Difference between revisions of "Sessile serrated adenoma"
m (rm space) |
|||
| Line 76: | Line 76: | ||
*Typically do not have nuclear atypia, i.e. no nuclear crowding, no nuclear hyperchromasia, no cigar-shaped nuclei. | *Typically do not have nuclear atypia, i.e. no nuclear crowding, no nuclear hyperchromasia, no cigar-shaped nuclei. | ||
**SSAs with nuclear atypia may be referred to as ''advanced sessile serrated adenomas''. | **SSAs with nuclear atypia may be referred to as ''advanced sessile serrated adenomas''. | ||
*Submucosal [[lipoma]]s seem to be associated with SSA in some way.{{fact}} | |||
===DDx=== | ===DDx=== | ||
Revision as of 11:41, 23 July 2013
| Sessile serrated adenoma | |
|---|---|
| Diagnosis in short | |
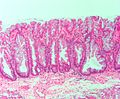
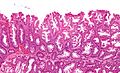
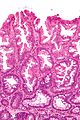
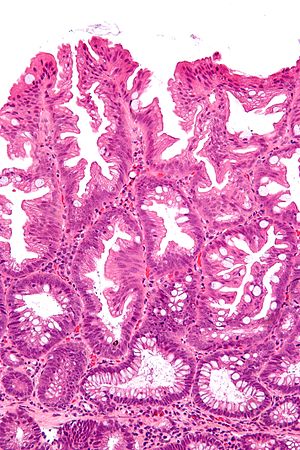 SSA. H&E stain. | |
|
| |
| LM | serrated epithelium, crypt base dilation, crypt branching, boot-shaped glands, horizontal glands |
| LM DDx | hyperplastic polyp, tubular adenoma (when with dysplasia) |
| Site | colon - usually cecum or ascending colon |
|
| |
| Associated Dx | colorectal adenocarcinoma, hyperplastic polyp |
| Syndromes | serrated polyposis syndrome, MUTYH polyposis syndrome |
|
| |
| Prevalence | common |
| Endoscopy | flat, usually > 5 mm, mucinous cap |
| Clin. DDx | normal, hyperplastic polyp |
Sessile serrated adenoma, abbreviated SSA, is a premalignant polyp of the large bowel.
It is also known as sessile serrated polyp (abbreviated SSP), sessile serrated lesion and sessile serrated adenoma/polyp (abbreviated SSA/P).
This lesion should not be confused with the traditional serrated adenoma, previously known as serrated adenoma.
General
- Colonic lesion.
- May be seen in the context of serrated polyposis syndrome.
Epidemiology:
- Thought to lead to colorectal cancer through a different pathway than most tumours in the left colon/rectum.
- Microvesicular hyperplastic polyps are hypothesized to be the the precursor of SSAs.[1]
Gross
Features:[2]
- Flat lesions, usually > 5 mm.
- Typically have a "mucous cap" - present ~65% of the time; useful for identification.
- Border not well-demarcated.
- More common in the proximal colon.
Note:
- Sessile lesions over 1 cm are usually SSAs.[2]
Image:
Microscopic
Features:
- Serrated epithelium at the surface and deep in the crypts.
- Saw-tooth appearance, epithelium has jagged appearing edge.
- Crypt dilation at base with serrations - key feature.
- Very common -- anecdotally the most sensitive feature.
- "Boot"-shape or "L"-shaped glands.
- Shape may be similar to a hockey stick.
- Horizontal crypts = crypt long axis parallel to the muscularis mucosae.
- Crypt branching.
Minimal extent criteria - number of abnormal crypts with the above features:
- German Society of Pathology proposal: at least two abnormal crypts -- crypts do not have to be adjacent.[4][5]
- Onlinepathology prefers this definition.
- An expert panel lead by Rex states that one unequivocally altered crypt should prompt calling SSA.[2]
- The WHO requires - depending on what you read:
Notes:
- Typically do not have nuclear atypia, i.e. no nuclear crowding, no nuclear hyperchromasia, no cigar-shaped nuclei.
- SSAs with nuclear atypia may be referred to as advanced sessile serrated adenomas.
- Submucosal lipomas seem to be associated with SSA in some way.[citation needed]
DDx
- Hyperplastic polyp.
- Tubular adenoma - for SSA with dysplasia, TAs often less than 1 cm (uncommon for SSAs).
Images
Sign out
COLONIC POLYP, ASCENDING COLON, BIOPSY: - SESSILE SERRATED ADENOMA. - NEGATIVE FOR DYSPLASIA.
COLONIC POLYP, ASCENDING COLON, BIOPSY: - SESSILE SERRATED ADENOMA WITH DYSPLASIA.
Note:
- The above exactly mirrors the Canadian consensus.[7]
Micro
The section shows a small polypoid fragment of colonic mucosa with a serrated epithelium that focally extends to the crypt base. Several dilated crypt bases are seen. One horizontal crypt and one boot-shaped crypt are present. The epithelium matures to the surface. A small amount of submucosa is present and contains a benign lymphoid aggregate.
References
- ↑ Huang, CS.; Farraye, FA.; Yang, S.; O'Brien, MJ. (Feb 2011). "The clinical significance of serrated polyps.". Am J Gastroenterol 106 (2): 229-40; quiz 241. doi:10.1038/ajg.2010.429. PMID 21045813.
- ↑ 2.0 2.1 2.2 Rex, DK.; Ahnen, DJ.; Baron, JA.; Batts, KP.; Burke, CA.; Burt, RW.; Goldblum, JR.; Guillem, JG. et al. (Sep 2012). "Serrated lesions of the colorectum: review and recommendations from an expert panel.". Am J Gastroenterol 107 (9): 1315-29; quiz 1314, 1330. doi:10.1038/ajg.2012.161. PMID 22710576.
- ↑ Rex DK, Hewett DG, Snover DC (December 2010). "Editorial: Detection targets for colonoscopy: from variable detection to validation". Am. J. Gastroenterol. 105 (12): 2665–9. doi:10.1038/ajg.2010.330. PMID 21131934.
- ↑ 4.0 4.1 Ensari, A.; Bilezikçi, B.; Carneiro, F.; Doğusoy, GB.; Driessen, A.; Dursun, A.; Flejou, JF.; Geboes, K. et al. (Nov 2012). "Serrated polyps of the colon: how reproducible is their classification?". Virchows Arch 461 (5): 495-504. doi:10.1007/s00428-012-1319-7. PMID 23052370.
- ↑ Aust, DE.; Baretton, GB. (Sep 2010). "Serrated polyps of the colon and rectum (hyperplastic polyps, sessile serrated adenomas, traditional serrated adenomas, and mixed polyps)-proposal for diagnostic criteria.". Virchows Arch 457 (3): 291-7. doi:10.1007/s00428-010-0945-1. PMID 20617338.
- ↑ URL: http://surgpathcriteria.stanford.edu/gitumors/sessile-serrated-polyp-adenoma/. Accessed on: 26 September 2012.
- ↑ Driman, DK.; Marcus, VA.; Hilsden, RJ; Owen, DA (2012). "Pathologic reporting of colorectal polyps: pan-Canadian consensus guidelines". Canadian Journal of Pathology 4 (3): 81-90.