Necrotizing fasciitis
(Redirected from Fournier gangrene)
Jump to navigation
Jump to search
| Necrotizing fasciitis | |
|---|---|
| Diagnosis in short | |
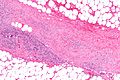
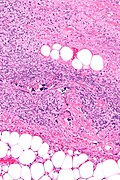
 Necrotizing fasciitis. H&E stain. | |
|
| |
| LM | necrotic fascia - amorphous grey or pink material and neutrophils |
| LM DDx | vasculitis |
| Gross | sloughing, bulae, erythema |
| Site | skin / subcutaneous tissue |
|
| |
| Clinical history | +/-trauma |
| Signs | subcutaneous emphysema, edema, skin sloughing, bulae, erythema, signs of sepsis |
| Symptoms | pain |
| Prevalence | uncommon |
| Prognosis | poor |
| Clin. DDx | cellulitis, abscess |
| Treatment | surgical debridement, antibiotics |
Necrotizing fasciitis, also known as flesh-eating disease, is an uncommon non-malignant skin disease with a high mortality.
It should not to be confused with nodular fasciitis.
In the perineum/genital region it is known as Fournier gangrene.[1]
General
Clinical:
- Pain - classically out-of-keep with appearance.
- Features of sepsis - late.
- Often nonspecific.[2]
Clinical DDx:
- Abscess.
- Cellulitis.
Epidemiology:
- Classically associated with Group A streptococcus.
- High mortality.[2]
- Usually adults, sometimes children.
Treatment:
- Operative debridement - emergency.[2]
- Broad spectrum antibiotics.
Note:
- May be diagnosed at frozen section.[3]
Gross
Features:[4]
- Subcutaneous emphysema.
- Edema.
- Erythema.
- Bulae.
- Skin sloughing.
Image
Microscopic
Features:
- Necrosis of fascia - key feature.[5]
- PMNs and necrotic debris (amorphous grey or pink material).
- +/-Vascular thrombosis.[6]
Note:
- Fat lobules between septae may be normal.
DDx:
Images
Sign out
Perianal Skin and Subcutaneous Tissue, Excision: - Consistent with clinical impression of necrotizing fasciitis.
Alternate
Submitted as "Tissue from Left Elbow", Excision:
- Skin and subcutaneous tissue with marked inflammation (see microscopic),
consistent with clinical impression of necrotizing fasciitis.
Comment:
The positive tissue cultures are noted.
Micro
Necrotic fascial tissue with inflamed adipose tissue and micro-abscess formation at dermis/subcutis interface. The overlying skin is moderately inflamed and edematous appearing.
See also
References
- ↑ Haemers, K.; Peters, R.; Braak, S.; Wesseling, F. (2013). "Necrotising fasciitis of the thigh.". BMJ Case Rep 2013. doi:10.1136/bcr-2013-009331. PMID 23771967.
- ↑ 2.0 2.1 2.2 Lancerotto, L.; Tocco, I.; Salmaso, R.; Vindigni, V.; Bassetto, F. (Mar 2012). "Necrotizing fasciitis: classification, diagnosis, and management.". J Trauma Acute Care Surg 72 (3): 560-6. doi:10.1097/TA.0b013e318232a6b3. PMID 22491537.
- ↑ Majeski, J.; Majeski, E. (Nov 1997). "Necrotizing fasciitis: improved survival with early recognition by tissue biopsy and aggressive surgical treatment.". South Med J 90 (11): 1065-8. PMID 9386043.
- ↑ Schuster, L.; Nuñez, DE. (Apr 2012). "Using clinical pathways to aid in the diagnosis of necrotizing soft tissue infections synthesis of evidence.". Worldviews Evid Based Nurs 9 (2): 88-99. doi:10.1111/j.1741-6787.2011.00235.x. PMID 22151905.
- ↑ Wong, CH.; Wang, YS. (Apr 2005). "The diagnosis of necrotizing fasciitis.". Curr Opin Infect Dis 18 (2): 101-6. PMID 15735411.
- ↑ Malghem, J.; Lecouvet, FE.; Omoumi, P.; Maldague, BE.; Vande Berg, BC. (Mar 2013). "Necrotizing fasciitis: contribution and limitations of diagnostic imaging.". Joint Bone Spine 80 (2): 146-54. doi:10.1016/j.jbspin.2012.08.009. PMID 23043899.