Difference between revisions of "Spermatocytic tumour"
Jump to navigation
Jump to search
m (add image) |
|||
| Line 70: | Line 70: | ||
Image:Spermatocytic_seminoma_high_mag.jpg | Spermatocytic tumour - high mag. (WC) | Image:Spermatocytic_seminoma_high_mag.jpg | Spermatocytic tumour - high mag. (WC) | ||
Image:Spermatocytic_seminoma_intermed_mag.jpg | Spermatocytic tumour - intermed. mag. (WC) | Image:Spermatocytic_seminoma_intermed_mag.jpg | Spermatocytic tumour - intermed. mag. (WC) | ||
Image:testicular spermatocytic tumour high mag | Spermatocytic tumour - high mag. (WC) | |||
</gallery> | </gallery> | ||
Revision as of 16:18, 30 September 2018
| Spermatocytic tumour | |
|---|---|
| Diagnosis in short | |
 Spermatocytic tumour | |
|
| |
| Synonyms | spermatocytic seminoma (old term) |
|
| |
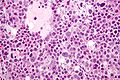
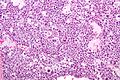
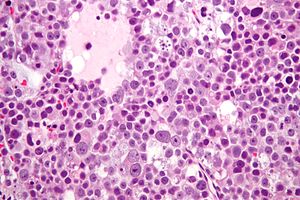
| LM | three cell populations: (1) small cells (6-8 µm) - with a large NC ratio, (2) medium cells (15-18 µm) with prominent nucleoli and spireme chromatin, (3) Large cells (50-100 µm) with spireme chromatin; mucoid lakes, intratubular spread |
| LM DDx | DLBCL, seminoma |
| Site | testis |
|
| |
| Signs | mass lesion |
| Prevalence | rare |
| Prognosis | benign, good |
| Clin. DDx | other germ cell tumours, lymphoma |
| Treatment | excision to exclude malignancy |
Spermatocytic tumour is a rare benign testicular tumour.
It was previously known as spermatocytic seminoma. It should not be confused with seminoma which is an unrelated tumour.
General
- Rare tumour.
- Only one case of metastases in 200 cases.[1]
- Orchiectomy is curative.
- Not reported/found in females.[1]
- Typically older - mean age 50s.[1]
Epidemiology
- Does not arise from germ cell neoplasia in situ (previously known as intratubular germ cell neoplasia)[2] - not considered a subtype of seminoma.
Microscopic
Features:[3]
- Population of three cells.
- Mucoid lakes.
- Intratubular spread.
Notes:
- Spireme = the tangle of filaments in prophase portion of mitosis.[4]
- May have eosinophilic cytoplasm (dependent on lab).
- Usually larger than Leydig cell tumour.
DDx:
Images
- Testicular spermatocytic tumour high mag
Spermatocytic tumour - high mag. (WC)
IHC
Features:[5]
- PLAP -ve (0 positive/17).
- CD117 -ve (7 positive/17).
- CAM5.2 -ve (1 positive/17).
See also
References
- ↑ 1.0 1.1 1.2 1.3 Eble JN (October 1994). "Spermatocytic seminoma". Hum. Pathol. 25 (10): 1035–42. PMID 7927308.
- ↑ Müller J, Skakkebaek NE, Parkinson MC (February 1987). "The spermatocytic seminoma: views on pathogenesis". Int. J. Androl. 10 (1): 147–56. doi:10.1111/j.1365-2605.1987.tb00176.x. PMID 3583416.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-0187-1.
- ↑ URL: http://www.thefreedictionary.com/spireme. Accessed on: 4 June 2010.
- ↑ Kraggerud, SM.; Berner, A.; Bryne, M.; Pettersen, EO.; Fossa, SD. (Mar 1999). "Spermatocytic seminoma as compared to classical seminoma: an immunohistochemical and DNA flow cytometric study.". APMIS 107 (3): 297-302. PMID 10223302.