Twin placentas
Revision as of 13:26, 23 January 2014 by Michael (talk | contribs) (→Twin-to-twin transfusion syndrome)
Twin placentas often come to the pathologist... even if they are normal. In these specimens, usually, the chorion is the key; the pathologist may be able to sort-out whether the twins are monozygotic (identical) or dizygotic (fraternal).
Monozygotic versus dizygotic twins
Monoamniotic-monochorionic gestation
- Abbreviated MoMo.
General
- Split at approximately 7th day.
- Always monozygotic twins.
- Very rare.
- High rate of complications - cords get into knots.
Gross
- No membrane between the fetuses - apparently clinically.
- Umbilical cord attachments usually very close to one another.[1]
Diamniotic-monochorionic gestation
- Abbreviated DiMo.
General
- The dogma is that the twins are always monozygotic.
- There is a case report of an exception.[2]
- Highest risk of TTTS (twin-to-twin transfusion syndrome).
Gross
Features - T-zone membrane is:[3]
- Thin.
- Translucent.
- No blood vessel remnants.
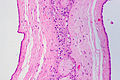
Microscopic
Features:[4]
- No chorion in the T-zone - key feature.
Images
Sign out
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION ABSENT (DIAMNIOTIC-MONOCHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Diamniotic-dichorionic gestation
- Abbreviated DiDi.
General
- Most dizygotic (70%), may be monozygotic (30%).
- If monozygotic -- split before 3 days.
Gross
Features - T-zone:[5]
- Thick.
- Less translucent.
- Blood vessels - fine branching.
Microscopic
Features:
- Chorion present in the T-zone.
Images
Sign out
Normal
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Early delivery
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, CESAREAN SECTION: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI AND ZONAL CONGESTION. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI.
Pathology seen only in twin pregnancies
Twin-to-twin transfusion syndrome
General
- Abbreviated as TTTS.
Definition:
- Monozygotic twins that share a placental disc, have vessels which cross-over between the twins that lead to a blood imbalance between the two twins.
- Only seen in monozygotic twins.
- Vascular connection may be vein-to-vein, artery-to-vein, artery-to-artery (uncommon).[6]
Prevalence:
- Seen in ~15% of monozygotic twins.[6]
Clinical:
- Donor:
- Twin: hypovolemic, oliguric, oligohydramnic, +/- anemia, +/-hypoglycemia, +/- small pale organs.
- Placental disc: large, pale.
- Recipient:
- Twin: hypervolemia, polyuria, polyhydramnios, +/- hydrops fetalis, +/- CHF, hemolytic janundice, +/- large congested organs.
- Placental disc: small, firm, congested.
Gross
- Large vessels that connect the two umbilical cords.
Image:
Microscopic
Features:[7]
- Artery-to-vein anatomosis - where artery and vein are associated with different umbilical cords.
- Donor twin side of placenta:
- Edematous villi.
- Increased nucleated RBCs.
- Recipient twin side of placenta:
- Congested.
See also
References
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 133. ISBN 978-1441974938.
- ↑ Redline, RW. (Jul 2003). "Nonidentical twins with a single placenta--disproving dogma in perinatal pathology.". N Engl J Med 349 (2): 111-4. doi:10.1056/NEJMp030097. PMID 12853583.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 128. ISBN 978-1441974938.
- ↑ URL: http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html. Accessed on: 30 October 2013.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 129. ISBN 978-1441974938.
- ↑ 6.0 6.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469. ISBN 978-0781765275.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469-70. ISBN 978-0781765275.