Difference between revisions of "Polypectomy scar"
Jump to navigation
Jump to search
(create) |
|||
| (8 intermediate revisions by the same user not shown) | |||
| Line 2: | Line 2: | ||
==General== | ==General== | ||
*Scar alone is difficult to differentiate from scar with cancer.<ref>{{cite journal | | *Scar alone is difficult to differentiate from scar with cancer.<ref>{{cite journal |authors=Riu Pons F, Andreu M, Gimeno Beltran J, Álvarez-Gonzalez MA, Seoane Urgorri A, Dedeu JM, Barranco Priego L, Bessa X |title=Narrow band imaging and white light endoscopy in the characterization of a polypectomy scar: A single-blind observational study |journal=World J. Gastroenterol. |volume=24 |issue=45 |pages=5179–5188 |date=December 2018 |pmid=30568394 |pmc=6288651 |doi=10.3748/wjg.v24.i45.5179 |url=}}</ref> | ||
*Iatrogenic tattoos are commonly seen in the context of polypectomy scars. Unfortunately, endoscopists are not good at documenting them; a study from 2021 found 67% of the time the location of the tattoo is not documented.<ref name=pmid33025255>{{cite journal |authors=Hershorn O, Park J, Singh H, Clouston K, Vergis A, Helewa RM |title=Predictors and rates of prior endoscopic tattoo localization amongst individuals undergoing elective colorectal resections for benign and malignant lesions |journal=Surg Endosc |volume=35 |issue=10 |pages=5524–5530 |date=October 2021 |pmid=33025255 |doi=10.1007/s00464-020-08048-8 |url=}}</ref> | |||
==Gross== | |||
*Flat white regions with loss of the usual mucosal folds. | |||
*Usually seen in association with an [[iatrogenic tattoo]]. | |||
Note: | |||
*The tattoo is most often distal to the scar.<ref name=pmid33025255/> | |||
==Microscopic== | ==Microscopic== | ||
| Line 10: | Line 19: | ||
DDx: | DDx: | ||
*Polypectomy scar with adenocarcinoma. | *Polypectomy scar with adenocarcinoma. | ||
*Focal fibrosis due to other cause. | |||
===Images=== | ===Images=== | ||
| Line 17: | Line 27: | ||
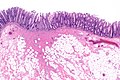
Image: Colorectal polypectomy scar -- low mag.jpg | CPR - low mag. (WC) | Image: Colorectal polypectomy scar -- low mag.jpg | CPR - low mag. (WC) | ||
</gallery> | </gallery> | ||
==Sign out== | |||
Should be signed in a non-committal way (e.g. "focal submucosal fibrosis") if no prior pathology is available/specimen is not labelled something like "old polypectomy site". | |||
The location of any intragenic tattoo(s) should be documented in relation to the suspected scar and correlated with clinical information (if available). | |||
<pre> | |||
Right Colon, Terminal Ileum and Appendix, Right Hemicolectomy: | |||
- Benign mucosal/submucosa scar compatible with the polypectomy site, correlation recommended, see comment. | |||
- Iatrogenic tattoo. | |||
- Terminal ileum within normal limits. | |||
- Appendix within normal limits. | |||
- Twenty benign lymph nodes (0 positive/20). | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
Comment: | |||
The scar was submitted in total. The location of the scar in relation to the tattoo is documented within the gross. | |||
It would be useful to confirm that: the location of lesion (that prompted the resection) in relation to the tattoo is the same as the relationship between scar and the tattoo. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Polypectomy]]. | *[[Polypectomy]]. | ||
*[[Iatrogenic tattoo]]. | |||
==References== | ==References== | ||
{{Reflist|1}} | {{Reflist|1}} | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Gastrointestinal pathology]] | [[Category:Gastrointestinal pathology]] | ||
Latest revision as of 22:08, 12 December 2023
A polypectomy scar results from a polypectomy.
General
- Scar alone is difficult to differentiate from scar with cancer.[1]
- Iatrogenic tattoos are commonly seen in the context of polypectomy scars. Unfortunately, endoscopists are not good at documenting them; a study from 2021 found 67% of the time the location of the tattoo is not documented.[2]
Gross
- Flat white regions with loss of the usual mucosal folds.
- Usually seen in association with an iatrogenic tattoo.
Note:
- The tattoo is most often distal to the scar.[2]
Microscopic
Features:
- Focal submucosal fibrosis.
DDx:
- Polypectomy scar with adenocarcinoma.
- Focal fibrosis due to other cause.
Images
Sign out
Should be signed in a non-committal way (e.g. "focal submucosal fibrosis") if no prior pathology is available/specimen is not labelled something like "old polypectomy site".
The location of any intragenic tattoo(s) should be documented in relation to the suspected scar and correlated with clinical information (if available).
Right Colon, Terminal Ileum and Appendix, Right Hemicolectomy: - Benign mucosal/submucosa scar compatible with the polypectomy site, correlation recommended, see comment. - Iatrogenic tattoo. - Terminal ileum within normal limits. - Appendix within normal limits. - Twenty benign lymph nodes (0 positive/20). - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: The scar was submitted in total. The location of the scar in relation to the tattoo is documented within the gross. It would be useful to confirm that: the location of lesion (that prompted the resection) in relation to the tattoo is the same as the relationship between scar and the tattoo.
See also
References
- ↑ Riu Pons F, Andreu M, Gimeno Beltran J, Álvarez-Gonzalez MA, Seoane Urgorri A, Dedeu JM, Barranco Priego L, Bessa X (December 2018). "Narrow band imaging and white light endoscopy in the characterization of a polypectomy scar: A single-blind observational study". World J. Gastroenterol. 24 (45): 5179–5188. doi:10.3748/wjg.v24.i45.5179. PMC 6288651. PMID 30568394. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6288651/.
- ↑ 2.0 2.1 Hershorn O, Park J, Singh H, Clouston K, Vergis A, Helewa RM (October 2021). "Predictors and rates of prior endoscopic tattoo localization amongst individuals undergoing elective colorectal resections for benign and malignant lesions". Surg Endosc 35 (10): 5524–5530. doi:10.1007/s00464-020-08048-8. PMID 33025255.