Difference between revisions of "Juvenile xanthogranuloma"
Jump to navigation
Jump to search
m (touch) |
(→Images: +image) |
||
| Line 52: | Line 52: | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
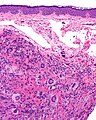
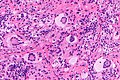
Image:Juvenile_xanthogranuloma_-_intermed_mag.jpg | Juvenile xanthogranuloma - intermed. mag. (WC) | Image:Juvenile_xanthogranuloma_-_intermed_mag.jpg | JXG - intermed. mag. (WC) | ||
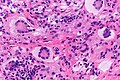
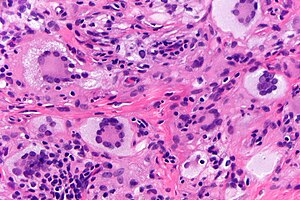
Image:Juvenile_xanthogranuloma_-_very_high_mag.jpg | Touton giant cells in a | Image:Juvenile xanthogranuloma - high mag.jpg | | JXG - intermed. mag. (WC) | ||
Image:Juvenile_xanthogranuloma_-_very_high_mag.jpg | Touton giant cells in a JXG - very high mag. (WC) | |||
</gallery> | </gallery> | ||
===IHC=== | ===IHC=== | ||
Features:<ref name=emed_jxg/> | Features:<ref name=emed_jxg/> | ||
Revision as of 04:18, 1 March 2015
| Juvenile xanthogranuloma | |
|---|---|
| Diagnosis in short | |
 Juvenile xanthogranuloma. H&E stain. | |
|
| |
| LM | dermal histiocytes with abundant cytoplasm, +/-Touton giant cells (large multi-nucleated cells where nuclei are distributed at the cell periphery) |
| LM DDx | Langerhans cell histiocytosis, Spitz nevus (reported to have Touton cells), Dermatofibroma - aneurysmal type |
| IHC | CD68 +ve, CD1a -ve, CD207 -ve |
| Site | skin |
|
| |
| Clinical history | usually in children and infants, sometimes in adults |
| Prognosis | benign |
Juvenile xanthogranuloma, abbreviated JXG, is a relatively common distinctive diagnosis in dermatopathology. It is also known as nevoxanthoendothelioma. In adults, it is called adult xanthogranuloma.[1]
General
- Usually in children and infants, sometimes in adults.[1]
- Most common form of non–Langerhans cell histiocytosis.[2]
- Can rarely be found in the brain.[3]
Microscopic
Features:[2]
- Dermal histiocytes:
- Abundant cytoplasm - may not be xanthomatous/foam cells.
- +/-Touton giant cell - key feature.
- Large multi-nucleated cells where nuclei are distributed at the cell periphery.
DDx:
- Langerhans cell histiocytosis.
- Spitz nevus - uncommon; reported to have Touton cells.[4]
- Dermatofibroma, aneurysmal - has Touton giant cells and hemosiderin deposition.
Notes:
- Must prove they are non-Langerhans cell histiocytes, esp. if no Touton giant cells.
Images
IHC
Features:[2]
- Langerhans cell markers: CD1a, CD207 -- both should be negative.
- If Touton giant cells are absent -- this is essential.
- Histiocyte markers: CD68, CD163 -- both should be positive.
- Vimentin +ve.
Other markers:[5]
- CD4 +ve (21 of 27 cases).
- CD45 +ve (25 of 27 cases).
- Factor XIIIa +ve (25 of 27 cases).
Negatives:[6]
- Muscle markers: actin, desmin.
- Others: S100, factor VIII, cytokeratins.
Sign out
SKIN LESION, CHIN, BIOPSY: - JUVENILE XANTHOGRANULOMA.
See also
References
- ↑ 1.0 1.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 622. ISBN 978-0443066542.
- ↑ 2.0 2.1 2.2 URL: http://emedicine.medscape.com/article/1111629-diagnosis. Accessed on: 3 February 2011.
- ↑ URL: http://path.upmc.edu/cases/case245/dx.html. Accessed on: 13 January 2012.
- ↑ Guitart, J.; Gerami, P. (Jul 2008). "Touton-like giant cells in a Spitz's nevus.". J Cutan Pathol 35 (7): 694-5. doi:10.1111/j.1600-0560.2007.00877.x. PMID 18312437.
- ↑ Kraus, MD.; Haley, JC.; Ruiz, R.; Essary, L.; Moran, CA.; Fletcher, CD. (Apr 2001). "Juvenile xanthogranuloma: an immunophenotypic study with a reappraisal of histogenesis.". Am J Dermatopathol 23 (2): 104-11. PMID 11285404.
- ↑ Thomas DB, Sidler AK, Huston BM (October 1998). "Radiological case of the month. Juvenile xanthogranuloma". Arch Pediatr Adolesc Med 152 (10): 1029–30. PMID 9790615. http://archpedi.ama-assn.org/cgi/content/full/152/10/1029.