Difference between revisions of "Juvenile granulosa cell tumour"
Jump to navigation
Jump to search
(→IHC) |
(→Images: added a case) |
||
| (5 intermediate revisions by one other user not shown) | |||
| Line 3: | Line 3: | ||
| Image = Juvenile_granulosa_cell_tumour_-_very_high_mag.jpg | | Image = Juvenile_granulosa_cell_tumour_-_very_high_mag.jpg | ||
| Width = | | Width = | ||
| Caption = Juvenile granulosa cell tumour. [[H&E stain]]. | | Caption = Juvenile granulosa cell tumour. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = microcystic spaces, cuboidal-to-polygonal cells in sheets or stands or cords, with moderate-to-marked nuclear atypia, and basophilic cytoplasm | | Micro = microcystic spaces, cuboidal-to-polygonal cells in sheets or stands or cords, with moderate-to-marked nuclear atypia, and basophilic cytoplasm | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[Brenner tumour]] | | LMDDx = [[Brenner tumour]], [[small cell carcinoma of hypercalcemic type]] | ||
| Stains = | | Stains = | ||
| IHC = inhibin +ve, calretinin +ve | | IHC = inhibin +ve, calretinin +ve | ||
| Line 59: | Line 59: | ||
DDx: | DDx: | ||
*[[Brenner tumour]]. | *[[Brenner tumour]]. | ||
*[[Adult granulosa cell tumour]]. | |||
*[[Small cell carcinoma of hypercalcemic type]].<ref name=pmid21993272>{{Cite journal | last1 = Bárcena | first1 = C. | last2 = Oliva | first2 = E. | title = WT1 expression in the female genital tract. | journal = Adv Anat Pathol | volume = 18 | issue = 6 | pages = 454-65 | month = Nov | year = 2011 | doi = 10.1097/PAP.0b013e318234aaed | PMID = 21993272 }}</ref> | |||
===Images=== | ===Images=== | ||
| Line 66: | Line 68: | ||
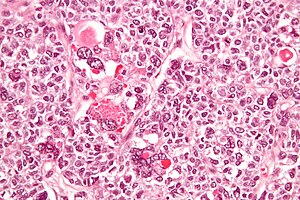
Image:Juvenile_granulosa_cell_tumour_-_very_high_mag.jpg | Juvenile granulosa cell tumour - very high mag. (WC) | Image:Juvenile_granulosa_cell_tumour_-_very_high_mag.jpg | Juvenile granulosa cell tumour - very high mag. (WC) | ||
</gallery> | </gallery> | ||
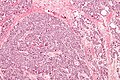
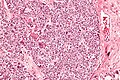
[[File:3 13627319654987 sl 1.png| Juvenile granulosa cell tumor]] | |||
[[File:3 13627319654987 sl 2.png| Juvenile granulosa cell tumor]] | |||
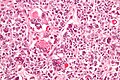
[[File:3 13627319654987 sl 3.png| Juvenile granulosa cell tumor]] | |||
[[File:3 13627319654987 sl 4.png| Juvenile granulosa cell tumor]] | |||
Juvenile granulosa cell tumor of ovary of child. A. A pink tumor shows cyst-like areas with occasional nodules at low power. B. Tumor cells haphazardly spread without longitudinal grooves, with small nucleoli, in an edematous background. C. The cysts are in fact follicles, some producing, as here, the typical basophilic fluid. D. In some regions, abundant pink cytoplasm is obvious. | |||
==IHC== | ==IHC== | ||
Latest revision as of 17:43, 2 January 2017
| Juvenile granulosa cell tumour | |
|---|---|
| Diagnosis in short | |
 Juvenile granulosa cell tumour. H&E stain. | |
|
| |
| LM | microcystic spaces, cuboidal-to-polygonal cells in sheets or stands or cords, with moderate-to-marked nuclear atypia, and basophilic cytoplasm |
| LM DDx | Brenner tumour, small cell carcinoma of hypercalcemic type |
| IHC | inhibin +ve, calretinin +ve |
| Molecular | trisomy 12 |
| Gross | mass lesion, solid |
| Site | ovary - ovarian tumours |
|
| |
| Associated Dx | endometrial hyperplasia, endometrioid endometrial carcinoma |
| Symptoms | +/-menorrhagia |
| Prevalence | uncommon |
| Prognosis | good to moderate (dependent on stage) |
| Treatment | surgery |
Juvenile granulosa cell tumour is an uncommon ovarian tumour in the sex cord stromal tumours group.
General
May secrete estrogen - can present with:
- Endometrial pathology, e.g. endometrial hyperplasia or endometrioid endometrial carcinoma.
- Precocious puberty.[3]
Prognosis - granulosa cell tumours (adult and juvenile):[1]
- Low-stage: 97% five year survival.
- High-stage: 67% five year survival.
Gross
- Classically solid.
Microscopic
Features:
- Microcystic spaces.
- Moderate-to-marked nuclear atypia.
- Cuboidal-to-polygonal cell in sheets or stands or cords.
- Basophilic cytoplasm.
Notes:
- Juvenile variant of GCT has more nuclear pleomorphism.
DDx:
Images


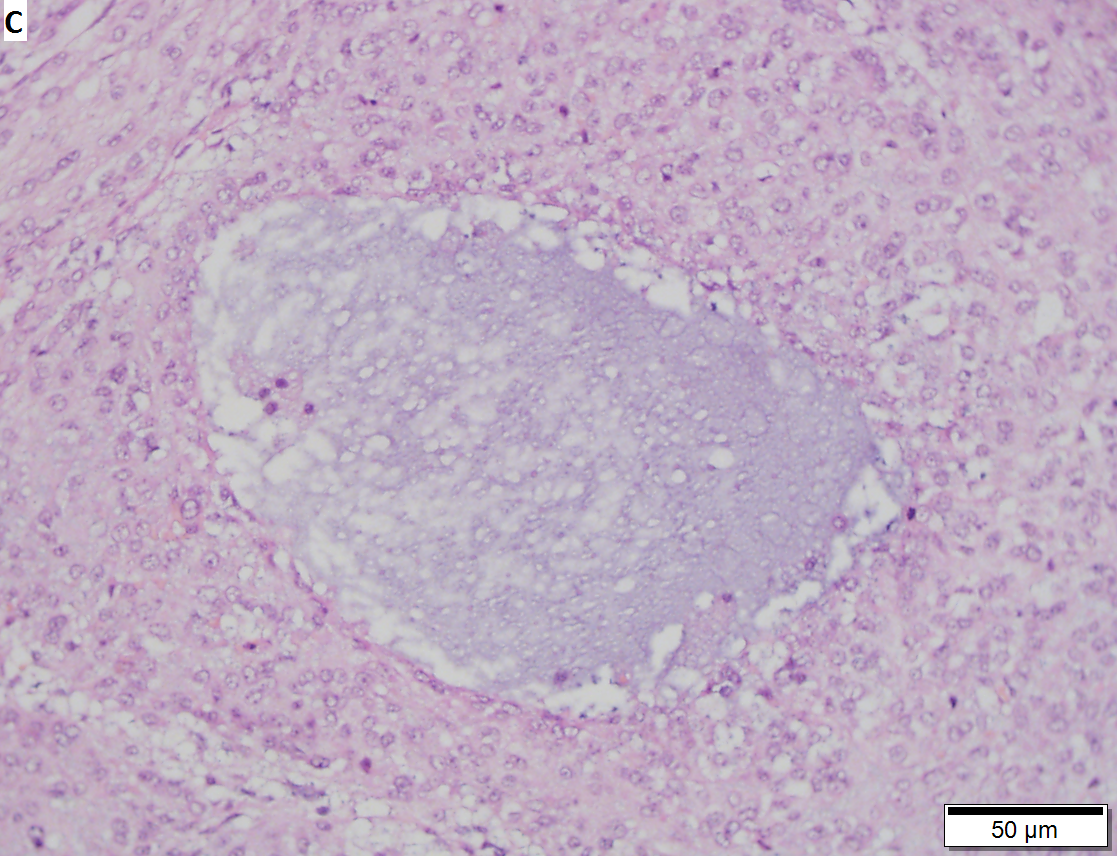
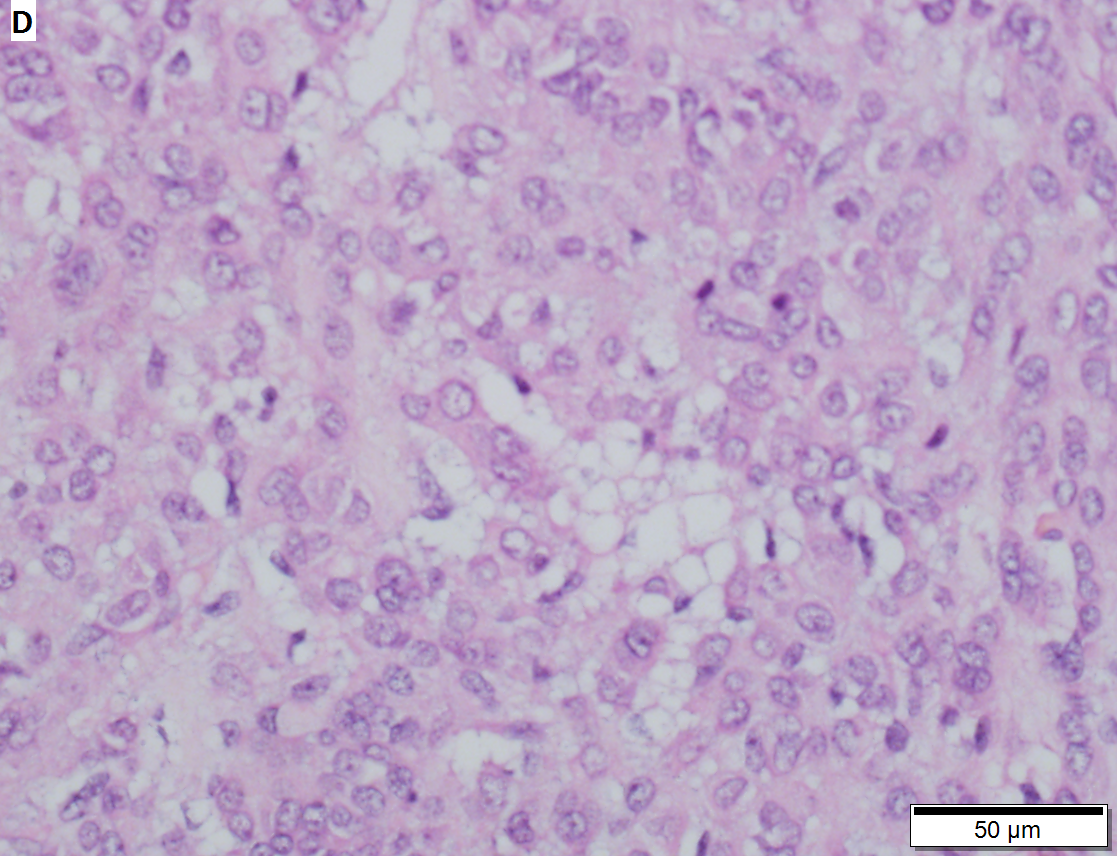 Juvenile granulosa cell tumor of ovary of child. A. A pink tumor shows cyst-like areas with occasional nodules at low power. B. Tumor cells haphazardly spread without longitudinal grooves, with small nucleoli, in an edematous background. C. The cysts are in fact follicles, some producing, as here, the typical basophilic fluid. D. In some regions, abundant pink cytoplasm is obvious.
Juvenile granulosa cell tumor of ovary of child. A. A pink tumor shows cyst-like areas with occasional nodules at low power. B. Tumor cells haphazardly spread without longitudinal grooves, with small nucleoli, in an edematous background. C. The cysts are in fact follicles, some producing, as here, the typical basophilic fluid. D. In some regions, abundant pink cytoplasm is obvious.
IHC
- Inhibin positive.[5]
- Inhibin negative in Brenner tumour.
- Calretinin +ve.
- Ki-67 <5% (12/12 cases[6]).
- CD34 -ve (0 +ve/12 cases[6]).
- Vimentin +ve (11 +ve/12 cases[6]).
- CD99 +ve.[7]
Molecular
- Currently not used for the diagnosis.
See also
References
- ↑ 1.0 1.1 Oztekin, D.; Kurt, S.; Camuzcuoglu, H.; Balsak, D.; Dicle, N.; Tinar, S.. "Granulosa cell tumors of the ovary: review of 43 cases.". J BUON 17 (3): 461-4. PMID 23033282.
- ↑ URL: http://path.upmc.edu/cases/case631.html. Accessed on: 26 January 2012.
- ↑ Hashemipour, M.; Moaddab, MH.; Nazem, M.; Mahzouni, P.; Salek, M. (Jul 2010). "Granulosa cell tumor in a six-year-old girl presented as precocious puberty.". J Res Med Sci 15 (4): 240-2. PMID 21526089.
- ↑ Bárcena, C.; Oliva, E. (Nov 2011). "WT1 expression in the female genital tract.". Adv Anat Pathol 18 (6): 454-65. doi:10.1097/PAP.0b013e318234aaed. PMID 21993272.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1102. ISBN 0-7216-0187-1.
- ↑ 6.0 6.1 6.2 Kondi-Pafiti, A.; Grapsa, D.; Kairi-Vassilatou, E.; Carvounis, E.; Hasiakos, D.; Kontogianni, K.; Fotiou, S. (2010). "Granulosa cell tumors of the ovary: a clinicopathologic and immunohistochemical study of 21 cases.". Eur J Gynaecol Oncol 31 (1): 94-8. PMID 20349790.
- ↑ Schmidt, D.; Kommoss, F. (May 2007). "[Diagnosis and differential diagnosis of granulosa cell tumor].". Pathologe 28 (3): 195-202. doi:10.1007/s00292-007-0908-8. PMID 17387475.
- ↑ Schofield, DE.; Fletcher, JA. (Dec 1992). "Trisomy 12 in pediatric granulosa-stromal cell tumors. Demonstration by a modified method of fluorescence in situ hybridization on paraffin-embedded material.". Am J Pathol 141 (6): 1265-9. PMID 1466394.
- ↑ Mayr, D.; Kaltz-Wittmer, C.; Arbogast, S.; Amann, G.; Aust, DE.; Diebold, J. (Sep 2002). "Characteristic pattern of genetic aberrations in ovarian granulosa cell tumors.". Mod Pathol 15 (9): 951-7. doi:10.1097/01.MP.0000024290.55261.14. PMID 12218213.