Diffuse alveolar damage
(Redirected from TRALI)
Jump to navigation
Jump to search
| Diffuse alveolar damage | |
|---|---|
| Diagnosis in short | |
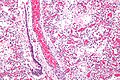
 Hyaline membranes. H&E stain. | |
|
| |
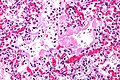
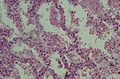
| LM | dependent on phase - exudative: hyaline membranes; proliferative: interstitial thickening, inflammation (lymphocytes), type 2 pneumocyte hyperplasia, edema, Masson bodies in the airway, hyaline material (usu. focal); fibrotic: interstitial inflammation, interstitial fibrosis |
| Subtypes | exudative, proliferative, fibrotic |
| LM DDx | organizing pneumonia (especially for proliferative phase DAD), bronchiolitis obliterans |
| Site | lung - see diffuse lung diseases |
|
| |
| Prognosis | often poor, dependent on severity and comorbidities |
| Other | histologic correlate of: acute respiratory distress syndrome (ARDS), acute interstitial pneumonia (AIP), transfusion related acute lung injury (TRALI); may be seen in chronic interstitial lung disease - esp. IPF |
| Treatment | dependent on underlying cause |
Diffuse alveolar damage, abbreviated DAD, is a relatively common lung pathology that is grouped with the diffuse lung diseases and has several clinical correlates.
General
Etiology:
- Abrupt hypoxemia with pulmonary infiltrates leading to epithelial cell and endothelial cell death not accompanied by cardiac failure.[1]
Classically, DAD is the histologic correlate of:
- Acute respiratory distress syndrome (ARDS).
- AKA adult respiratory distress syndrome (ARDS) to differentiate it from respiratory distress syndrome in infants.
- Acute interstitial pneumonia (AIP).
The DDx is broad:[2]
- Infection/sepsis.
- Toxic (smoke, oxygen).
- Drug (amiodarone, chemotherapy).
- Trauma/shock.
- Inflammatory.
- Idiopathic.
Notes:
- DAD may not be present in all cases that are clinically ARDS.[3]
- Transfusion related acute lung injury (TRALI) may have DAD; however, cases are reported without the pattern.[4]
- DAD may be seen in acute exacerbations of chronic interstitial lung disease, e.g. idiopathic pulmonary fibrosis.[5]
Microscopic
- Exudative:
- Hyaline membranes - key feature.
- Debris (pink crap) lines the alveolar spaces.
- Hyaline membranes - key feature.
- Proliferative:
- Interstitial thickening.
- Inflammation (lymphocytes).
- Hobnailing of alveolar lining cells (type 2 pneumocyte hyperplasia[8]).
- Edema (link pink crap in the alveoli).
- Masson bodies in the airway.
- Hyaline material (usu. focal) - key feature.
- Fibrotic:
- Interstitial inflammation.
- Fibrosis.
DDx:[7]
- Cryptogenic organizing pneumonia - especially for proliferative phase DAD.
- Bronchiolitis obliterans.
Images
www:
- Proliferative phase DAD - intermed. mag. (flickr.com/Yale Rosen).
- Proliferative phase DAD - high mag. (flickr.com/Yale Rosen).
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 364. ISBN 978-1416054542.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 91. ISBN 978-0781765275.
- ↑ Thille AW, Esteban A, Fernández-Segoviano P, Rodriguez JM, Aramburu JA, Peñuelas O, Cortés-Puch I, Cardinal-Fernández P, Lorente JA, Frutos-Vivar F (April 2013). "Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy". Am J Respir Crit Care Med 187 (7): 761–7. doi:10.1164/rccm.201211-1981OC. PMID 23370917.
- ↑ Danielson C, Benjamin RJ, Mangano MM, Mills CJ, Waxman DA (November 2008). "Pulmonary pathology of rapidly fatal transfusion-related acute lung injury reveals minimal evidence of diffuse alveolar damage or alveolar granulocyte infiltration". Transfusion 48 (11): 2401–8. doi:10.1111/j.1537-2995.2008.01879.x. PMID 18673344.
- ↑ Kaarteenaho R, Kinnula VL (2011). "Diffuse alveolar damage: a common phenomenon in progressive interstitial lung disorders". Pulm Med 2011: 531302. doi:10.1155/2011/531302. PMC 3099744. PMID 21637367. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099744/.
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 103. ISBN 978-1416002741.
- ↑ 7.0 7.1 Castro, CY. (2006). "ARDS and diffuse alveolar damage: a pathologist's perspective.". Semin Thorac Cardiovasc Surg 18 (1): 13-9. doi:10.1053/j.semtcvs.2006.02.001. PMID 16766248.
- ↑ URL: http://d3jonline.tripod.com/20-Pulmonary_II/Pathology_of_Interstitial_Lung_Diseases.htm. Accessed on: 22 February 2012.