Epilepsy
(Redirected from SUDEP)
Jump to navigation
Jump to search
Epilepsy is a common chronic seizure disorder.
General
- Epilepsy = seizures that are "idiopathic", i.e. no brain tumour, no mass lesion, no brain injury.
- Most common form: temporal lobe epilepsy.[1]
Etiology
- Many.
- Cortical dysplasia.
- Hamartia.
- Stroke.
- Infection.
- Head trauma.
Syndromic:
Tumour:
- Dysembryoplastic neuroepithelial tumour.[2]
- Ganglioglioma.[3]
- Isomorphic astrocytoma.
Types
Features:[4]
- Temporal lobe epilepsy
- Mesial temporal sclerosis = scarring of the medial temporal lobe.
- Involves: hippocampus, parahippocampal gyrus and amygdala.
- Granule cell dispersion
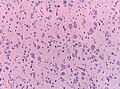
Hamartia
- Small collection of ectopic glioneuronal cells.
- Morpholology resembling oligodendroglial-like cells. [5]
- Mostly amygdala, less common in hippocampus or temporal lobe.
- Can coexist with focal cortical dysplasia.
Focal cortical dysplasia (FCD)
- Localized malformations of the cortex.
- Frequently associated with epilepsy in children.
- Includes cortical dyslamination, cytoarchitectural changes and white matter abnormalities.
- Current consensus: ILAE classification scheme 2011 [6](based on previous classification by Palmini 2004):
- Type I FCD (focal)
- Ia: Abnormal radial cortical lamination.
- Ib: Abnormal tangential cortical lamination.
- Ic: Abnormal radial and tangential cortical lamination.
- Type II FCD (focal)
- IIa: Presence of dysmorphic neurons.
- IIb: Presence of dysmorphic neurons and balloon cells.
- Type III FCD (associated with other lesion)
- IIIa: FCD associated with hippocampal sclerosis.
- IIIb: FCD adjacent to a brain tumor.
- IIIc: FCD adjacent to vascular malformation.
- IIIc: FCD associated with previous injury (trauma, inflammation...).
Hippocampal sclerosis
- Most frequent histopathology in temporal lobe epilepsy (33% of all epilepsy surgery specimen).
- ILAE classification for hippocampus specimen:[7]
- ILAE type 1: cell loss predominantly in CA1 and CA4 sectors.
- ILAE type 2: predominant CA1 neuron loss and gliosis.
- ILAE type 3: CA4 predominant neuronal cell loss and gliosis.
Clinic: ILAE type 1: benefit from epilepsy surgery.
Notes:
- Gliosis withot neuronal loss is not considered hippocampal sclerosis.
Granule cell dispersion
- Affects dentate gyrus.
- Observed in up to 40% specimen with hippocampal sclerosis.
- Clinico-pathological classification:[8]
- Granule cell pathology (GCP) Type 1: Substantial granule cell loss.
- Granule cell pathology (GCP) Type 2: Cell dispersion, ectopic neurons or clusters of neurons in the molecular layer or bi-lamination.
Clinic:
- Association with longer epilepsy duration.
DDx:
- Epilepsy.
- Dementia.
Mild Malformation of Cortical Development with Oligodendroglial Hyperplasia
- Abbreviated: MOGHE [9].
- Frontal lobe.
- Nonlesional (3.7% of epilepsy case).
- Increase cellularity of Olig2-, and PDGFR-alpha-immunoreactive oligodendroglia.
Sudden unexpected death in epilepsy
- Abbreviated SUDEP.
Diagnosis:
- Negative autopsy.
- History of epilepsy.
Epidemiology:[10]
- Typically poorly controlled epilepsy.
- Incidence: 0.09-9 per 1000 patient-years.
See also
References
- ↑ URL: http://emedicine.medscape.com/article/342150-overview. Accessed on: 20 November 2010.
- ↑ Cataltepe, O.; Turanli, G.; Yalnizoglu, D.; Topçu, M.; Akalan, N. (Apr 2005). "Surgical management of temporal lobe tumor-related epilepsy in children.". J Neurosurg 102 (3 Suppl): 280-7. doi:10.3171/ped.2005.102.3.0280. PMID 15881751.
- ↑ Im, SH.; Chung, CK.; Cho, BK.; Lee, SK. (Mar 2002). "Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome.". J Neurooncol 57 (1): 59-66. PMID 12125968.
- ↑ MUN. 15 November 2010.
- ↑ Kasper, BS.; Stefan, H.; Buchfelder, M.; Paulus, W. (Jan 1999). "Temporal lobe microdysgenesis in epilepsy versus control brains.". J Neuropathol Exp Neurol 58 (1): 22-8. PMID 10068310.
- ↑ Blümcke, I.; Aronica, E.; Miyata, H.; Sarnat, HB.; Thom, M.; Roessler, K.; Rydenhag, B.; Jehi, L. et al. (Mar 2016). "International recommendation for a comprehensive neuropathologic workup of epilepsy surgery brain tissue: A consensus Task Force report from the ILAE Commission on Diagnostic Methods.". Epilepsia 57 (3): 348-58. doi:10.1111/epi.13319. PMID 26839983.
- ↑ Blümcke, I.; Thom, M.; Aronica, E.; Armstrong, DD.; Bartolomei, F.; Bernasconi, A.; Bernasconi, N.; Bien, CG. et al. (Jul 2013). "International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a Task Force report from the ILAE Commission on Diagnostic Methods.". Epilepsia 54 (7): 1315-29. doi:10.1111/epi.12220. PMID 23692496.
- ↑ Blümcke, I.; Kistner, I.; Clusmann, H.; Schramm, J.; Becker, AJ.; Elger, CE.; Bien, CG.; Merschhemke, M. et al. (May 2009). "Towards a clinico-pathological classification of granule cell dispersion in human mesial temporal lobe epilepsies.". Acta Neuropathol 117 (5): 535-44. doi:10.1007/s00401-009-0512-5. PMID 19277686.
- ↑ Schurr, J.; Coras, R.; Rössler, K.; Pieper, T.; Kudernatsch, M.; Holthausen, H.; Winkler, P.; Woermann, F. et al. (01 2017). "Mild Malformation of Cortical Development with Oligodendroglial Hyperplasia in Frontal Lobe Epilepsy: A New Clinico-Pathological Entity.". Brain Pathol 27 (1): 26-35. doi:10.1111/bpa.12347. PMID 26748554.
- ↑ Tomson, T.; Nashef, L.; Ryvlin, P. (Nov 2008). "Sudden unexpected death in epilepsy: current knowledge and future directions.". Lancet Neurol 7 (11): 1021-31. doi:10.1016/S1474-4422(08)70202-3. PMID 18805738.