Difference between revisions of "Juvenile xanthogranuloma"
Jump to navigation
Jump to search
m (touch) |
|||
| (7 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = Juvenile_xanthogranuloma_-_very_high_mag.jpg | | Image = Juvenile_xanthogranuloma_-_very_high_mag.jpg | ||
| Width = | | Width = | ||
| Caption = Juvenile xanthogranuloma. [[H&E stain]]. | | Caption = Juvenile xanthogranuloma. [[H&E stain]]. | ||
| Line 32: | Line 32: | ||
==General== | ==General== | ||
*Usually in children and infants, sometimes in adults.<ref name=Ref_Derm622>{{Ref Derm|622}}</ref> | *Usually in children and infants, sometimes in adults.<ref name=Ref_Derm622>{{Ref Derm|622}}</ref> | ||
**In adults, it may be referred to as ''cutaneous xanthogranuloma'',<ref name=pmid24801255>{{Cite journal | last1 = Chiang | first1 = E. | last2 = Lissner | first2 = G. | last3 = Bryar | first3 = PJ. | title = Unusual presentation of xanthogranuloma on the eyelid of an adult. | journal = Ophthal Plast Reconstr Surg | volume = 30 | issue = 6 | pages = e155-6 | month = | year = | doi = 10.1097/01.iop.0000440703.67932.37 | PMID = 24801255 }}</ref> ''adult onset xanthogranuloma'', and ''adult xanthogranuloma''.<ref name=pmid24154556>{{Cite journal | last1 = Tan | first1 = LC. | last2 = Tan | first2 = KB. | last3 = Aw | first3 = CW. | title = Unusual presentation of adult xanthogranuloma: a case report. | journal = Singapore Med J | volume = 55 | issue = 2 | pages = e25-7 | month = Feb | year = 2014 | doi = 10.11622/smedj.2013207 | PMID = 24154556 }}</ref> | |||
*Most common form of non–Langerhans cell histiocytosis.<ref name=emed_jxg>URL: [http://emedicine.medscape.com/article/1111629-diagnosis http://emedicine.medscape.com/article/1111629-diagnosis]. Accessed on: 3 February 2011.</ref> | *Most common form of non–Langerhans cell histiocytosis.<ref name=emed_jxg>URL: [http://emedicine.medscape.com/article/1111629-diagnosis http://emedicine.medscape.com/article/1111629-diagnosis]. Accessed on: 3 February 2011.</ref> | ||
*Can rarely be found in the brain.<ref>URL: [http://path.upmc.edu/cases/case245/dx.html http://path.upmc.edu/cases/case245/dx.html]. Accessed on: 13 January 2012.</ref> | *Can rarely be found in the brain.<ref>URL: [http://path.upmc.edu/cases/case245/dx.html http://path.upmc.edu/cases/case245/dx.html]. Accessed on: 13 January 2012.</ref> | ||
| Line 41: | Line 42: | ||
*+/-Touton [[giant cell]] - '''key feature'''. | *+/-Touton [[giant cell]] - '''key feature'''. | ||
**Large multi-nucleated cells where nuclei are distributed at the cell periphery. | **Large multi-nucleated cells where nuclei are distributed at the cell periphery. | ||
Notes: | |||
*Must prove they are non-Langerhans cell histiocytes, esp. if no Touton giant cells. | |||
DDx: | DDx: | ||
| Line 46: | Line 50: | ||
*[[Spitz nevus]] - uncommon; reported to have Touton cells.<ref name=pmid18312437>{{Cite journal | last1 = Guitart | first1 = J. | last2 = Gerami | first2 = P. | title = Touton-like giant cells in a Spitz's nevus. | journal = J Cutan Pathol | volume = 35 | issue = 7 | pages = 694-5 | month = Jul | year = 2008 | doi = 10.1111/j.1600-0560.2007.00877.x | PMID = 18312437 }}</ref> | *[[Spitz nevus]] - uncommon; reported to have Touton cells.<ref name=pmid18312437>{{Cite journal | last1 = Guitart | first1 = J. | last2 = Gerami | first2 = P. | title = Touton-like giant cells in a Spitz's nevus. | journal = J Cutan Pathol | volume = 35 | issue = 7 | pages = 694-5 | month = Jul | year = 2008 | doi = 10.1111/j.1600-0560.2007.00877.x | PMID = 18312437 }}</ref> | ||
*[[Dermatofibroma]], aneurysmal - has Touton [[giant cell]]s and hemosiderin deposition. | *[[Dermatofibroma]], aneurysmal - has Touton [[giant cell]]s and hemosiderin deposition. | ||
*[[Tuberculoma]]. | |||
*[[Erdheim-Chester disease]] - usu. [[BRAF V600E mutated]].<ref name=pmid22879539>{{Cite journal | last1 = Haroche | first1 = J. | last2 = Charlotte | first2 = F. | last3 = Arnaud | first3 = L. | last4 = von Deimling | first4 = A. | last5 = Hélias-Rodzewicz | first5 = Z. | last6 = Hervier | first6 = B. | last7 = Cohen-Aubart | first7 = F. | last8 = Launay | first8 = D. | last9 = Lesot | first9 = A. | title = High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. | journal = Blood | volume = 120 | issue = 13 | pages = 2700-3 | month = Sep | year = 2012 | doi = 10.1182/blood-2012-05-430140 | PMID = 22879539 }}</ref> | |||
* | *[[Rosai-Dorfman disease]] - Emperipolesis. | ||
*[[Necrobiotic xanthogranuloma]] - also may have Touton giant cells. | |||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
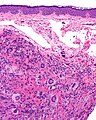
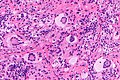
Image:Juvenile_xanthogranuloma_-_intermed_mag.jpg | Juvenile xanthogranuloma - intermed. mag. (WC) | Image:Juvenile_xanthogranuloma_-_intermed_mag.jpg | JXG - intermed. mag. (WC) | ||
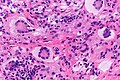
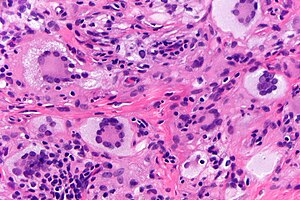
Image:Juvenile_xanthogranuloma_-_very_high_mag.jpg | Touton giant cells in a | Image:Juvenile xanthogranuloma - high mag.jpg | | JXG - intermed. mag. (WC) | ||
Image:Juvenile_xanthogranuloma_-_very_high_mag.jpg | Touton giant cells in a JXG - very high mag. (WC) | |||
</gallery> | </gallery> | ||
===IHC=== | ===IHC=== | ||
Features:<ref name=emed_jxg/> | Features:<ref name=emed_jxg/> | ||
Latest revision as of 20:37, 17 June 2016
| Juvenile xanthogranuloma | |
|---|---|
| Diagnosis in short | |
 Juvenile xanthogranuloma. H&E stain. | |
|
| |
| LM | dermal histiocytes with abundant cytoplasm, +/-Touton giant cells (large multi-nucleated cells where nuclei are distributed at the cell periphery) |
| LM DDx | Langerhans cell histiocytosis, Spitz nevus (reported to have Touton cells), Dermatofibroma - aneurysmal type |
| IHC | CD68 +ve, CD1a -ve, CD207 -ve |
| Site | skin |
|
| |
| Clinical history | usually in children and infants, sometimes in adults |
| Prognosis | benign |
Juvenile xanthogranuloma, abbreviated JXG, is a relatively common distinctive diagnosis in dermatopathology. It is also known as nevoxanthoendothelioma. In adults, it is called adult xanthogranuloma.[1]
General
- Usually in children and infants, sometimes in adults.[1]
- Most common form of non–Langerhans cell histiocytosis.[4]
- Can rarely be found in the brain.[5]
Microscopic
Features:[4]
- Dermal histiocytes:
- Abundant cytoplasm - may not be xanthomatous/foam cells.
- +/-Touton giant cell - key feature.
- Large multi-nucleated cells where nuclei are distributed at the cell periphery.
Notes:
- Must prove they are non-Langerhans cell histiocytes, esp. if no Touton giant cells.
DDx:
- Langerhans cell histiocytosis.
- Spitz nevus - uncommon; reported to have Touton cells.[6]
- Dermatofibroma, aneurysmal - has Touton giant cells and hemosiderin deposition.
- Tuberculoma.
- Erdheim-Chester disease - usu. BRAF V600E mutated.[7]
- Rosai-Dorfman disease - Emperipolesis.
- Necrobiotic xanthogranuloma - also may have Touton giant cells.
Images
IHC
Features:[4]
- Langerhans cell markers: CD1a, CD207 -- both should be negative.
- If Touton giant cells are absent -- this is essential.
- Histiocyte markers: CD68, CD163 -- both should be positive.
- Vimentin +ve.
Other markers:[8]
- CD4 +ve (21 of 27 cases).
- CD45 +ve (25 of 27 cases).
- Factor XIIIa +ve (25 of 27 cases).
Negatives:[9]
- Muscle markers: actin, desmin.
- Others: S100, factor VIII, cytokeratins.
Sign out
SKIN LESION, CHIN, BIOPSY: - JUVENILE XANTHOGRANULOMA.
See also
References
- ↑ 1.0 1.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 622. ISBN 978-0443066542.
- ↑ Chiang, E.; Lissner, G.; Bryar, PJ.. "Unusual presentation of xanthogranuloma on the eyelid of an adult.". Ophthal Plast Reconstr Surg 30 (6): e155-6. doi:10.1097/01.iop.0000440703.67932.37. PMID 24801255.
- ↑ Tan, LC.; Tan, KB.; Aw, CW. (Feb 2014). "Unusual presentation of adult xanthogranuloma: a case report.". Singapore Med J 55 (2): e25-7. doi:10.11622/smedj.2013207. PMID 24154556.
- ↑ 4.0 4.1 4.2 URL: http://emedicine.medscape.com/article/1111629-diagnosis. Accessed on: 3 February 2011.
- ↑ URL: http://path.upmc.edu/cases/case245/dx.html. Accessed on: 13 January 2012.
- ↑ Guitart, J.; Gerami, P. (Jul 2008). "Touton-like giant cells in a Spitz's nevus.". J Cutan Pathol 35 (7): 694-5. doi:10.1111/j.1600-0560.2007.00877.x. PMID 18312437.
- ↑ Haroche, J.; Charlotte, F.; Arnaud, L.; von Deimling, A.; Hélias-Rodzewicz, Z.; Hervier, B.; Cohen-Aubart, F.; Launay, D. et al. (Sep 2012). "High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses.". Blood 120 (13): 2700-3. doi:10.1182/blood-2012-05-430140. PMID 22879539.
- ↑ Kraus, MD.; Haley, JC.; Ruiz, R.; Essary, L.; Moran, CA.; Fletcher, CD. (Apr 2001). "Juvenile xanthogranuloma: an immunophenotypic study with a reappraisal of histogenesis.". Am J Dermatopathol 23 (2): 104-11. PMID 11285404.
- ↑ Thomas DB, Sidler AK, Huston BM (October 1998). "Radiological case of the month. Juvenile xanthogranuloma". Arch Pediatr Adolesc Med 152 (10): 1029–30. PMID 9790615. http://archpedi.ama-assn.org/cgi/content/full/152/10/1029.