Difference between revisions of "Low-grade papillary urothelial carcinoma"
Jump to navigation
Jump to search
(→Image) |
|||
| Line 80: | Line 80: | ||
<gallery> | <gallery> | ||
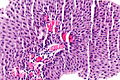
Image: Low-grade papillary urothelial carcinoma -- intermed mag.jpg | LGPUC - intermed. mag. | Image: Low-grade papillary urothelial carcinoma -- intermed mag.jpg | LGPUC - intermed. mag. | ||
Image: Low-grade papillary urothelial carcinoma -- high mag.jpg | LGPUC - | Image: Low-grade papillary urothelial carcinoma -- high mag.jpg | LGPUC - high mag. | ||
Image: Low-grade papillary urothelial carcinoma - alt -- high mag.jpg | LGPUC - | Image: Low-grade papillary urothelial carcinoma - alt -- high mag.jpg | LGPUC - high mag. | ||
</gallery> | </gallery> | ||
Revision as of 01:54, 4 June 2014
| Low-grade papillary urothelial carcinoma | |
|---|---|
| Diagnosis in short | |
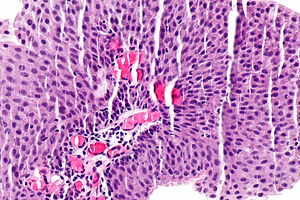 Low-grade papillary urothelial carcinoma. H&E stain. | |
|
| |
| LM | papillae (fibrovascular cores covered by urothelium) -- usually with fusion and branching, small nuclei (~3x a resting lymphocyte), +/-invasion into the lamina propria (rare), +/-mitoses (uncommon) |
| LM DDx | PUNLMP, urothelial papilloma, inverted papilloma, high-grade papillary urothelial carcinoma |
| IHC | Ki-67 low (<25% of cells) |
| Gross | exophytic lesion, frond-like appearance, friable |
| Site | urothelium |
|
| |
| Syndromes | Lynch syndrome |
|
| |
| Signs | hematuria |
| Prevalence | very common |
| Prognosis | very good |
| Clin. DDx | high-grade papillary urothelial carcinoma, urothelial papilloma |
Low-grade papillary urothelial carcinoma, abbreviated LGPUC,[1] is a very common indolent form of cancer that arises from the urothelium.
It is also known as low-grade papillary urothelial cell carcinoma, abbreviated LGPUCC.
General
- Very common.
- Very good prognosis - if it is non-invasive.
- Usually non-invasive.[2]
Note:
- Invasive low-grade UCC is:[2]
- ~75% nested variant of urothelial carcinoma.
- ~25: low-grade papillary urothelial carcinoma.
Gross
- Exophytic lesion.
- Frond-like appearance.
Microscopic
Features:[3]
- Papillae = fibrovascular cores covered by urothelium.
- Usually with fusion of papillae and branching of papillae.
- Small nuclei (~3x a resting lymphocyte).
- +/-Invasion into the lamina propria (rare).
- Rare mitoses.
- Usually difficult to find.
- Basal location.
Criteria for invasion (mnemonic PISS-R):[2]
- Stromal reaction.
- Infiltrating single cells.
- Small nests.
- Retraction artifact.
- Paradoxical differentiation.
Note:
- Nuclei slightly larger than in PUNLMPs.
- The presence/absence of muscle should be commented on in biopsy specimens.
- Adipose tissue may be seen in the lamina propria; tumour adjacent to adipose tissue on a biopsy does not imply invasion deep to the muscularis propria.[4]
DDx:
- PUNLMP.
- High grade papillary urothelial carcinoma.
- Often under-diagnosed (~15% in one series) when reassessed by experts.[5]
- The three most predictive features of high-grade are architectural complexity, nuclear size variation, and absence of umbrella cells.[6]
- Stanford criteria has a 5% rule -- if the high-grade component is <5% it is low-grade.[7]
- Inverted urothelial papilloma - often have peripheral palisading.
- Urothelial papilloma.
Image
IHC
- Ki-67:
Molecular
Molecular changes:[11]
- FGFR3
- HRAS
- Loss of heterozygosity - chromosome 9.
Note:
- Not currently used diagnostically.
Sign out
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION:
- LOW-GRADE PAPILLARY UROTHELIAL CARCINOMA.
-- NEGATIVE FOR LAMINA PROPRIA INVASION.
- NO MUSCULARIS PROPRIA IDENTIFIED.
Muscularis propria present
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION:
- LOW-GRADE PAPILLARY UROTHELIAL CARCINOMA.
-- NEGATIVE FOR LAMINA PROPRIA INVASION.
- BENIGN MUSCULARIS PROPRIA PRESENT.
Micro
The sections show urothelial mucosa with a tumour with fibrovascular cores. The nuclei are of uniform size (2-3 times a resting lymphocytes). Rare foci of degenerative cells are seen. The papillary structures are thick and appear to compress the lamina propria. Rare mitotic figures are identified. No atypical mitoses are apparent. No lamina propria invasion is identified. No muscularis propria is identified.
See also
References
- ↑ Watts, KE.; Montironi, R.; Mazzucchelli, R.; van der Kwast, T.; Osunkoya, AO.; Stephenson, AJ.; Hansel, DE. (Aug 2012). "Clinicopathologic characteristics of 23 cases of invasive low-grade papillary urothelial carcinoma.". Urology 80 (2): 361-6. doi:10.1016/j.urology.2012.04.010. PMID 22857755.
- ↑ 2.0 2.1 2.2 Toll, AD.; Epstein, JI. (Jul 2012). "Invasive low-grade papillary urothelial carcinoma: a clinicopathologic analysis of 41 cases.". Am J Surg Pathol 36 (7): 1081-6. doi:10.1097/PAS.0b013e318253d6e0. PMID 22510761.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 310. ISBN 978-0781765275.
- ↑ Bochner, BH.; Nichols, PW.; Skinner, DG. (Mar 1995). "Overstaging of transitional cell carcinoma: clinical significance of lamina propria fat within the urinary bladder.". Urology 45 (3): 528-31. doi:10.1016/S0090-4295(99)80030-2. PMID 7879346.
- ↑ Miyamoto, H.; Brimo, F.; Schultz, L.; Ye, H.; Miller, JS.; Fajardo, DA.; Lee, TK.; Epstein, JI. et al. (Aug 2010). "Low-grade papillary urothelial carcinoma of the urinary bladder: a clinicopathologic analysis of a post-World Health Organization/International Society of Urological Pathology classification cohort from a single academic center.". Arch Pathol Lab Med 134 (8): 1160-3. doi:10.1043/2009-0403-OA.1. PMID 20670136.
- ↑ Isfoss, BL.; Majak, B.; Busch, C.; Braathen, GJ. (Apr 2011). "Simplification of grading papillary urothelial neoplasia using a reduced set of diagnostic features.". Anal Quant Cytol Histol 33 (2): 68-74. PMID 21980608.
- ↑ URL: http://surgpathcriteria.stanford.edu/bladder/tcc-papillary-transitional-urothelial-carcinoma/. Accessed on: 27 January 2014.
- ↑ Rajcani, J.; Kajo, K.; Adamkov, M.; Moravekova, E.; Lauko, L.; Felcanova, D.; Bencat, M. (2013). "Immunohistochemical characterization of urothelial carcinoma.". Bratisl Lek Listy 114 (8): 431-8. PMID 23944616.
- ↑ Pich, A.; Chiusa, L.; Comino, A.; Navone, R. (1994). "Cell proliferation indices, morphometry and DNA flow cytometry provide objective criteria for distinguishing low and high grade bladder carcinomas.". Virchows Arch 424 (2): 143-8. PMID 7910097.
- ↑ Mai, KT.; Flood, TA.; Williams, P.; Kos, Z.; Belanger, EC. (Oct 2013). "Mixed low- and high-grade papillary urothelial carcinoma: histopathogenetic and clinical significance.". Virchows Arch 463 (4): 575-81. doi:10.1007/s00428-013-1456-7. PMID 23913166.
- ↑ Ehdaie, B.; Theodorescu, D. (Jan 2008). "Molecular markers in transitional cell carcinoma of the bladder: New insights into mechanisms and prognosis.". Indian J Urol 24 (1): 61-7. doi:10.4103/0970-1591.38606. PMC 2684226. PMID 19468362. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684226/.