Twin placentas
(Redirected from Twin placenta)
Jump to navigation
Jump to search
Twin placentas often come to the pathologist... even if they are normal. In these specimens, usually, the chorion is the key; the pathologist may be able to sort-out whether the twins are monozygotic (identical) or dizygotic (fraternal).
Monozygotic versus dizygotic twins
Monoamniotic-monochorionic gestation
- Abbreviated MoMo.
General
- Split at approximately 7th day.
- Always monozygotic twins.
- Very rare.
- High rate of complications - cords get into knots.
Gross
- No membrane between the fetuses - apparently clinically.
- Umbilical cord attachments usually very close to one another.[1]
Diamniotic-monochorionic gestation
- Abbreviated DiMo.
General
- The dogma is that the twins are always monozygotic.
- There is a case report of an exception.[2]
- Highest risk of TTTS (twin-to-twin transfusion syndrome).
Gross
Features - T-zone membrane is:[3]
- Thin.
- Translucent.
- No blood vessel remnants.
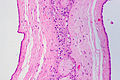
Microscopic
Features:[4]
- No chorion in the T-zone - key feature.
Images
Sign out
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION ABSENT (DIAMNIOTIC-MONOCHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Diamniotic-dichorionic gestation
- Abbreviated DiDi.
General
- Most dizygotic (70%), may be monozygotic (30%).
- If monozygotic -- split before 3 days.
Gross
Features - T-zone:[5]
- Thick.
- Less translucent.
- Blood vessels - fine branching.
Microscopic
Features:
- Chorion present in the T-zone.
Images
Sign out
Normal
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Early delivery
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, CESAREAN SECTION: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI AND ZONAL CONGESTION. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI.
Pathology seen only in twin pregnancies
Twin-to-twin transfusion syndrome
General
- Abbreviated as TTTS.
Definition:
- Monozygotic twins that share a placental disc, have vessels which cross-over between the twins that lead to a blood imbalance between the two twins.
- Only seen in monozygotic twins.
- Vascular connection may be vein-to-vein, artery-to-vein, artery-to-artery (uncommon).[6]
Prevalence:
- Seen in ~15% of monozygotic twins.[6]
Clinical:
- Donor:
- Twin: hypovolemic, oliguric, oligohydramnic, +/- anemia, +/-hypoglycemia, +/- small pale organs.
- Placental disc: large, pale.
- Recipient:
- Twin: hypervolemia, polyuria, polyhydramnios, +/- hydrops fetalis, +/- CHF, hemolytic janundice, +/- large congested organs.
- Placental disc: small, firm, congested.
Gross
- Large vessels that connect the two umbilical cords.
Image:
Microscopic
Features:[7]
- Artery-to-vein anatomosis - where artery and vein are associated with different umbilical cords.
- Donor twin side of placenta:
- Edematous villi.
- Increased nucleated RBCs.
- Recipient twin side of placenta:
- Congested.
See also
References
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 133. ISBN 978-1441974938.
- ↑ Redline, RW. (Jul 2003). "Nonidentical twins with a single placenta--disproving dogma in perinatal pathology.". N Engl J Med 349 (2): 111-4. doi:10.1056/NEJMp030097. PMID 12853583.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 128. ISBN 978-1441974938.
- ↑ URL: http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html. Accessed on: 30 October 2013.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 129. ISBN 978-1441974938.
- ↑ 6.0 6.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469. ISBN 978-0781765275.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469-70. ISBN 978-0781765275.