Difference between revisions of "Pulmonary alveolar proteinosis"
Jump to navigation
Jump to search
m (→General) |
(→IHC) |
||
| Line 59: | Line 59: | ||
==IHC== | ==IHC== | ||
*Surfactant +ve.<ref name=pmid23821516>{{Cite journal | last1 = Albores | first1 = J. | last2 = Seki | first2 = A. | last3 = Fishbein | first3 = MC. | last4 = Abtin | first4 = F. | last5 = Lynch | first5 = JP. | last6 = Wang | first6 = T. | last7 = Weigt | first7 = SS. | title = A rare occurrence of pulmonary alveolar proteinosis after lung transplantation. | journal = Semin Respir Crit Care Med | volume = 34 | issue = 3 | pages = 431-8 | month = Jun | year = 2013 | doi = 10.1055/s-0033-1348472 | PMID = 23821516 }}</ref> | *Surfactant +ve.<ref name=pmid23821516>{{Cite journal | last1 = Albores | first1 = J. | last2 = Seki | first2 = A. | last3 = Fishbein | first3 = MC. | last4 = Abtin | first4 = F. | last5 = Lynch | first5 = JP. | last6 = Wang | first6 = T. | last7 = Weigt | first7 = SS. | title = A rare occurrence of pulmonary alveolar proteinosis after lung transplantation. | journal = Semin Respir Crit Care Med | volume = 34 | issue = 3 | pages = 431-8 | month = Jun | year = 2013 | doi = 10.1055/s-0033-1348472 | PMID = 23821516 }}</ref> | ||
==Sign out== | |||
<pre> | |||
LUNG, RIGHT UPPER LOBE (ABNORMAL AREA ON CT), WEDGE RESECTION: | |||
- PULMONARY ALVEOLAR PROTEINOSIS, SEE COMMENT. | |||
- NO SIGNIFICANT INTERSTITIAL FIBROSIS. | |||
- NO SIGNIFICANT INFLAMMATION. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
===Micro=== | |||
Sections show lung with eosinophilic material in the airspaces. Focally, small (~20 micrometres), more dense appearing, bodies are also in the airspace. The alveolar walls are within normal limits. No significant inflammation is identified. No microorganisms are seen with routine stains. There is no pulmonary hemorrhage. | |||
==See also== | ==See also== | ||
Revision as of 19:03, 26 February 2014
Pulmonary alveolar proteinosis, abbreviated PAP, in an uncommon medical lung disease.
General
- Associated with smoking - particularily in men.[1]
Pathophysiology:
- GM-CSF (granulocyte-macrophage colony stimulating factor) signaling in macrophages/lack of GM-CSF.
- GM-CSF is required by alveolar macrophages to clear surfactant.
Classification:[1]
- Congenital:
- Abnormal surfactant.
- GM-CSF receptor defect.
- Secondary:
- Infections.
- Haematologic malignancy.
- Acquired:
- Dusts - interfere with macrophage function.
Clinical:
Radiology
- CXR: airspace disease.
- HRCT: "crazy paving" - see: http://radiographics.rsnajnls.org/cgi/content/figsonly/23/6/1509.
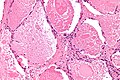
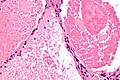
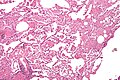
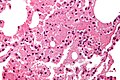
Microscopic
Features:
- Crap in the alveoli:
- "Dense bodies" - dead macrophages ("Chatter" in the alveoli).
- Edema - has pink stuff in the alveoli like PAP but no dense bodies.
DDx - may mimic:[4]
- Pulmonary edema.
- Pneumocystis pneumonia - exudates foamy & vacuolated.
- Pulmonary hemorrhage (acute). (???)
Images
www:
Images of DDx:
Stains
- PAS +ve -- material in airspace (surfactant).[6]
IHC
- Surfactant +ve.[7]
Sign out
LUNG, RIGHT UPPER LOBE (ABNORMAL AREA ON CT), WEDGE RESECTION: - PULMONARY ALVEOLAR PROTEINOSIS, SEE COMMENT. - NO SIGNIFICANT INTERSTITIAL FIBROSIS. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
Micro
Sections show lung with eosinophilic material in the airspaces. Focally, small (~20 micrometres), more dense appearing, bodies are also in the airspace. The alveolar walls are within normal limits. No significant inflammation is identified. No microorganisms are seen with routine stains. There is no pulmonary hemorrhage.
See also
References
- ↑ 1.0 1.1 Trapnell BC, Whitsett JA, Nakata K (December 2003). "Pulmonary alveolar proteinosis". N. Engl. J. Med. 349 (26): 2527-39. doi:10.1056/NEJMra023226. PMID 14695413. http://content.nejm.org/cgi/content/extract/349/26/2527.
- ↑ 2.0 2.1 Lin, FC.; Chang, GD.; Chern, MS.; Chen, YC.; Chang, SC. (Jun 2006). "Clinical significance of anti-GM-CSF antibodies in idiopathic pulmonary alveolar proteinosis.". Thorax 61 (6): 528-34. doi:10.1136/thx.2005.054171. PMID 16517574.
- ↑ Bhattacharyya, D.; Barthwal, MS.; Katoch, CD.; Rohatgi, MG.; Hasnain, S.; Rai, SP.; Arora, A. (Jan 2013). "Primary alveolar proteinosis - A report of two cases.". Med J Armed Forces India 69 (1): 90-3. doi:10.1016/j.mjafi.2012.02.016. PMID 24532945.
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 248. ISBN 978-0443066313.
- ↑ Leslie KO (May 2009). "My approach to interstitial lung disease using clinical, radiological and histopathological patterns". J. Clin. Pathol. 62 (5): 387–401. doi:10.1136/jcp.2008.059782. PMC 2668105. PMID 19398592. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2668105/.
- ↑ Ben-Dov, I.; Segel, MJ. (Jan 2014). "Autoimmune pulmonary alveolar proteinosis: Clinical course and diagnostic criteria.". Autoimmun Rev. doi:10.1016/j.autrev.2014.01.046. PMID 24424195.
- ↑ Albores, J.; Seki, A.; Fishbein, MC.; Abtin, F.; Lynch, JP.; Wang, T.; Weigt, SS. (Jun 2013). "A rare occurrence of pulmonary alveolar proteinosis after lung transplantation.". Semin Respir Crit Care Med 34 (3): 431-8. doi:10.1055/s-0033-1348472. PMID 23821516.