Difference between revisions of "Urothelial carcinoma in situ"
Jump to navigation
Jump to search
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
| Caption = Urothelial carcinoma in situ. [[H&E stain]]. | | Caption = Urothelial carcinoma in situ. [[H&E stain]]. | ||
| Synonyms = high-grade dysplasia | | Synonyms = urothelial cell carcinoma in situ, high-grade dysplasia | ||
| Micro = nuclear changes (enlargement of nuclei (often 4-5x the size of stromal lymphocytes), nuclear pleomorphism - marked variation in size of nuclei), +/-disordered arrangement/crowding of cells, +/-mitoses, +/-enlarged nucleoli | | Micro = nuclear changes (enlargement of nuclei (often 4-5x the size of stromal lymphocytes), nuclear pleomorphism - marked variation in size of nuclei), +/-disordered arrangement/crowding of cells, +/-mitoses, +/-enlarged nucleoli | ||
| Subtypes = | | Subtypes = | ||
Revision as of 00:38, 19 March 2014
| Urothelial carcinoma in situ | |
|---|---|
| Diagnosis in short | |
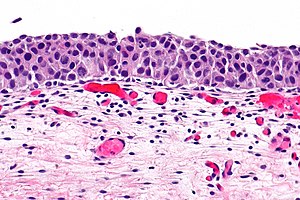 Urothelial carcinoma in situ. H&E stain. | |
|
| |
| Synonyms | urothelial cell carcinoma in situ, high-grade dysplasia |
|
| |
| LM | nuclear changes (enlargement of nuclei (often 4-5x the size of stromal lymphocytes), nuclear pleomorphism - marked variation in size of nuclei), +/-disordered arrangement/crowding of cells, +/-mitoses, +/-enlarged nucleoli |
| LM DDx | urothelial carcinoma, urothelial dysplasia, urothelial atypia of unknown significance |
| IHC | CK20 +ve (full thickness), Ki-67 high, p53 +ve, CD44 -ve, CK7 +ve |
| Site | urothelium - urinary bladder, ureter, renal pelvis, prostatic urethra |
|
| |
| Signs | +/-hematuria |
| Prevalence | relatively uncommon |
| Clin. DDx | invasive (flat) urothelial carcinoma |
Urothelial carcinoma in situ, also known as high-grade (urothelial) dysplasia, a non-invasive urothelial neoplasm without papillae.
It is also known as carcinoma in situ (abbreviated CIS) and urothelial cell carcinoma in situ (abbreviated UCC in situ). Urothelial carcinoma in situ may be abbreviated UCIS.
General
- Lack papillae.
- Uncommon in relation to other urothelial lesions.
- Less common than invasive flat urothelial carcinoma ~3-4x more common than UCIS.[1]
Classification of flat urothelial lesions
The World Health Organization classification is:[2]
- Reactive urothelial atypia.
- Flat urothelial hyperplasia.
- Urothelial atypia of unknown significance.
- Urothelial dysplasia (low-grade dysplasia).
- Urothelial carcinoma in situ (high-grade dysplasia).
- Invasive urothelial carcinoma.
Microscopic
Features:
- Nuclear changes key feature.
- Enlargement of nuclei (often 4-5x the size of stromal lymphocytes) -- diagnostic.[3]
- Normal urothelium approx. 2x the size of stromal lymphocytes.
- Nuclear pleomorphism - marked variation in size of nuclei.
- Enlargement of nuclei (often 4-5x the size of stromal lymphocytes) -- diagnostic.[3]
- +/-Disordered arrangement/crowding of cells.
- In normal urothelium the cell line-up on the basement membrane.
- Umbrella cells often absent.
- +/-Mitoses present.
- +/-Enlarged nucleoli.
Note:
- The urothelium may be "depleted", i.e. exist only of rare large cells on the basement membrane.
- This is known as clinging urothelial carcinoma in situ.[4]
DDx:
- Urothelial atypia of unknown significance - waffle diagnosis.
- Urothelial dysplasia.
- Urothelial carcinoma, invasive.
Images
www:
- Urothelial CIS (webpathology.com).
- Urothelial CIS with shedding (webpathology.com).
- Urothelial CIS - low mag. (webpathology.com).
- Urothelial CIS - high mag. (webpathology.com).
IHC
Features:[5]
- p53 +ve.
- Ki-67 high.
Benign urothelium vs. CIS:[6]
- CK20 +ve in deep cells (23/26 cases).
- Normal urothelium -- only the umbrella cells.
- Ki-67 ~50% of cells - deep and superficial.
- Normal ~10% of cells, confined to basal aspect.
- CD44 -ve.[7]
- Positive in indeterminant and negative.
Sign out
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR (TURBT):
- UROTHELIAL CARCINOMA IN SITU.
- BENIGN MUSCULARIS PROPRIA PRESENT.
URINARY BLADDER, RANDOM BIOPSIES: - UROTHELIAL CARCINOMA IN SITU, SEE COMMENT. -- NO EVIDENCE OF LAMINA PROPRIA INVASION. - CHRONIC INFLAMMATION, MILD. - BENIGN MUSCULARIS PROPRIA PRESENT. COMMENT: A CK20 immunostain marks the full thickness of the urothelium in atypical areas. A p53 immunostain moderately marks up to 20% of atypical cells focally. A Ki-67 immunostain marks 20-50% of the cells in the atypical areas.
Micro
The sections show multiple fragments of urothelium with nuclear hyperchromasia, nuclear crowding, mild-to-moderate nuclear enlargement, several atypical mitoses, and lack of maturation to the surface. There is no evidence of invasion. Benign muscularis propria is present.
See also
References
- ↑ Nielsen, ME.; Smith, AB.; Meyer, AM.; Kuo, TM.; Tyree, S.; Kim, WY.; Milowsky, MI.; Pruthi, RS. et al. (Jan 2014). "Trends in stage-specific incidence rates for urothelial carcinoma of the bladder in the United States: 1988 to 2006.". Cancer 120 (1): 86-95. doi:10.1002/cncr.28397. PMID 24122346.
- ↑ Hodges, KB.; Lopez-Beltran, A.; Davidson, DD.; Montironi, R.; Cheng, L. (Feb 2010). "Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features.". Hum Pathol 41 (2): 155-62. doi:10.1016/j.humpath.2009.07.002. PMID 19762067.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 161. ISBN 978-0443066771.
- ↑ Amin, Mahul B. (2010). Diagnostic Pathology: Genitourinary (1st ed.). Amirsys. pp. 2-55. ISBN 978-1931884280.
- ↑ Lopez-Beltran, A.; Jimenez, RE.; Montironi, R.; Patriarca, C.; Blanca, A.; Menendez, CL.; Algaba, F.; Cheng, L. (Nov 2011). "Flat urothelial carcinoma in situ of the bladder with glandular differentiation.". Hum Pathol 42 (11): 1653-9. doi:10.1016/j.humpath.2010.12.024. PMID 21531007.
- ↑ Yin, H.; He, Q.; Li, T.; Leong, AS. (Sep 2006). "Cytokeratin 20 and Ki-67 to distinguish carcinoma in situ from flat non-neoplastic urothelium.". Appl Immunohistochem Mol Morphol 14 (3): 260-5. PMID 16932015.
- ↑ Aron, M.; Luthringer, DJ.; McKenney, JK.; Hansel, DE.; Westfall, DE.; Parakh, R.; Mohanty, SK.; Balzer, B. et al. (Dec 2013). "Utility of a triple antibody cocktail intraurothelial neoplasm-3 (IUN-3-CK20/CD44s/p53) and α-methylacyl-CoA racemase (AMACR) in the distinction of urothelial carcinoma in situ (CIS) and reactive urothelial atypia.". Am J Surg Pathol 37 (12): 1815-23. doi:10.1097/PAS.0000000000000114. PMID 24225842.