Urothelial dysplasia
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Urothelial dysplasia | |
|---|---|
| Diagnosis in short | |
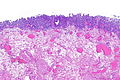
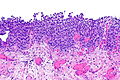
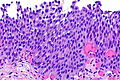
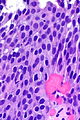
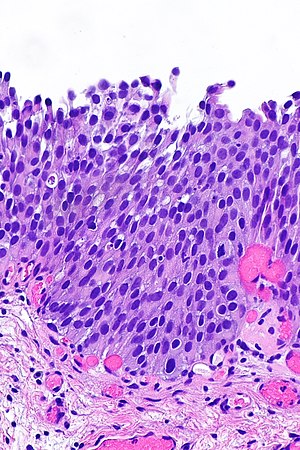 Urothelial dysplasia. H&E stain. | |
|
| |
| Synonyms | low-grade urothelial dysplasia |
|
| |
| LM | mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia, mild disorganization of the architecture (some maturation), occasional mitotic figures - none atypical |
| LM DDx | reactive changes, urothelial atypia of unknown significance, urothelial carcinoma in situ |
| IHC | CK20 +ve/-ve (esp. non-umbrella cells), Ki-67 +ve/-ve (>10%), p53 +ve/-ve (>20%) |
| Site | urothelium (renal pelvis, urinary bladder, ureters, urethra) |
|
| |
| Prevalence | common |
| Prognosis | pre-malignant |
Urothelial dysplasia, also low-grade (urothelial) dysplasia, is a lesion of the urothelium in the ISUP/WHO 2004 classification.[1]
It is precursor lesion to urothelial carcinoma that is less worrisome than urothelial carcinoma in situ (also known as high-grade (urothelial) dysplasia).
General
The ISUP/WHO classification of flat urothelial lesions is:[1]
- Reactive urothelial atypia.
- Flat urothelial hyperplasia.
- Urothelial atypia of unknown significance.
- Urothelial dysplasia (low-grade dysplasia).
- Urothelial carcinoma in situ (high-grade dysplasia).
- Invasive urothelial carcinoma.
Microscopic
Features:[2]
- Mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia.
- Slight disorganization of the architecture.
- Some maturation to the surface - important.
- Mitotic figures - occasional, none atypical.
Notes:
- It is probably not a good idea to make this diagnosis without immunohistochemistry.
- This diagnosis not made on frozen section.
DDx:
- Benign urothelium with reactive changes.
- Urothelial carcinoma in situ - no maturation to the surface or marked atypia - as in pagetoid UCIS and undermining UCIS.[3]
Images
www:
IHC
A comparison between benign, dysplasia and UCIS:[4]
| Diagnosis | CK20 | Ki-67 | p53 | p63 ‡ |
|---|---|---|---|---|
| Benign (reactive) | umbrella cells +ve only | -ve <=10% of cells (+/-rare basal cells) | -ve <20% of cells (+/-weak staining) | -ve surface cells |
| Urothelial dysplasia | +ve non-umbrella cells +ve (~30% of cases) | +ve >10% of cells (~40% of cases) | +ve >=20% of cells (~70% of cases) | -ve surface cells[5][6] |
| Urothelial carcinoma in situ (UCIS) | +ve non-umbrella cells (~70% of cases) | +ve >10% of cells (~95% of cases) | +ve >=20% of cells (~80% of cases) | +ve surface cells[5][6] |
Note:
- ‡ Morphology is considered the gold standard for UCIS versus urothelial dysplasia;[7] however, there is a small literature on p63 for dysplasia versus UCIS that is published in lesser known journals.
Sign out
Urinary Bladder, Biopsy:
- Urothelial dysplasia, see comment.
- Giant cell reaction and chronic inflammation.
Comment:
The urothelium has moderate CK20 staining that extends to the basement membrane. A p53 stain is negative (<10% staining). A Ki-67 stain shows increased staining (marks 20% of urothelium). A p63 stain shows weak/negative surface staining.
Block letters
RIGHT URETER (MARGIN), EXCISION:
- UROTHELIAL DYSPLASIA, SEE COMMENT.
- NEGATIVE FOR UROTHELIAL CARCINOMA.
COMMENT:
There is focal non-umbrella cell CK20 staining, 10% (focal) urothelial
p53 staining, and 30% (focal) urothelial Ki-67 staining. The findings
are that of (low-grade) urothelial dysplasia.
See also
References
- ↑ 1.0 1.1 Hodges, KB.; Lopez-Beltran, A.; Davidson, DD.; Montironi, R.; Cheng, L. (Feb 2010). "Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features.". Hum Pathol 41 (2): 155-62. doi:10.1016/j.humpath.2009.07.002. PMID 19762067.
- ↑ URL: http://pathology.jhu.edu/bladder/image1.cfm?case_number=10&image_number=1. Accessed on: 31 December 2013.
- ↑ McKenney, JK.; Gomez, JA.; Desai, S.; Lee, MW.; Amin, MB. (Mar 2001). "Morphologic expressions of urothelial carcinoma in situ: a detailed evaluation of its histologic patterns with emphasis on carcinoma in situ with microinvasion.". Am J Surg Pathol 25 (3): 356-62. PMID 11224606.
- ↑ Mallofré, C.; Castillo, M.; Morente, V.; Solé, M. (Mar 2003). "Immunohistochemical expression of CK20, p53, and Ki-67 as objective markers of urothelial dysplasia.". Mod Pathol 16 (3): 187-91. doi:10.1097/01.MP.0000056628.38714.5D. PMID 12640096.
- ↑ 5.0 5.1 Stepan, A.; Mărgăritescu, C.; Simionescu, C.; Ciurea, R. (2009). "E-cadherin and p63 immunoexpression in dysplastic lesions and urothelial carcinomas of the bladder.". Rom J Morphol Embryol 50 (3): 461-5. PMID 19690775.
- ↑ 6.0 6.1 Raheem, Sayad A.; Saied, Abdel N.; Al Shaer, Rabee; Mustafa, Osama; Ali, Ali H. (2014). "The Role of CK20, p53 and p63 in Differentiation of Some Urothelial Lesions of Urinary Bladder, Immunohistochemical Study". Open Journal of Pathology (4): 181-193. doi:10.4236/ojpathology.2014.44024.
- ↑ Amin MB, Trpkov K, Lopez-Beltran A, Grignon D (August 2014). "Best practices recommendations in the application of immunohistochemistry in the bladder lesions: report from the International Society of Urologic Pathology consensus conference". Am J Surg Pathol 38 (8): e20–34. doi:10.1097/PAS.0000000000000240. PMID 25029121.