Difference between revisions of "Lynch syndrome"
Jump to navigation
Jump to search
| (19 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
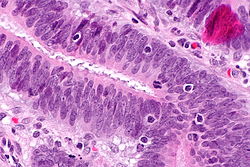
[[Image:Tumour-infiltrating lymphocytes - 2 -- very high mag.jpg|thumb|right|250px||[[Micrograph]] showing [[tumour infiltrating lymphocytes]], a finding seen in Lynch syndrome.]] | |||
'''Lynch syndrome''', also '''hereditary non-polyposis colorectal cancer syndrome''' (abbreviated '''HNPCC'''), is a constellation of clinical findings caused by a mutation in a mismatch repair gene, of which there are several.<ref name=OMIM120435>{{OMIM|120435}}</ref> | '''Lynch syndrome''', also '''hereditary non-polyposis colorectal cancer syndrome''' (abbreviated '''HNPCC'''), is a constellation of clinical findings caused by a mutation in a mismatch repair gene, of which there are several.<ref name=OMIM120435>{{OMIM|120435}}</ref> | ||
| Line 5: | Line 6: | ||
The term ''Lynch syndrome'' is preferred as individuals with this syndrome often present with non-colorectal cancers. | The term ''Lynch syndrome'' is preferred as individuals with this syndrome often present with non-colorectal cancers. | ||
==Clinical== | ==General== | ||
*Definitive diagnosis is by molecular testing (sequencing). | |||
*[[Immunohistochemical stains]] have a very strong concordance with molecular testing - see ''[[microsatellite instability]]''. | |||
===Clinical classification=== | |||
Divided into:<ref name=OMIM120435>{{OMIM|120435}}</ref> | Divided into:<ref name=OMIM120435>{{OMIM|120435}}</ref> | ||
*''Lynch syndrome I'' - colon cancer associated. | *''Lynch syndrome I'' - colon cancer associated. | ||
| Line 11: | Line 16: | ||
** More common in females (~50%) vs. males (~25%).<ref name=pmid19215248>{{Cite journal | last1 = Barrow | first1 = E. | last2 = Robinson | first2 = L. | last3 = Alduaij | first3 = W. | last4 = Shenton | first4 = A. | last5 = Clancy | first5 = T. | last6 = Lalloo | first6 = F. | last7 = Hill | first7 = J. | last8 = Evans | first8 = DG. | title = Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. | journal = Clin Genet | volume = 75 | issue = 2 | pages = 141-9 | month = Feb | year = 2009 | doi = 10.1111/j.1399-0004.2008.01125.x | PMID = 19215248 }}</ref> | ** More common in females (~50%) vs. males (~25%).<ref name=pmid19215248>{{Cite journal | last1 = Barrow | first1 = E. | last2 = Robinson | first2 = L. | last3 = Alduaij | first3 = W. | last4 = Shenton | first4 = A. | last5 = Clancy | first5 = T. | last6 = Lalloo | first6 = F. | last7 = Hill | first7 = J. | last8 = Evans | first8 = DG. | title = Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. | journal = Clin Genet | volume = 75 | issue = 2 | pages = 141-9 | month = Feb | year = 2009 | doi = 10.1111/j.1399-0004.2008.01125.x | PMID = 19215248 }}</ref> | ||
==Associations== | ===Genes=== | ||
*Colorectal carcinoma. | *MSH2 gene<ref name=OMIM120435>{{OMIM|120435}}</ref> - most common. | ||
*Non-endometrioid endometrial carcinoma | *MLH1 gene<ref name=OMIM120436>{{OMIM|120436}}</ref> - second most common. | ||
*Stomach carcinoma | *PMS2 gene.<ref name=OMIM600259>{{OMIM|600259}}</ref> | ||
*MSH6 gene<ref name=OMIM600678>{{OMIM|600678}}</ref> - tend to present in older individuals compared to individuals with MLH1 or MSH2 mutations.<ref name=pmid24056992>{{Cite journal | last1 = Stewart | first1 = A. | title = Genetic testing strategies in newly diagnosed endometrial cancer patients aimed at reducing morbidity or mortality from lynch syndrome in the index case or her relatives. | journal = PLoS Curr | volume = 5 | issue = | pages = | month = | year = 2013 | doi = 10.1371/currents.eogt.b59a6e84f27c536e50db4e46aa26309c | PMID = 24056992 }}</ref> | |||
*Others. | |||
===Associations=== | |||
*[[Colorectal carcinoma]]. | |||
*[[Endometrial carcinoma]]. | |||
**Morphologic features are not [[sensitivity|sensitive]] - IHC required. | |||
**Non-endometrioid [[endometrial carcinoma]],<ref name=pmid20396392>{{cite journal |author=Okuda T, Sekizawa A, Purwosunu Y, ''et al.'' |title=Genetics of endometrial cancers |journal=Obstet Gynecol Int |volume=2010 |issue= |pages=984013 |year=2010 |pmid=20396392 |pmc=2852605 |doi=10.1155/2010/984013 |url=}}</ref> e.g. [[endometrial clear cell carcinoma]].<ref name=pmid19638537>{{Cite journal | last1 = Garg | first1 = K. | last2 = Soslow | first2 = RA. | title = Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma. | journal = J Clin Pathol | volume = 62 | issue = 8 | pages = 679-84 | month = Aug | year = 2009 | doi = 10.1136/jcp.2009.064949 | PMID = 19638537 | url = http://jcp.bmj.com/content/62/8/679.long }}</ref> | |||
**[[Endometrioid endometrial carcinoma]].<ref name=pmid11873308>{{Cite journal | last1 = Lax | first1 = SF. | title = [Dualistic model of molecular pathogenesis in endometrial carcinoma]. | journal = Zentralbl Gynakol | volume = 124 | issue = 1 | pages = 10-6 | month = Jan | year = 2002 | doi = 10.1055/s-2002-20303 | PMID = 11873308 }}</ref> | |||
**Suggestive features: lower uterine segment, [[tumour infiltrating lymphocytes]].<ref name=pmid9638537>{{Cite journal | last1 = Garg | first1 = K. | last2 = Soslow | first2 = RA. | title = Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma. | journal = J Clin Pathol | volume = 62 | issue = 8 | pages = 679-84 | month = Aug | year = 2009 | doi = 10.1136/jcp.2009.064949 | PMID = 19638537 }}</ref> | |||
*[[Stomach carcinoma]],<ref name=OMIM120435>{{OMIM|120435}}</ref> intestinal-type.<ref name=pmid3581033>{{Cite journal | last1 = Cristofaro | first1 = G. | last2 = Lynch | first2 = HT. | last3 = Caruso | first3 = ML. | last4 = Attolini | first4 = A. | last5 = DiMatteo | first5 = G. | last6 = Giorgio | first6 = P. | last7 = Senatore | first7 = S. | last8 = Argentieri | first8 = A. | last9 = Sbano | first9 = E. | title = New phenotypic aspects in a family with Lynch syndrome II. | journal = Cancer | volume = 60 | issue = 1 | pages = 51-8 | month = Jul | year = 1987 | doi = | PMID = 3581033 }}</ref> | |||
**Significantly more common in males.<ref name=pmid19215248>{{Cite journal | last1 = Barrow | first1 = E. | last2 = Robinson | first2 = L. | last3 = Alduaij | first3 = W. | last4 = Shenton | first4 = A. | last5 = Clancy | first5 = T. | last6 = Lalloo | first6 = F. | last7 = Hill | first7 = J. | last8 = Evans | first8 = DG. | title = Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. | journal = Clin Genet | volume = 75 | issue = 2 | pages = 141-9 | month = Feb | year = 2009 | doi = 10.1111/j.1399-0004.2008.01125.x | PMID = 19215248 }}</ref> | **Significantly more common in males.<ref name=pmid19215248>{{Cite journal | last1 = Barrow | first1 = E. | last2 = Robinson | first2 = L. | last3 = Alduaij | first3 = W. | last4 = Shenton | first4 = A. | last5 = Clancy | first5 = T. | last6 = Lalloo | first6 = F. | last7 = Hill | first7 = J. | last8 = Evans | first8 = DG. | title = Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. | journal = Clin Genet | volume = 75 | issue = 2 | pages = 141-9 | month = Feb | year = 2009 | doi = 10.1111/j.1399-0004.2008.01125.x | PMID = 19215248 }}</ref> | ||
**Surveillance may not be worthwhile.<ref name=pmid12059060>{{Cite journal | last1 = Renkonen-Sinisalo | first1 = L. | last2 = Sipponen | first2 = P. | last3 = Aarnio | first3 = M. | last4 = Julkunen | first4 = R. | last5 = Aaltonen | first5 = LA. | last6 = Sarna | first6 = S. | last7 = Järvinen | first7 = HJ. | last8 = Mecklin | first8 = JP. | title = No support for endoscopic surveillance for gastric cancer in hereditary non-polyposis colorectal cancer. | journal = Scand J Gastroenterol | volume = 37 | issue = 5 | pages = 574-7 | month = May | year = 2002 | doi = | PMID = 12059060 }}</ref> | |||
*Biliary tree carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | *Biliary tree carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | ||
*Pancreatic carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | *Pancreatic carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | ||
*Urinary system carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | *Urinary system carcinoma.<ref name=OMIM120435>{{OMIM|120435}}</ref> | ||
**More common in the ureter than in sporadic cancers.<ref name=pmid21419447>{{Cite journal | last1 = Crockett | first1 = DG. | last2 = Wagner | first2 = DG. | last3 = Holmäng | first3 = S. | last4 = Johansson | first4 = SL. | last5 = Lynch | first5 = HT. | title = Upper urinary tract carcinoma in Lynch syndrome cases. | journal = J Urol | volume = 185 | issue = 5 | pages = 1627-30 | month = May | year = 2011 | doi = 10.1016/j.juro.2010.12.102 | PMID = 21419447 }}</ref> | **More common in the [[ureter]] than in sporadic cancers.<ref name=pmid21419447>{{Cite journal | last1 = Crockett | first1 = DG. | last2 = Wagner | first2 = DG. | last3 = Holmäng | first3 = S. | last4 = Johansson | first4 = SL. | last5 = Lynch | first5 = HT. | title = Upper urinary tract carcinoma in Lynch syndrome cases. | journal = J Urol | volume = 185 | issue = 5 | pages = 1627-30 | month = May | year = 2011 | doi = 10.1016/j.juro.2010.12.102 | PMID = 21419447 }}</ref> | ||
**Papillary lesions > flat lesions.<ref name=pmid12673555>{{Cite journal | last1 = Hartmann | first1 = A. | last2 = Dietmaier | first2 = W. | last3 = Hofstädter | first3 = F. | last4 = Burgart | first4 = LJ. | last5 = Cheville | first5 = JC. | last6 = Blaszyk | first6 = H. | title = Urothelial carcinoma of the upper urinary tract: inverted growth pattern is predictive of microsatellite instability. | journal = Hum Pathol | volume = 34 | issue = 3 | pages = 222-7 | month = Mar | year = 2003 | doi = 10.1053/hupa.2003.22 | PMID = 12673555 }}</ref> | |||
**Extensive inverted growth pattern suggestive of MSI.<ref name=pmid12673555/> | |||
**MSH2 mutations have an increased risk of urothelial carcinoma relative to MLH1 and MSH6 mutations.<ref name=pmid20591884>{{Cite journal | last1 = van der Post | first1 = RS. | last2 = Kiemeney | first2 = LA. | last3 = Ligtenberg | first3 = MJ. | last4 = Witjes | first4 = JA. | last5 = Hulsbergen-van de Kaa | first5 = CA. | last6 = Bodmer | first6 = D. | last7 = Schaap | first7 = L. | last8 = Kets | first8 = CM. | last9 = van Krieken | first9 = JH. | title = Risk of urothelial bladder cancer in Lynch syndrome is increased, in particular among MSH2 mutation carriers. | journal = J Med Genet | volume = 47 | issue = 7 | pages = 464-70 | month = Jul | year = 2010 | doi = 10.1136/jmg.2010.076992 | PMID = 20591884 }}</ref> | |||
Lame mnemonic ''GP CUBE'': | Lame mnemonic ''GP CUBE'': | ||
| Line 29: | Line 49: | ||
*'''E'''ndometrial. | *'''E'''ndometrial. | ||
== | Note: | ||
* | *All the cancers are below the diaphragm. | ||
* | ===Special types=== | ||
* | ====Muir-Torre syndrome==== | ||
*Abbreviated ''MTS''. | |||
*Muir-Torre syndrome is a subset of HNPCC that includes the presence of [[sebaceous adenoma]]s,<ref name=PBoD8_1177>{{Ref PBoD8|1177}}</ref> and [[sebaceous carcinoma]]s.<ref name=pmid2029018>{{Cite journal | last1 = Cohen | first1 = PR. | last2 = Kohn | first2 = SR. | last3 = Kurzrock | first3 = R. | title = Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. | journal = Am J Med | volume = 90 | issue = 5 | pages = 606-13 | month = May | year = 1991 | doi = | PMID = 2029018 }}</ref> | |||
**Cutaneous pathology precedes the internal malignancy in ~40% of cases.<ref name=pmid2029018/> | |||
Molecular pathology: | |||
*MTS is caused by mutations in MSH2 or MLH1.<ref name=omim158320>{{OMIM|158320}}</ref> | |||
== | ==IHC== | ||
:''See [[microsatellite instability]]''. | |||
==See also== | ==See also== | ||
Latest revision as of 20:49, 13 March 2016
Lynch syndrome, also hereditary non-polyposis colorectal cancer syndrome (abbreviated HNPCC), is a constellation of clinical findings caused by a mutation in a mismatch repair gene, of which there are several.[1]
As the name suggests, HNPCC is a form of inherited colorectal cancer that is not characterized by abundant intestinal polyps (non-polyposis), as in adenomatous polyposis coli.
The term Lynch syndrome is preferred as individuals with this syndrome often present with non-colorectal cancers.
General
- Definitive diagnosis is by molecular testing (sequencing).
- Immunohistochemical stains have a very strong concordance with molecular testing - see microsatellite instability.
Clinical classification
Divided into:[1]
- Lynch syndrome I - colon cancer associated.
- Lynch syndrome II - non-colon cancer associated.
- More common in females (~50%) vs. males (~25%).[2]
Genes
- MSH2 gene[1] - most common.
- MLH1 gene[3] - second most common.
- PMS2 gene.[4]
- MSH6 gene[5] - tend to present in older individuals compared to individuals with MLH1 or MSH2 mutations.[6]
- Others.
Associations
- Colorectal carcinoma.
- Endometrial carcinoma.
- Morphologic features are not sensitive - IHC required.
- Non-endometrioid endometrial carcinoma,[7] e.g. endometrial clear cell carcinoma.[8]
- Endometrioid endometrial carcinoma.[9]
- Suggestive features: lower uterine segment, tumour infiltrating lymphocytes.[10]
- Stomach carcinoma,[1] intestinal-type.[11]
- Biliary tree carcinoma.[1]
- Pancreatic carcinoma.[1]
- Urinary system carcinoma.[1]
Lame mnemonic GP CUBE:
- Gastric.
- Pancreas.
- CRC.
- UCC.
- Biliary.
- Endometrial.
Note:
- All the cancers are below the diaphragm.
Special types
Muir-Torre syndrome
- Abbreviated MTS.
- Muir-Torre syndrome is a subset of HNPCC that includes the presence of sebaceous adenomas,[16] and sebaceous carcinomas.[17]
- Cutaneous pathology precedes the internal malignancy in ~40% of cases.[17]
Molecular pathology:
- MTS is caused by mutations in MSH2 or MLH1.[18]
IHC
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Online 'Mendelian Inheritance in Man' (OMIM) 120435
- ↑ 2.0 2.1 Barrow, E.; Robinson, L.; Alduaij, W.; Shenton, A.; Clancy, T.; Lalloo, F.; Hill, J.; Evans, DG. (Feb 2009). "Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations.". Clin Genet 75 (2): 141-9. doi:10.1111/j.1399-0004.2008.01125.x. PMID 19215248.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 120436
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 600259
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 600678
- ↑ Stewart, A. (2013). "Genetic testing strategies in newly diagnosed endometrial cancer patients aimed at reducing morbidity or mortality from lynch syndrome in the index case or her relatives.". PLoS Curr 5. doi:10.1371/currents.eogt.b59a6e84f27c536e50db4e46aa26309c. PMID 24056992.
- ↑ Okuda T, Sekizawa A, Purwosunu Y, et al. (2010). "Genetics of endometrial cancers". Obstet Gynecol Int 2010: 984013. doi:10.1155/2010/984013. PMC 2852605. PMID 20396392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2852605/.
- ↑ Garg, K.; Soslow, RA. (Aug 2009). "Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma.". J Clin Pathol 62 (8): 679-84. doi:10.1136/jcp.2009.064949. PMID 19638537. http://jcp.bmj.com/content/62/8/679.long.
- ↑ Lax, SF. (Jan 2002). "[Dualistic model of molecular pathogenesis in endometrial carcinoma].". Zentralbl Gynakol 124 (1): 10-6. doi:10.1055/s-2002-20303. PMID 11873308.
- ↑ Garg, K.; Soslow, RA. (Aug 2009). "Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma.". J Clin Pathol 62 (8): 679-84. doi:10.1136/jcp.2009.064949. PMID 19638537.
- ↑ Cristofaro, G.; Lynch, HT.; Caruso, ML.; Attolini, A.; DiMatteo, G.; Giorgio, P.; Senatore, S.; Argentieri, A. et al. (Jul 1987). "New phenotypic aspects in a family with Lynch syndrome II.". Cancer 60 (1): 51-8. PMID 3581033.
- ↑ Renkonen-Sinisalo, L.; Sipponen, P.; Aarnio, M.; Julkunen, R.; Aaltonen, LA.; Sarna, S.; Järvinen, HJ.; Mecklin, JP. (May 2002). "No support for endoscopic surveillance for gastric cancer in hereditary non-polyposis colorectal cancer.". Scand J Gastroenterol 37 (5): 574-7. PMID 12059060.
- ↑ Crockett, DG.; Wagner, DG.; Holmäng, S.; Johansson, SL.; Lynch, HT. (May 2011). "Upper urinary tract carcinoma in Lynch syndrome cases.". J Urol 185 (5): 1627-30. doi:10.1016/j.juro.2010.12.102. PMID 21419447.
- ↑ 14.0 14.1 Hartmann, A.; Dietmaier, W.; Hofstädter, F.; Burgart, LJ.; Cheville, JC.; Blaszyk, H. (Mar 2003). "Urothelial carcinoma of the upper urinary tract: inverted growth pattern is predictive of microsatellite instability.". Hum Pathol 34 (3): 222-7. doi:10.1053/hupa.2003.22. PMID 12673555.
- ↑ van der Post, RS.; Kiemeney, LA.; Ligtenberg, MJ.; Witjes, JA.; Hulsbergen-van de Kaa, CA.; Bodmer, D.; Schaap, L.; Kets, CM. et al. (Jul 2010). "Risk of urothelial bladder cancer in Lynch syndrome is increased, in particular among MSH2 mutation carriers.". J Med Genet 47 (7): 464-70. doi:10.1136/jmg.2010.076992. PMID 20591884.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1177. ISBN 978-1416031215.
- ↑ 17.0 17.1 Cohen, PR.; Kohn, SR.; Kurzrock, R. (May 1991). "Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome.". Am J Med 90 (5): 606-13. PMID 2029018.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 158320