Flat lesions?
- Nuclear pleomorphism?
- Maturation to surface?
- No --> Dx: sectioning artefact vs. flat UCC.
- Yes --> likely benign.
- Normal thickness?
- Normal is 4-5 cell layers.
- Nests of glandular cells
- Consider cystitis cystica, cystitis glandularis, cystitis cystica et glandularis, von Brunn's nest, inverted papilloma.
- Inflammation?
- Michaelis-Gutman bodies?
Pitfalls:
- Urothelial carcinoma of the bladder may be confused with a paraganglioma of the bladder.
- Way to differentiate: paraganglioma = stippled chromatin, UCC = single nucleoli.
Note about terminology
- The bladder is rather unique in that "carcinoma" is a label used for things that are non-invasive.
- It has been suggested that many things that are called papillary urothelial carcinoma, would be better described as papillary intraurothelial neoplasia.[2]
- If the terminology in the urinary bladder were applied to the colon, we'd call all adenomas, i.e. pre-malignant lesions, carcinomas.
Overview in tables
General categorization
Urothelial lesions can broadly be divided into:
- Flat lesions.
- Lack papillae.
- Tend to be more aggressive.
- Papillary lesions.
- Must have true papillae.
- Very common.
- More often benign/indolent.
Flat urothelial lesions
Comparison urothelial changes - flat epithelium - benign/premalignant/cancerous:[3]
| Diagnosis | Nuclear enlargement (X stromal lymphocyte) |
Nucleoli | size var., shape | Polarity | Mitoses | Thickness | Inflammation | Other |
|---|---|---|---|---|---|---|---|---|
| Normal | none (2x) | small | none, round | matures to surface | none/minimal | 4-5 cells | none | - |
| Reactive atypia | moderate, prominent (3x) | prominent | none, round | as normal | some, none atypical | as normal | severe, acute or chronic | - |
| Flat urothelial hyperplasia | none (2x) | small | none, round | as normal | as normal | increased | usu. none | - |
| Urothelial dysplasia | moderate (3x) | small, some multiple | mod. variation, some irregularity | lost | rare, none atypical | as normal | usu. none | - |
| Urothelial carcinoma in situ | signif. (4-5x) | +/-large | marked, irregular | lost | common, atypical | thin, thick or norm. | +/- | - |
| Invasive UCC | signif. (4-5X) | +/-large | marked, irregular | lost | common, atypical | thin, thick or norm. | +/- | stromal invasion |
The bold entry is considered the key feature.
Papillary urothelial lesions
Urothelial cells in papillae - benign/premalignant/cancerous:[4][5]
| Diagnosis | Papillae features | Papillae branching | Papillae fusion | Nuclear size | Mitoses | DDx | IHC | Other | Key feature |
|---|---|---|---|---|---|---|---|---|---|
| Papilloma | fat papillae, thick FV core |
rare | none | normal (2x lymphocyte) | very rare basal | PUNLMP, low gr. PUCC | p53-, CK20+ umbrella cells | cytologically normal | normal cells, fat papillae |
| PUNLMP | slender FV core | uncommon | rare | enlarged - uniform | rare basal only | papilloma, low gr. | CK20+ umbrella | low cellular density (@ low power) vs. low gr.[6] | uniformly enlarged cell pop., slender papillae |
| Low grade PUCC | slender FV core, thick epithelium |
frequent | some | enlarged with variation | infreq., usually basal | PUNLMP, high gr. | -/+ p53, CK20+ umbrella | +/- small nucleoli | nuc. pleomorphism, thick epithelium |
| High grade PUCC | mixed population | common | common | 4-5x lymphocyte, marked pleomorphism |
common, everywhere | low gr., invasive UCC | diffuse CK20+, p53+ in 50% | nucleoli prominent | marked nuclear pleomorphism |
Notes:
- FV core = fibrovascular core.
- PUCC = papillary urothelial carcinoma.
Risk factors for urothelial carcinoma
Others:
- Lynch syndrome.
- Should be considered in ureteral cancers.[9]
Flat urothelial lesions
Overview
Several different benign & pre-malignant diagnoses can be made.
The World Health Organization classification is:[10]
- Reactive urothelial atypia.
- Flat urothelial hyperplasia.
- Urothelial atypia of unknown significance.
- Urothelial dysplasia (low-grade dysplasia).
- Urothelial carcinoma in situ (high-grade dysplasia).
- Invasive urothelial carcinoma.
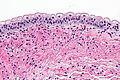
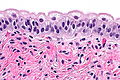
Mild urothelial atypia in normal urothelium
General
- May be confused with urothelial carcinoma in situ.[11]
- Uncommon.
- Considered to be normal urothelium.
Microscopic
Features:[11]
- Umbrella cells have:
- Mild nuclear enlargement ~3-4x lymphocyte.
- Round/regular nuclear membranes.
- +/-Multi-nucleation.
- Focally clear cytoplasm with cobwebs.
- Clear cytoplasm with eosinophilic reticulations.
- +/-Inflammation.
- No mitotic activity.
DDx:[12]
Images
IHC
- Ki-67 low.
- p53 -ve.
Sign out
URINARY BLADDER, TRANSURETHRAL BIOPSY: - UROTHELIAL MUCOSA WITH MILD CHRONIC INFLAMMATION. - NO EVIDENCE OF MALIGNANCY. COMMENT: Levels were cut and show large benign umbrella cells.
Micro
The sections show small fragments of urothelial mucosa with enlarged benign superficial epithelial cells. The lamina propria has a mild lymphocytic infiltrate. No papillary structures are identified. There is no significant nuclear atypia. Superficial small blood vessels appear congested.
Urothelial dysplasia
- AKA low-grade (urothelial) dysplasia.
Urothelial carcinoma in situ
- Abbreviated CIS.
- AKA high-grade (urothelial) dysplasia.
Urothelial cell carcinoma
- See urine cytology for the cytopathology.
- Abbreviated UCC.
- AKA urothelial carcinoma.
Papillary urothelial lesions
Papillary urothelial lesions are grouped into one of five categories (listed from good to bad prognosis):[5]
- Urothelial papilloma.
- Inverted papilloma.
- Papillary urothelial neoplasm of low malignant potential (PUNLMP).
- PUNLMP is pronouced "pun-lump".
- Low grade papillary urothelial carcinoma.
- High grade papillary urothelial carcinoma.
Key characteristics:
- Nuclear - size/pleomorphism.
- Papillae branching.
- Papillae fusion.
Urothelial papilloma
Inverted urothelial papilloma
Papillary urothelial neoplasm of low malignant potential
- Abbreviated PUNLMP.
- This is pronounced pun-lump.
Low-grade papillary urothelial carcinoma
High-grade papillary urothelial carcinoma
- Abbreviated HGPUC.
- AKA high-grade papillary urothelial cell carcinoma, abbreviated HGPUCC.
Papillary urothelial hyperplasia
Benign urothelial lesions
Cystitis
- Inflammation of the urinary bladder.
- Comes in many forms (see below).
- Typically a clinical diagnosis under the more general term urinary tract infection.
Note:
- So called "giant cell cystitis" is dealt with separately; it is a benign non-pathologic change that may or may not be associated with inflammation.[14]
The big table of cystitis
| Type | Key feature | DDx | Reference |
|---|---|---|---|
| Florid proliferative cystitis | expanded lamina propria with von Brunn's nests, cystitis cystica et glandularis | von Brunn's nests, cystitis cystica et glandularis, low-grade urothelial carcinoma | [15] |
| Polypoid cystitis | wide base, height > base | papillary cystitis, bullous cystitis | [16] |
| Bullous cystitis | wide base, height < base | papillary cystitis, polypoid cystitis | [16] |
| Papillary cystitis | narrow base, height > base | polypoid cystitis, bullous cystitis | [16] |
| Interstitial cystitis | +/-ulceration (uncommon) - requires clinical correlation | urothelial CIS | [17] |
| Follicular cystitis | lymphoid follicles | non-Hodgkin lymphoma | [18] |
| Infectious cystitis | dependent cause (bacterial, viral, fungal) | [19] | |
| Granulomatous cystitis | granulomas | tuberculosis, schistosomiasis, fungal infection, post-BCG | [19] |
| Radiation cystitis | edema, vascular congestion, +/- erosions -- acute; fibrosis in LP and detrusor -- chronic | [20] |
Interstitial cystitis
Follicular cystitis
Microscopic
Features:[18]
- Lymphoid follicles in the lamina propria.
DDx:
- Non-Hodgkin lymphoma.
Sign out
URINARY BLADDER, BIOPSY: - UROTHELIAL MUCOSA WITH CHRONIC INFLAMMATION AND BENIGN LYMPHOID NODULES WITH GERMINAL CENTRE FORMATION. - MUSCULARIS PROPRIA PRESENT. - NEGATIVE FOR UROTHELIAL CARCINOMA IN SITU AND NEGATIVE FOR MALIGNANCY.
Polypoid cystitis
General
- Uncommon.
- Wide age range.
- Benign.
Microscopic
Features:[16]
- Polypoid urothelium-covered projections with:
- Broad bases.
- Height > base.
- Extensive edema.
DDx:
- Papillary cystitis - not a broad base.
- Bullous cystitis.
Image:
von Brunn nests
General
- Benign.
Microscopic
Features:[21]
- Nests of (benign) urothelium budding into the lamina propria.
Note:
- Nests should not extend into the muscularis propria.
DDx:
- Nested urothelial cell carcinoma.[22]
- Inverted papilloma.
- Cystitis cystica - have lumens, may be focal.
IHC
Features:[22]
- p53 -ve.
- MIB-1 <3%.
Cystitis cystica
Cystitis glandularis
Malakoplakia
Nephrogenic adenoma
See also
References
- ↑ JS. 9 June 2010.
- ↑ Van der Kwast, TH.; Zlotta, AR.; Fleshner, N.; Jewett, M.; Lopez-Beltran, A.; Montironi, R. (Dec 2008). "Thirty-five years of noninvasive bladder carcinoma: a plea for the use of papillary intraurothelial neoplasia as new terminology.". Anal Quant Cytol Histol 30 (6): 309-15. PMID 19160695.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 155-163. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 166-175. ISBN 978-0443066771.
- ↑ 5.0 5.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 310. ISBN 978-0781765275.
- ↑ GAG. 26 February 2009.
- ↑ Chacko, JA.; Heiner, JG.; Siu, W.; Macy, M.; Terris, MK. (Jan 2006). "Association between marijuana use and transitional cell carcinoma.". Urology 67 (1): 100-4. doi:10.1016/j.urology.2005.07.005. PMID 16413342.
- ↑ URL: http://content.nejm.org/cgi/content/full/343/17/1268. Accessed on: 27 May 2010.
- ↑ Crockett, DG.; Wagner, DG.; Holmäng, S.; Johansson, SL.; Lynch, HT. (May 2011). "Upper urinary tract carcinoma in Lynch syndrome cases.". J Urol 185 (5): 1627-30. doi:10.1016/j.juro.2010.12.102. PMID 21419447.
- ↑ Hodges, KB.; Lopez-Beltran, A.; Davidson, DD.; Montironi, R.; Cheng, L. (Feb 2010). "Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features.". Hum Pathol 41 (2): 155-62. doi:10.1016/j.humpath.2009.07.002. PMID 19762067.
- ↑ 11.0 11.1 Amin, Mahul B. (2010). Diagnostic Pathology: Genitourinary (1st ed.). Amirsys. pp. 2-57. ISBN 978-1931884280.
- ↑ URL: http://pathology.jhu.edu/bladder/definitions.cfm. Accessed on: 8 January 2014.
- ↑ Watts, KE.; Montironi, R.; Mazzucchelli, R.; van der Kwast, T.; Osunkoya, AO.; Stephenson, AJ.; Hansel, DE. (Aug 2012). "Clinicopathologic characteristics of 23 cases of invasive low-grade papillary urothelial carcinoma.". Urology 80 (2): 361-6. doi:10.1016/j.urology.2012.04.010. PMID 22857755.
- ↑ Amin, Mahul B. (2010). Diagnostic Pathology: Genitourinary (1st ed.). Amirsys. pp. 2:6. ISBN 978-1931884280.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 113. ISBN 978-0443066771.
- ↑ 16.0 16.1 16.2 16.3 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 120. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 124. ISBN 978-0443066771.
- ↑ 18.0 18.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 122. ISBN 978-0443066771.
- ↑ 19.0 19.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 127. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 138. ISBN 978-0443066771.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1028. ISBN 0-7216-0187-1.
- ↑ 22.0 22.1 Volmar, KE.; Chan, TY.; De Marzo, AM.; Epstein, JI. (Sep 2003). "Florid von Brunn nests mimicking urothelial carcinoma: a morphologic and immunohistochemical comparison to the nested variant of urothelial carcinoma.". Am J Surg Pathol 27 (9): 1243-52. PMID 12960809.