Difference between revisions of "Low-grade oncocytic renal tumour"
Jump to navigation
Jump to search
(+L1CAM) |
|||
| (31 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
''' | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Low grade oncocytic renal tumour -- very high mag.jpg | |||
| Width = | |||
| Caption = Low-grade renal oncocytic tumour. [[H&E stain]]. | |||
| Micro = abundant eosinophilic cytoplasm, nuclei uniform and round without significant pleomorphism, solid or tubular architecture | |||
| Subtypes = | |||
| LMDDx = [[renal oncocytoma]], [[chromophobe renal cell carcinoma]] eosinophilic variant, [[clear cell renal cell carcinoma]] eosinophilic variant, [[papillary renal cell carcinoma]] oncocytic variant, [[tubulocystic carcinoma of the kidney]], other [[renal tumours with eosinophilic cytoplasm]], benign [[liver]] | |||
| Stains = | |||
| IHC = CK7 +ve, CD117 -ve, GATA3 +ve, [[PAX8]] +ve | |||
| EM = | |||
| Molecular = TSC/mTOR pathway mutation | |||
| IF = | |||
| Gross = | |||
| Grossing = [[partial nephrectomy grossing]], [[total nephrectomy for tumour grossing]] | |||
| Site = [[kidney]] - see [[kidney tumours]] | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = often incidentally discovered mass | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = likely benign | |||
| Other = | |||
| ClinDDx = other [[kidney tumours]] | |||
}} | |||
'''Low-grade oncocytic renal tumour''', abbreviated '''LOT''', is an unusual [[renal tumour]] that does not neatly fit into any WHO renal neoplasia category. It is also known as '''renal oncocytic tumour that is CD117 negative and CK7 positive'''. | |||
''Low-grade oncocytic tumour'' directs to here. | |||
Whether it is a distinct entity is not clear as of 2019.<ref name=pmid30895640/> It can be considered an emerging entity that may be in the WHO classification of renal neoplasia in the future.<ref name=pmid31936678>{{cite journal |authors=Siadat F, Trpkov K |title=ESC, ALK, HOT and LOT: Three Letter Acronyms of Emerging Renal Entities Knocking on the Door of the WHO Classification |journal=Cancers (Basel) |volume=12 |issue=1 |pages= |date=January 2020 |pmid=31936678 |pmc=7017067 |doi=10.3390/cancers12010168 |url=}}</ref> | |||
==General== | ==General== | ||
*Very rare. | *Very rare. | ||
*Benign behaviour based on a small series.<ref name=pmid30895640>{{cite journal |authors=Trpkov K, Williamson SR, Gao Y, Martinek P, Cheng L, Sangoi AR, Yilmaz A, Wang C, San Miguel Fraile P, Perez Montiel DM, Bulimbasić S, Rogala J, Hes O |title=Low-grade oncocytic tumour of kidney (CD117-negative, cytokeratin 7-positive): a distinct entity? |journal=Histopathology |volume=75 |issue=2 |pages=174–184 |date=August 2019 |pmid=30895640 |doi=10.1111/his.13865 |url=}}</ref> | |||
==Microscopic== | ==Microscopic== | ||
| Line 10: | Line 44: | ||
*Tubular or solid architecture. | *Tubular or solid architecture. | ||
*Edematous areas with loosly arranged cells. | *Edematous areas with loosly arranged cells. | ||
*Low [[ISUP nucleolar grade]] - grade 1 or 2. | |||
DDx: | DDx: | ||
*[[Renal oncocytoma]]. | *[[Renal oncocytoma]]. | ||
*[[Chromophobe renal cell carcinoma]]. | *[[Chromophobe renal cell carcinoma]]. | ||
*[[ | *[[Renal hybrid oncocytic/chromophobe tumour]]. | ||
*[[Renal cell carcinoma, unclassified]]. | |||
*[[Renal tumours with eosinophilic cytoplasm]]. | |||
===Images=== | |||
<gallery> | |||
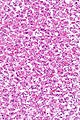
Image: Low grade oncocytic renal tumour -- low mag.jpg | LGORT - low mag. (WC) | |||
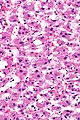
Image: Low grade oncocytic renal tumour -- intermed mag.jpg | LGORT - intermed. mag. (WC) | |||
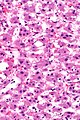
Image: Low grade oncocytic renal tumour - alt -- intermed mag.jpg | LGORT - intermed. mag. (WC) | |||
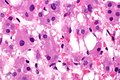
Image: Low grade oncocytic renal tumour -- high mag.jpg | LGORT - high mag. (WC) | |||
Image: Low grade oncocytic renal tumour - alt - high mag.jpg | LGORT - high mag. (WC) | |||
Image: Low grade oncocytic renal tumour -- very high mag.jpg | LGORT - high mag. (WC) | |||
</gallery> | |||
==IHC== | ==IHC== | ||
Features: | Features:<ref>{{cite journal |authors=Ricci C, Ambrosi F, Franceschini T, Giunchi F, Grillini A, Franchini E, Grillini M, Schiavina R, Massari F, Mollica V, Tateo V, Bianchi FM, Bianchi L, Droghetti M, Maloberti T, Tallini G, Colecchia M, Acosta AM, Lobo J, Trpkov K, Fiorentino M, de Biase D |title=Evaluation of an institutional series of low-grade oncocytic tumor (LOT) of the kidney and review of the mutational landscape of LOT |journal=Virchows Arch |volume= |issue= |pages= |date=October 2023 |pmid=37845471 |doi=10.1007/s00428-023-03673-9 |url=}}</ref> | ||
*CK7 +ve. | |||
*[[GATA3]] +ve. | |||
**GATA3 very rarely positive in RCCs (1/71 clear cell RCC, 0/53 papillary RCC, 2/33 chromophobe RCC).<ref name=pmid2431520>{{cite journal |authors=Gonzalez-Roibon N, Faraj SF, Munari E, Bezerra SM, Albadine R, Sharma R, Argani P, Allaf ME, Netto GJ |title=Comprehensive profile of GATA binding protein 3 immunohistochemical expression in primary and metastatic renal neoplasms |journal=Hum Pathol |volume=45 |issue=2 |pages=244–8 |date=February 2014 |pmid=24315206 |doi=10.1016/j.humpath.2013.08.020 |url=}}</ref> | |||
**GATA3 occasionally positive in [[renal oncocytoma]] (9/47 cases).<ref name=pmid2431520/> | |||
*PAX8 +ve. | |||
*CD117 -ve. | |||
Others: | |||
*CD10 -ve/+ve. | *CD10 -ve/+ve. | ||
*AMACR -ve/+ve. | *AMACR -ve/+ve. | ||
*CA9 -ve. | *CA9 -ve. | ||
*CK20 -ve. | *CK20 -ve. | ||
*CD10 -ve. | |||
*L1CAM +ve.<ref name=pmid38460672>{{cite journal |authors=Alghamdi M, Chen JF, Jungbluth A, Koutzaki S, Palmer MB, Al-Ahmadie HA, Fine SW, Gopalan A, Sarungbam J, Sirintrapun SJ, Tickoo SK, Reuter VE, Chen YB |title=L1CAM Expression and Molecular Alterations Distinguish Low Grade Oncocytic Tumor (LOT) from Eosinophilic Chromophobe Renal Cell Carcinoma |journal=Mod Pathol |volume= |issue= |pages=100467 |date=March 2024 |pmid=38460672 |doi=10.1016/j.modpat.2024.100467 |url=}}</ref> | |||
==Molecular== | |||
*[[Renal neoplasms with TSC/mTOR pathway mutations|TSC/mTOR pathway mutation]].<ref name=pmid35203531>{{cite journal |authors=Pivovarcikova K, Alaghehbandan R, Vanecek T, Ohashi R, Pitra T, Hes O |title=TSC/mTOR Pathway Mutation Associated Eosinophilic/Oncocytic Renal Neoplasms: A Heterogeneous Group of Tumors with Distinct Morphology, Immunohistochemical Profile, and Similar Genetic Background |journal=Biomedicines |volume=10 |issue=2 |pages= |date=January 2022 |pmid=35203531 |pmc=8869370 |doi=10.3390/biomedicines10020322 |url=}}</ref> | |||
==Sign out== | |||
<pre> | |||
Right Kidney Mass, Biopsy: | |||
- Low-grade oncocytic tumour (see comment). | |||
Comment: | |||
The tumour stains as follows: | |||
POSITIVE: CK7 (strong, diffuse), PAX8 (strong, diffuse), AE1/AE3, GATA-3 (moderate, diffuse). | |||
NEGATIVE: CD117, CD10, CK20, vimentin, CA9. | |||
It is in keeping with "low-grade oncocytic tumour" (LOT), an evolving entity. Based on limited data, LOT appears to have an indolent behavior. | |||
This tumour does not fit the diagnosis of renal oncocytoma or eosinophilic chromophobe renal cell carcinoma. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Renal oncocytoma]]. | *[[Renal oncocytoma]]. | ||
*[[Renal tumours with eosinophilic cytoplasm]]. | |||
==References== | ==References== | ||
{{Reflist| | {{Reflist|2}} | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Genitourinary pathology]] | [[Category:Genitourinary pathology]] | ||
Latest revision as of 12:37, 26 March 2024
| Low-grade oncocytic renal tumour | |
|---|---|
| Diagnosis in short | |
 Low-grade renal oncocytic tumour. H&E stain. | |
|
| |
| LM | abundant eosinophilic cytoplasm, nuclei uniform and round without significant pleomorphism, solid or tubular architecture |
| LM DDx | renal oncocytoma, chromophobe renal cell carcinoma eosinophilic variant, clear cell renal cell carcinoma eosinophilic variant, papillary renal cell carcinoma oncocytic variant, tubulocystic carcinoma of the kidney, other renal tumours with eosinophilic cytoplasm, benign liver |
| IHC | CK7 +ve, CD117 -ve, GATA3 +ve, PAX8 +ve |
| Molecular | TSC/mTOR pathway mutation |
| Grossing notes | partial nephrectomy grossing, total nephrectomy for tumour grossing |
| Site | kidney - see kidney tumours |
|
| |
| Clinical history | often incidentally discovered mass |
| Prognosis | likely benign |
| Clin. DDx | other kidney tumours |
Low-grade oncocytic renal tumour, abbreviated LOT, is an unusual renal tumour that does not neatly fit into any WHO renal neoplasia category. It is also known as renal oncocytic tumour that is CD117 negative and CK7 positive.
Low-grade oncocytic tumour directs to here.
Whether it is a distinct entity is not clear as of 2019.[1] It can be considered an emerging entity that may be in the WHO classification of renal neoplasia in the future.[2]
General
- Very rare.
- Benign behaviour based on a small series.[1]
Microscopic
Features:[3]
- Oncocytic cytoplasm.
- Round nuclei.
- Tubular or solid architecture.
- Edematous areas with loosly arranged cells.
- Low ISUP nucleolar grade - grade 1 or 2.
DDx:
- Renal oncocytoma.
- Chromophobe renal cell carcinoma.
- Renal hybrid oncocytic/chromophobe tumour.
- Renal cell carcinoma, unclassified.
- Renal tumours with eosinophilic cytoplasm.
Images
IHC
Features:[4]
- CK7 +ve.
- GATA3 +ve.
- GATA3 very rarely positive in RCCs (1/71 clear cell RCC, 0/53 papillary RCC, 2/33 chromophobe RCC).[5]
- GATA3 occasionally positive in renal oncocytoma (9/47 cases).[5]
- PAX8 +ve.
- CD117 -ve.
Others:
- CD10 -ve/+ve.
- AMACR -ve/+ve.
- CA9 -ve.
- CK20 -ve.
- CD10 -ve.
- L1CAM +ve.[6]
Molecular
Sign out
Right Kidney Mass, Biopsy: - Low-grade oncocytic tumour (see comment). Comment: The tumour stains as follows: POSITIVE: CK7 (strong, diffuse), PAX8 (strong, diffuse), AE1/AE3, GATA-3 (moderate, diffuse). NEGATIVE: CD117, CD10, CK20, vimentin, CA9. It is in keeping with "low-grade oncocytic tumour" (LOT), an evolving entity. Based on limited data, LOT appears to have an indolent behavior. This tumour does not fit the diagnosis of renal oncocytoma or eosinophilic chromophobe renal cell carcinoma.
See also
References
- ↑ 1.0 1.1 Trpkov K, Williamson SR, Gao Y, Martinek P, Cheng L, Sangoi AR, Yilmaz A, Wang C, San Miguel Fraile P, Perez Montiel DM, Bulimbasić S, Rogala J, Hes O (August 2019). "Low-grade oncocytic tumour of kidney (CD117-negative, cytokeratin 7-positive): a distinct entity?". Histopathology 75 (2): 174–184. doi:10.1111/his.13865. PMID 30895640.
- ↑ Siadat F, Trpkov K (January 2020). "ESC, ALK, HOT and LOT: Three Letter Acronyms of Emerging Renal Entities Knocking on the Door of the WHO Classification". Cancers (Basel) 12 (1). doi:10.3390/cancers12010168. PMC 7017067. PMID 31936678. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7017067/.
- ↑ Trpkov K, Williamson S, Martinek P, Cheng L, San Miguel Fraile P, Yilmaz A, Hes O, Oncocytic Renal Tumors with CD117 Negative, Cytokeratin 7 Positive Immunoprofile are Different from Eosinophilic Chromophobe Renal Cell Carcinoma (ChrRCC) and Oncocytoma. United States and Canadian Academy of Pathology Annual Meeting 2018.
- ↑ Ricci C, Ambrosi F, Franceschini T, Giunchi F, Grillini A, Franchini E, Grillini M, Schiavina R, Massari F, Mollica V, Tateo V, Bianchi FM, Bianchi L, Droghetti M, Maloberti T, Tallini G, Colecchia M, Acosta AM, Lobo J, Trpkov K, Fiorentino M, de Biase D (October 2023). "Evaluation of an institutional series of low-grade oncocytic tumor (LOT) of the kidney and review of the mutational landscape of LOT". Virchows Arch. doi:10.1007/s00428-023-03673-9. PMID 37845471.
- ↑ 5.0 5.1 Gonzalez-Roibon N, Faraj SF, Munari E, Bezerra SM, Albadine R, Sharma R, Argani P, Allaf ME, Netto GJ (February 2014). "Comprehensive profile of GATA binding protein 3 immunohistochemical expression in primary and metastatic renal neoplasms". Hum Pathol 45 (2): 244–8. doi:10.1016/j.humpath.2013.08.020. PMID 24315206.
- ↑ Alghamdi M, Chen JF, Jungbluth A, Koutzaki S, Palmer MB, Al-Ahmadie HA, Fine SW, Gopalan A, Sarungbam J, Sirintrapun SJ, Tickoo SK, Reuter VE, Chen YB (March 2024). "L1CAM Expression and Molecular Alterations Distinguish Low Grade Oncocytic Tumor (LOT) from Eosinophilic Chromophobe Renal Cell Carcinoma". Mod Pathol: 100467. doi:10.1016/j.modpat.2024.100467. PMID 38460672.
- ↑ Pivovarcikova K, Alaghehbandan R, Vanecek T, Ohashi R, Pitra T, Hes O (January 2022). "TSC/mTOR Pathway Mutation Associated Eosinophilic/Oncocytic Renal Neoplasms: A Heterogeneous Group of Tumors with Distinct Morphology, Immunohistochemical Profile, and Similar Genetic Background". Biomedicines 10 (2). doi:10.3390/biomedicines10020322. PMC 8869370. PMID 35203531. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8869370/.