Difference between revisions of "Gastroesophageal reflux disease"
Jump to navigation
Jump to search
| Line 65: | Line 65: | ||
#+/-Intraepithelial edema. | #+/-Intraepithelial edema. | ||
#+/-Apoptotic cells.<ref name=pmid9926792>{{cite journal |author=Wetscher GJ, Schwelberger H, Unger A, ''et al.'' |title=Reflux-induced apoptosis of the esophageal mucosa is inhibited in Barrett's epithelium |journal=Am. J. Surg. |volume=176 |issue=6 |pages=569–73 |year=1998 |month=December |pmid=9926792 |doi= |url=}}</ref> | #+/-Apoptotic cells.<ref name=pmid9926792>{{cite journal |author=Wetscher GJ, Schwelberger H, Unger A, ''et al.'' |title=Reflux-induced apoptosis of the esophageal mucosa is inhibited in Barrett's epithelium |journal=Am. J. Surg. |volume=176 |issue=6 |pages=569–73 |year=1998 |month=December |pmid=9926792 |doi= |url=}}</ref> | ||
#+/-Glycogen - cytoplasm cleared (white). | |||
Notes: | Notes: | ||
| Line 76: | Line 77: | ||
*[[Barrett's esophagus]] - intestinal metaplasia may be minimal. | *[[Barrett's esophagus]] - intestinal metaplasia may be minimal. | ||
Images: | ===Images=== | ||
<gallery> | |||
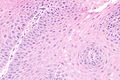
Image: Gastroesophageal reflux disease -- low mag.jpg | GERD - low mag. | |||
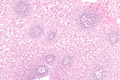
Image: Gastroesophageal reflux disease -- intermed mag.jpg | GERD - intermed. mag. | |||
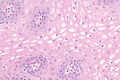
Image: Gastroesophageal reflux disease -- high mag.jpg | GERD - high mag. | |||
Image: Gastroesophageal reflux disease - glycogen -- intermed mag.jpg | GERD - intermed. mag. | |||
Image: Gastroesophageal reflux disease - glycogen -- high mag.jpg | GERD - high mag. | |||
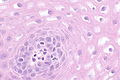
Image: Gastroesophageal reflux disease - glycogen -- very high mag.jpg | GERD - high mag. | |||
</gallery> | |||
www: | |||
*[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860>{{Cite journal | last1 = Genevay | first1 = M. | last2 = Rubbia-Brandt | first2 = L. | last3 = Rougemont | first3 = AL. | title = Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease? | journal = Arch Pathol Lab Med | volume = 134 | issue = 6 | pages = 815-25 | month = Jun | year = 2010 | doi = 10.1043/1543-2165-134.6.815 | PMID = 20524860 }}</ref> | *[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860>{{Cite journal | last1 = Genevay | first1 = M. | last2 = Rubbia-Brandt | first2 = L. | last3 = Rougemont | first3 = AL. | title = Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease? | journal = Arch Pathol Lab Med | volume = 134 | issue = 6 | pages = 815-25 | month = Jun | year = 2010 | doi = 10.1043/1543-2165-134.6.815 | PMID = 20524860 }}</ref> | ||
Revision as of 03:02, 14 June 2014
| Gastroesophageal reflux disease | |
|---|---|
| Diagnosis in short | |
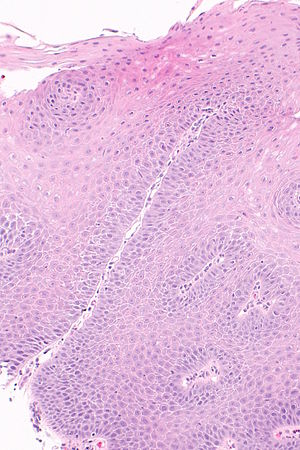 Micrograph showing histology compatible with gastroesophageal reflux disease. H&E stain. | |
|
| |
| LM | basal cell hyperplasia (> 3 cells thick or >15% of epithelial thickness), papillae elongated (papillae reach into the top 1/3 of the epithelial layer), inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells"), +/-intraepithelial edema, +/-Apoptotic cells |
| LM DDx | intestinal metaplasia (Barrett's esophagus), eosinophilic esophagitis, acute esophagitis |
| Site | esophagus |
|
| |
| Associated Dx | obesity, Barrett's esophagus |
| Prevalence | common |
| Endoscopy | erythema, erosions, +/-ulceration. |
| Prognosis | benign |
| Clin. DDx | eosinophilic esophagitis, acute esophagitis |
| Treatment | proton pump inhibitors |
Gastroesophageal reflux disease, abbreviated GERD, is a common pathology of the esophagus. It is occasionally abbreviated GORD (gastro-oesophageal reflux disease).
Reflux esophagitis redirects here. It technically isn't a synonym.[1][2]
General
Clinical:
- Usually chest pain
- +/-Abdominal pain.
- +/-Vomiting.
- +/-Blood loss.
Treatment:
- Treated with proton pump inhibitors (PPIs).
DDx (clinical):
Gross
- Erythema.
- Erosions.
- +/-Ulceration.
Note:
- Many be graded using Savary-Miller classification.
Images:
Microscopic
Features:
- Basal cell hyperplasia;[3] > 3 cells thick or >15% of epithelial thickness.
- Papillae elongated; papillae reach into the top 1/3 of the epithelial layer.[4]
- Inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells").
- +/-Intraepithelial edema.
- +/-Apoptotic cells.[5]
- +/-Glycogen - cytoplasm cleared (white).
Notes:
- Intraepithelial cells with irregular nuclear contours, "squiggle cells" (T lymphocytes[6]), may mimic neutrophils.
- Changes may be focal.
- PPI effect may be seen in a concurrent gastric biopsy.
- Perinuclear clearing may be seen.[7]
DDx:
- Eosinophilic esophagitis - characterized by similar histomorphologic features. The key difference is: more eosinophils.
- Barrett's esophagus - intestinal metaplasia may be minimal.
Images
www:
Sign out
Poorly oriented
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX.
Columnar epithelium present
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ulceration present
ESOPHAGUS, DISTAL, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA, RARE INTRAEPITHELIAL EOSINOPHILS AND EVIDENCE OF ULCERATION -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: PAS-D staining is negative for microorganisms.
BE and GERD present
ESOPHAGUS (DISTAL), BIOPSY: - COLUMNAR EPITHELIUM WITH INTESTINAL METAPLASIA AND MODERATE CHRONIC INFLAMMATION, SEE COMMENT. - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
See also
References
- ↑ Orbelo, DM.; Enders, FT.; Romero, Y.; Francis, DL.; Achem, SR.; Dabade, TS.; Crowell, MD.; Geno, DM. et al. (Jan 2014). "Once-Daily Omeprazole/Sodium Bicarbonate Heals Severe Refractory Reflux Esophagitis with Morning or Nighttime Dosing.". Dig Dis Sci. doi:10.1007/s10620-013-3017-y. PMID 24448652.
- ↑ Karbasi, A.; Ardestani, ME.; Ghanei, M.; Harandi, AA. (Jun 2013). "The association between reflux esophagitis and airway hyper-reactivity in patients with gastro-esophageal reflux.". J Res Med Sci 18 (6): 473-6. PMID 24250694.
- ↑ Steiner, SJ.; Kernek, KM.; Fitzgerald, JF. (May 2006). "Severity of basal cell hyperplasia differs in reflux versus eosinophilic esophagitis.". J Pediatr Gastroenterol Nutr 42 (5): 506-9. doi:10.1097/01.mpg.0000221906.06899.1b. PMID 16707971.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 804. ISBN 0-7216-0187-1.
- ↑ Wetscher GJ, Schwelberger H, Unger A, et al. (December 1998). "Reflux-induced apoptosis of the esophageal mucosa is inhibited in Barrett's epithelium". Am. J. Surg. 176 (6): 569–73. PMID 9926792.
- ↑ Cucchiara, S.; D'Armiento, F.; Alfieri, E.; Insabato, L.; Minella, R.; De Magistris, TM.; Scoppa, A. (Nov 1995). "Intraepithelial cells with irregular nuclear contours as a marker of esophagitis in children with gastroesophageal reflux disease.". Dig Dis Sci 40 (11): 2305-11. PMID 7587806.
- ↑ URL: http://155.37.5.42/eAtlas/GI/1262.htm. Accessed on: 31 January 2014.
- ↑ Genevay, M.; Rubbia-Brandt, L.; Rougemont, AL. (Jun 2010). "Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease?". Arch Pathol Lab Med 134 (6): 815-25. doi:10.1043/1543-2165-134.6.815. PMID 20524860.