Difference between revisions of "Twin placentas"
Jump to navigation
Jump to search
m (→General) |
|||
| (28 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Twin [[placenta]]s''' often come to the pathologist... even if they are normal. In these specimens, usually, the chorion is the key; the pathologist may be able to sort-out whether the twins are monozygotic (identical) or dizygotic (fraternal). | '''Twin [[placenta]]s''' often come to the pathologist... even if they are normal. In these specimens, usually, the chorion is the key; the pathologist may be able to sort-out whether the twins are monozygotic (identical) or dizygotic (fraternal). | ||
=Monozygotic versus dizygotic twins= | |||
==Monoamniotic-monochorionic gestation== | |||
*Abbreviated ''MoMo''. | |||
===General=== | |||
*Split at approximately 7th day. | *Split at approximately 7th day. | ||
* | *Always monozygotic twins. | ||
*Very rare. | |||
*High rate of complications - cords get into knots. | |||
=== | ===Gross=== | ||
*No | *No membrane between the fetuses - apparently clinically. | ||
*Umbilical cord attachments usually very close to one another.<ref name=Ref_Placenta133>{{Ref Placenta|133}}</ref> | |||
=== | ==Diamniotic-monochorionic gestation== | ||
*Abbreviated ''DiMo''. | |||
===General=== | |||
*The dogma is that the twins are always monozygotic. | |||
**There is a case report of an exception.<ref name=pmid12853583>{{Cite journal | last1 = Redline | first1 = RW. | title = Nonidentical twins with a single placenta--disproving dogma in perinatal pathology. | journal = N Engl J Med | volume = 349 | issue = 2 | pages = 111-4 | month = Jul | year = 2003 | doi = 10.1056/NEJMp030097 | PMID = 12853583 }}</ref> | |||
*Highest risk of TTTS ([[twin-to-twin transfusion syndrome]]). | |||
===Gross=== | |||
Features - T-zone membrane is:<ref name=Ref_Placenta128>{{Ref Placenta|128}}</ref> | |||
*Thin. | |||
*Translucent. | |||
*No blood vessel remnants. | |||
===Microscopic=== | |||
Features:<ref>URL: [http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html]. Accessed on: 30 October 2013.</ref> | |||
*No chorion in the T-zone - '''key feature'''. | |||
====Images==== | |||
<gallery> | |||
Image:Monochorionic Diamniotic Twins, Intervening Membrane.jpg | Di-Mo placenta. (WC/euthman) | |||
</gallery> | |||
*[http://www.pathologypics.com/PictView.aspx?ID=1304 Diamniotic-monochorionic gestation (pathologypics.com)]. | |||
*[http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html Di-Mo placenta (utah.edu)]. | |||
===Sign out=== | |||
<pre> | |||
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: | |||
- FETAL MEMBRANES AT T-ZONE: | |||
-- CHORION ABSENT (DIAMNIOTIC-MONOCHORIONIC GESTATION). | |||
- TWIN A: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
- TWIN B: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
</pre> | |||
==Diamniotic-dichorionic gestation== | |||
*Abbreviated ''DiDi''. | |||
===General=== | |||
*Most dizygotic (70%), may be monozygotic (30%). | *Most dizygotic (70%), may be monozygotic (30%). | ||
*If monozygotic -- split before 3 days. | *If monozygotic -- split before 3 days. | ||
===Gross=== | |||
Features - T-zone:<ref name=Ref_Placenta129>{{Ref Placenta|129}}</ref> | |||
*Thick. | |||
*Less translucent. | |||
*Blood vessels - fine branching. | |||
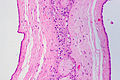
===Microscopic=== | |||
Features: | |||
*Chorion present in the T-zone. | |||
====Images==== | |||
<gallery> | |||
Image:Diamniotic-dichorionic_twin_placenta_-_low_mag.jpg | DiDi placenta. (WC) | |||
Image:Diamniotic dichorionic placenta, HE 1.jpg | DiDi placenta. (WC/euthman) | |||
Image:Diamniotic dichorionic placenta, HE 2.jpg | DiDi placenta. (WC/euthman) | |||
</gallery> | |||
*[http://library.med.utah.edu/WebPath/PLACHTML/PLAC005.html DiDi placenta (utah.edu)]. | |||
===Sign out=== | |||
====Normal==== | |||
<pre> | |||
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: | |||
- FETAL MEMBRANES AT T-ZONE: | |||
-- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). | |||
- TWIN A: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
- TWIN B: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
</pre> | |||
====Early delivery==== | |||
<pre> | |||
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, CESAREAN SECTION: | |||
- FETAL MEMBRANES AT T-ZONE: | |||
-- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). | |||
- TWIN A: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI AND | |||
ZONAL CONGESTION. | |||
- TWIN B: | |||
-- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
-- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
-- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI. | |||
</pre> | |||
=Pathology seen only in twin pregnancies= | |||
==Twin-to-twin transfusion syndrome== | ==Twin-to-twin transfusion syndrome== | ||
===General=== | ===General=== | ||
| Line 32: | Line 127: | ||
**Placental disc: large, pale. | **Placental disc: large, pale. | ||
*Recipient: | *Recipient: | ||
**Twin: hypervolemia, polyuria, polyhydramnios, +/- [[hydrops fetalis]], +/- CHF, hemolytic janundice, +/- large congested organs. | **Twin: hypervolemia, polyuria, [[polyhydramnios]], +/- [[hydrops fetalis]], +/- CHF, hemolytic janundice, +/- large congested organs. | ||
**Placental disc: small, firm, congested. | **Placental disc: small, firm, congested. | ||
===Gross=== | ===Gross=== | ||
*Large vessels that connect the two umbilical cords. | *Large vessels that connect the two umbilical cords. | ||
Image: | |||
<gallery> | |||
Image:De Wikkellkinderen.jpeg | Painting thought to depict TTTS. (WC) | |||
</gallery> | |||
===Microscopic=== | ===Microscopic=== | ||
Latest revision as of 13:26, 23 January 2014
Twin placentas often come to the pathologist... even if they are normal. In these specimens, usually, the chorion is the key; the pathologist may be able to sort-out whether the twins are monozygotic (identical) or dizygotic (fraternal).
Monozygotic versus dizygotic twins
Monoamniotic-monochorionic gestation
- Abbreviated MoMo.
General
- Split at approximately 7th day.
- Always monozygotic twins.
- Very rare.
- High rate of complications - cords get into knots.
Gross
- No membrane between the fetuses - apparently clinically.
- Umbilical cord attachments usually very close to one another.[1]
Diamniotic-monochorionic gestation
- Abbreviated DiMo.
General
- The dogma is that the twins are always monozygotic.
- There is a case report of an exception.[2]
- Highest risk of TTTS (twin-to-twin transfusion syndrome).
Gross
Features - T-zone membrane is:[3]
- Thin.
- Translucent.
- No blood vessel remnants.
Microscopic
Features:[4]
- No chorion in the T-zone - key feature.
Images
Sign out
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION ABSENT (DIAMNIOTIC-MONOCHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Diamniotic-dichorionic gestation
- Abbreviated DiDi.
General
- Most dizygotic (70%), may be monozygotic (30%).
- If monozygotic -- split before 3 days.
Gross
Features - T-zone:[5]
- Thick.
- Less translucent.
- Blood vessels - fine branching.
Microscopic
Features:
- Chorion present in the T-zone.
Images
Sign out
Normal
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Early delivery
TWIN PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, CESAREAN SECTION: - FETAL MEMBRANES AT T-ZONE: -- CHORION PRESENT (DIAMNIOTIC-DICHORIONIC GESTATION). - TWIN A: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI AND ZONAL CONGESTION. - TWIN B: -- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. -- FETAL MEMBRANES WITHIN NORMAL LIMITS. -- PLACENTAL DISC WITH FOCALLY MILDLY LARGE THIRD TRIMESTER VILLI.
Pathology seen only in twin pregnancies
Twin-to-twin transfusion syndrome
General
- Abbreviated as TTTS.
Definition:
- Monozygotic twins that share a placental disc, have vessels which cross-over between the twins that lead to a blood imbalance between the two twins.
- Only seen in monozygotic twins.
- Vascular connection may be vein-to-vein, artery-to-vein, artery-to-artery (uncommon).[6]
Prevalence:
- Seen in ~15% of monozygotic twins.[6]
Clinical:
- Donor:
- Twin: hypovolemic, oliguric, oligohydramnic, +/- anemia, +/-hypoglycemia, +/- small pale organs.
- Placental disc: large, pale.
- Recipient:
- Twin: hypervolemia, polyuria, polyhydramnios, +/- hydrops fetalis, +/- CHF, hemolytic janundice, +/- large congested organs.
- Placental disc: small, firm, congested.
Gross
- Large vessels that connect the two umbilical cords.
Image:
Microscopic
Features:[7]
- Artery-to-vein anatomosis - where artery and vein are associated with different umbilical cords.
- Donor twin side of placenta:
- Edematous villi.
- Increased nucleated RBCs.
- Recipient twin side of placenta:
- Congested.
See also
References
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 133. ISBN 978-1441974938.
- ↑ Redline, RW. (Jul 2003). "Nonidentical twins with a single placenta--disproving dogma in perinatal pathology.". N Engl J Med 349 (2): 111-4. doi:10.1056/NEJMp030097. PMID 12853583.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 128. ISBN 978-1441974938.
- ↑ URL: http://library.med.utah.edu/WebPath/PLACHTML/PLAC006.html. Accessed on: 30 October 2013.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 129. ISBN 978-1441974938.
- ↑ 6.0 6.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469. ISBN 978-0781765275.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 469-70. ISBN 978-0781765275.